Cockett’s Syndrome
Chaymae Faraj*, Kaoutar Imrani, Sara Essetti, Chaimae Lahlou, Nourelhouda Bahlouli, Nabil Moatassim Billah and Ittimade Nassar
Department of Radiology, Ibn Sina Hospital, Faculty of medicine and pharmacy, Mohammed V University, Morocco
Received Date: 13/08/2024; Published Date: 23/10/2024
*Corresponding author: Chaymae Faraj, Department of Radiology, Ibn Sina Hospital, Faculty of medicine and pharmacy, Mohammed V University, Rabat, Morocco
May-Thurner Syndrome (MTS), also known as ilio-caval compression syndrome or iliac vein compression syndrome or Cockett syndrome is a clinical condition resulting from compression of the ilio-caval anatomical unit against the underlying bone by the overlying arterial system.
The most common lesion is the compression of the left common iliac vein (LCIV) between the overlying Right Common Iliac Artery (RCIA) and the fifth lumbar vertebra [1].
Though not exclusive to this demographic, MTS typically affects women in their third to fifth decades of life. Venous hypertension is the most typical manifestation of these patients. Patients may present with acute episodic (activity related) heaviness and swelling of left lower limb or venous claudication which is relieved with rest and leg elevation. This develops into chronic venous insufficiency, which manifests as varicose veins, pigmentation in the legs, or venous ulcers [2]. Sometimes, the first presentation may be that of deep vein thrombosis with painful left lower limb swelling. There may be no precipitating cause or the disease may first present during or after pregnancy [3].
When a lower limb swells unilaterally, a venous duplex ultrasonography of the affected limb is sometimes used to help with the physical examination.Color Doppler ultrasound is a useful tool for evaluating varicose veins, venous incompetence, and diagnosing deep vein thrombosis; however, it is not sensitive enough to investigate the pelvic veins, particularly the ilio-caval region [1].
In the appropriate clinical context, cross-sectional imaging is required to assess the ilio-caval area and locate the stenotic lesion if MTS is suspected. Two great imaging modalities to detect MT architecture and show the presence of collaterals are magnetic resonance (MR) venography and multidetector computed tomography (MDCT) venography. For the diagnosis of MTS, CT and MR venography both show sensitivity and specificity of over 95% [4].
MDCT venography demonstrates the compression of the LCIV by the RCIA, presence of bony spurs, deep vein thrombosis, and pelvic venous collaterals and helps rule out other compressive pathologies [1].
MR venography is described as the imaging technique of choice, but is underused. it could easily depict the area of compression or obstruction and documents the presence of collaterals [5].
When assessing left lower limb deep vein thrombosis, MTS should be taken into account as it is an underdiagnosed condition. In the appropriate clinical context, a low threshold for cross-sectional imaging, such as MDCT venography and MR venography, should be maintained.
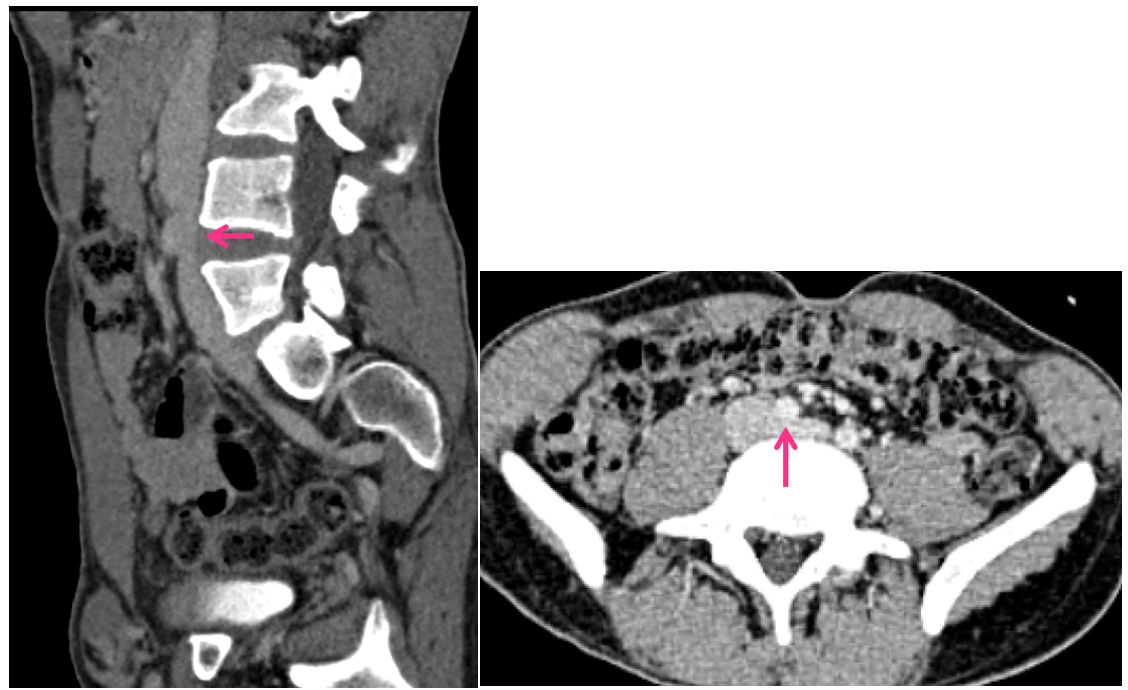
Figure 1: CT scan showing the compression of the left iliac vein by the right common iliac artery.
References
- Poyyamoli S, Mehta P, Cherian M, Anand RR, Patil SB, Kalva S, et al. May-Thurner syndrome. Cardiovasc Diagn Ther, 2021; 11(5): 1104-1111. doi: 10.21037/cdt.2020.03.07.
- Eberhardt RT, Raffetto JD. Chronic venous insufficiency. Circulation, 2005; 111: 2398-409.
- Oguzkurt L, Ozkan U, Ulusan S, et al. Compression of the left common iliac vein in asymptomatic subjects and patients with left iliofemoral deep vein thrombosis. J Vasc Interv Radiol, 2008; 19: 366-70; quiz 371.
- Wolpert LM, Rahmani O, Stein B, et al. Magnetic resonance venography in the diagnosis and management of May-Thurner syndrome. Vasc Endovascular Surg, 2002; 36: 51-57.
- Wolpert LM, Rahmani O, Stein B, et al. Magnetic resonance venography in the diagnosis and management of May–Thurner syndrome. Vasc Endovasc Surg, 2002; 36: 51–57.

