Guillain-Barré Syndrome on MRI: An Image to Remember
Yahya El Harras*, Safaa Choayb, Nazik Allali, Latifa Chat and Siham El Haddad
Department of Pediatric and Gynecology Radiology, Children’s Hospital, University Mohammed V, Rabat, Morocco
Received Date: 19/04/2023; Published Date: 01/08/2023
*Corresponding author: Yahya El Harras, Department of Pediatric and Gynecology Radiology, Children’s Hospital, University Mohammed V, Rabat, Morocco
Guillain-Barré Syndrome (GBS) is an Acute Inflammatory Demyelinating Polyradiculoneuropathy (AIDP), which corresponds to a group of acute-onset disorders involving sensory, motor, and autonomic nerves [1]. A recent event or “trigger” is found in 70% of cases such as upper respiratory tract infections or diarrhoea one to three weeks before their onset, caused in most cases by Campylobacter jejuni. Nowadays, we rather talk about the Guillain- Barré spectrum Disorders which includes several subtypes such as AIDP (being its most common form), axonal subtypes and Miller Fisher variant which is characterized by ataxia, ophthalmoplegia, and areflexia without weakness [2]. Through our image article, we highlight the Guillain-Barré syndrome or AIDP in particular with its key findings on MRI. It generally affects children and young adults with a generally more favorable prognosis in children.
Clinical examination typically finds rapidly progressive, symmetrical and ascending muscle paresis or paralysis with hyporeflexia and variable sensory involvement frequently present. The cranial nerves are affected in 30 to 40% of cases with facial and oropharyngeal muscles being deficient in 50% of patients with the most severe form of the disease (when the ascending paralysis attends the brainstem) [1].
Combining clinical presentation, CSF study, and electrophysiological findings usually confirms the diagnosis. CSF abnormalities are an increased protein without pleocytosis. As for nerve conduction abnormalities, we can find slow or blocked nerve conduction or a prolongation of distal latency [3].
As for imaging findings, we are requested to exclude other causes or in patients where nerve conduction studies and CSF examination are questionable. It is based on spine MRI as it helps in excluding compressive causes of polyradiculopathy. T1-WI before and after Gadolinium administration both sagittal and coronal are the most useful sequences [4]. It typically finds surface thickening and contrast enhancement on the conus medullaris as well as the nerve roots of the cauda equina (Figure 1). Most commonly, it enhances the anterior nerve roots. However, posterior nerve roots enhancement can also be found [1].
Differential diagnosis may include arachnoiditis especially postoperative, or post intrathecal injection, leptomeningeal carcinomatosis (which has typically a more nodular aspect) or even hereditary polyneuropathies such as Charcot Marie Tooth [1]. The latter has some specific clinical findings (especially muscle atrophy) as well as imaging aspects which differentiates from GBS by the hypertrophy of the roots of the cauda equina and plexuses, responsible of cauda equina syndrome in some cases.
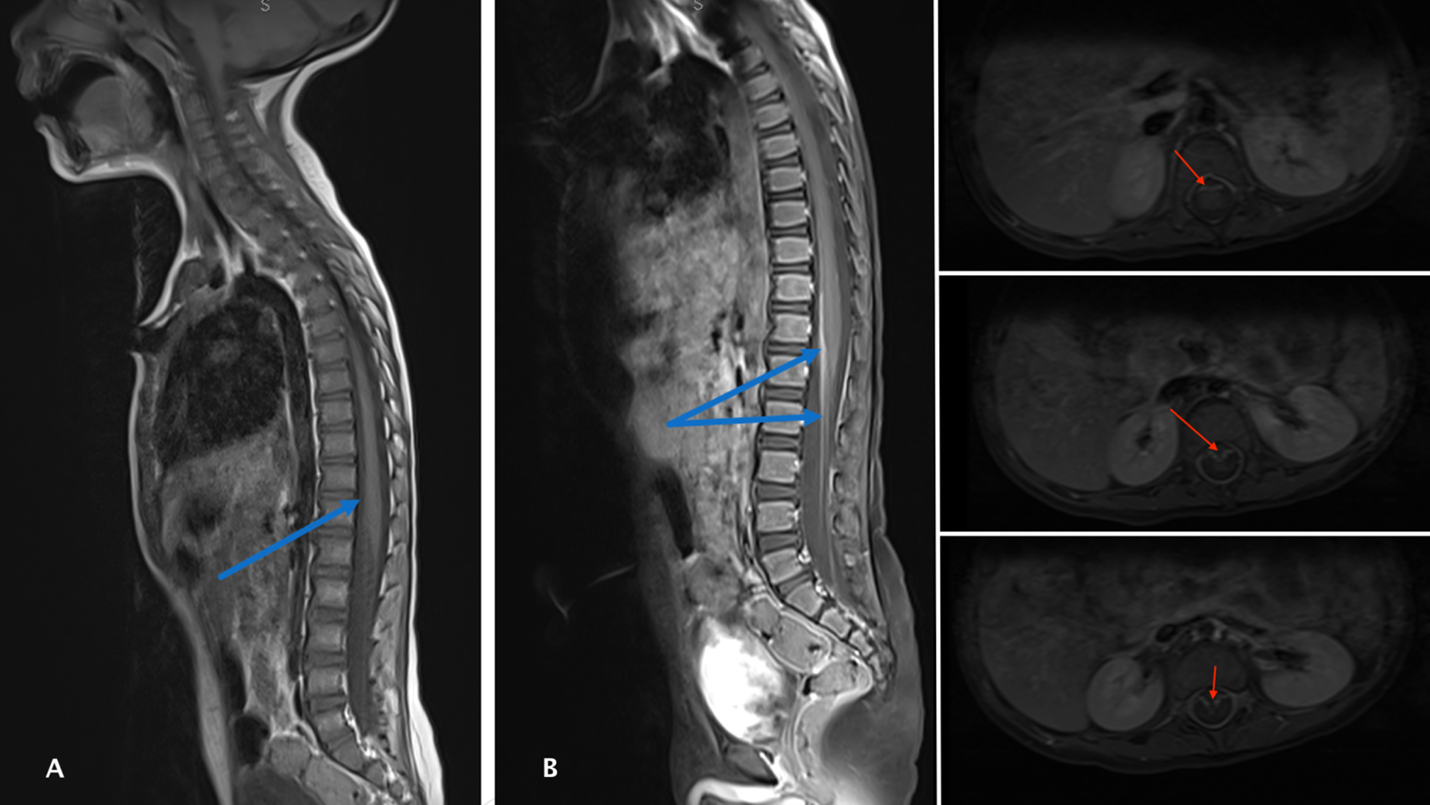
Figure: Spine MRI of our 4-year-old boy with no history, consulting for acute, ascending and symmetrical muscular weakness. Reduced osteo-tendinous reflexes were found on examination. CSF analysis revealed hyperproteinorrachia without pleocytosis. Sagittal T1 (A and B) shows bulging of the conus medullaris enhanced on the anterior side after Gadolinium as well as anterior nerve roots enhancement of the cauda equina. Note the anterior enhancement on axial images (red arrows).
References
- Li Hf, Ji Xj. The Diagnostic, Prognostic, and Differential Value of Enhanced MR Imaging in Guillain-Barré Syndrome. AJNR Am J Neuroradiol, 2011; 32(7): E140‑E140.
- Ralapanawa U, Kumarihamy P, Jayalath T, Udupihille J. Guillain-Barré syndrome with associated unilateral ptosis without ophthalmoplegia – a rare presentation: a case report and review of the literature. J Med Case Reports, 2019; 13(1): 221.
- Uncini A, Kuwabara S. Electrodiagnostic criteria for Guillain–Barrè syndrome: A critical revision and the need for an update. Clinical Neurophysiology, 2012; 123(8): 1487‑1495.
- Baraldés-Rovira M, Paul M, Gallego Y, Gil MI, Vicandi C, Vicente-Pascual M. Usefulness of magnetic resonance imaging in the diagnosis of Guillain Barré syndrome. Neurología, 2022; 37(9): 816‑818.

