Exuberant Gastric Distension
Joana Medeiros*, Marina Costa, Ana Ramoa, Sofia Ribeiro, Rosário Araújo, Manuela Vasconcelos, Margarida Monteiro
Internal Medicine Department, Braga Hospital, Portugal
Received Date: 08/03/2021; Published Date: 17/03/2021
*Corresponding author: Joana Trigo Medeiros, Internal Medicine Department, Braga Hospital, Portugal. Sete Fontes, S. Victor, Braga, PT 4710-243. Email: jrtmedeiros@gmail.com, +351 253 027 000. Address:1855 W, Taylor Street, Chicago, Illinois 606012. Email: jeffwyu@uic.edu.
CASE DESCRIPTION
An 87-year-old female patient with history of hypertension, dyslipidemia and Parkinson disease, enters in the emergency room with complaints of dyspnea after vomiting food content. The patient had undergone terminal colostomy due to a rectovaginal fistula, three years ago.
Laboratory evaluation showed infiltration in the right lower pulmonary lobe, hypoxemic respiratory failure and hyperlacticaemia. Aspiration pneumonia was assumed, and the patient was admitted to the internal medicine service where she started empirical antibiotic therapy with amoxicillin and clavulanic acid. A nasogastric tube was placed due to persistent vomiting with food intolerance. During hospitalization, the patient had complained of abdominal pain with maintained drainage of fecaloid content, experienced worsening of inflammatory parameters. In the suspicion of an occlusive intestinal condition, an abdominopelvic computerized tomography was performed, which showed an exuberant gastric distension with enlargement of the stomach to the pelvis (Figure 1). Upper digestive endoscopy revealed an antrum stenosis (Figure 2) and the presence of stasis content with areas of ulcerated mucosa (Figure 3). Patient's clinical condition worsened, and she died one week later.

Figure 1: Abdominopelvic computerized tomography showing an enlargement of the stomach to the pelvis.

Figure 2: Upper digestive endoscopy showing a stenosis of the gastric antrum which did not allow the progression of the endoscope.
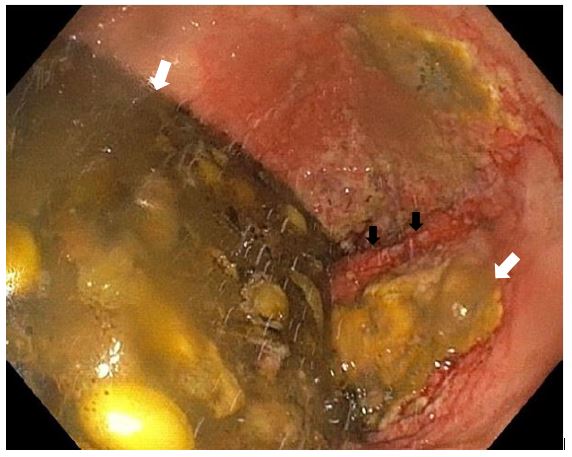
Figure 3: Upper digestive endoscopy showing areas of ulcerated mucosa (black arrows) and stasis food content (white arrows).
Several common neurologic disorders are associated with dysmotility of the upper gastrointestinal tract and resultant gastroparesis. Extrinsic neural control of gastrointestinal tract, myenteric plexus and autonomic nervous system can be affected in Parkinsonism [1-3]. In fact, enteric nervous system dysfunction may precede motor symptoms in this neurologic disorder [4]. Additionally, some medications used to treat this condition can also contribute to gastric stasis [5]. Although gastrointestinal transit time is slower in elderly people, particularly in patients with Parkinson disease, it is important to consider the possibility of an intestinal occlusion in persistent vomiting scenarios.
Conflicts of Interest:
None.
Grant Information:
The authors received no specific funding for this work.
References
- Jost WH. Gastrointestinal dysfunction in Parkinson's Disease. J Neurol Sci. 2010 Feb 15; 289(1-2): 69-73.
- Cersosimo MG, Benarroch EE. Pathological correlates of gastrointestinal dysfunction in Parkinson's disease. Neurobiol Dis. 2012;46(3): 559-564.
- Kaye J, Gage H, Kimber A, Storey L, Trend P. Excess burden of constipation in Parkinson's disease: a pilot study. Mov Disord. 2006; 21(8):1270-1273.
- Abbott RD, et al. Frequency of bowel movements and the future risk of Parkinson's disease. Neurology. 2001; 57(3): 456-462.
- Jost WH. Gastrointestinal motility problems in patients with Parkinson's disease. Effects of antiparkinsonian treatment and guidelines for management. Drugs Aging. 1997; 10(4): 249-258.

