Epididymal Lymphangioma, an Unusual Cause of Scotal Swelling in Adult
Alioune S1*, Abdellahi D1, Amadou N2, Désiré W1, Pape Mawade N1, Mouhamed C1, Ousmane S1, Abdou N1, Néné Mariame S1, Ibou T2 and Papa Ahmed F3
1Department of Surgery, National Hospital Center, Pikine, Dakar, Senegal
2Department of Pathological Anatomy, Aristide Le Dantec Hospital, Dakar, Senegal
3Department of Urology-Andrology, Dalal Jamm Hospital, Dakar, Senegal
Received Date: 29/09/2020; Published Date: 29/10/2020
*Corresponding author: Alioune Sarr, Surgery department, National Hospital, Center, Pikine, Dakar, Senegal. E-mail: sarramoc@yahoo.fr
Abstract
Lymphangioma is a benign tumor caused by localised malformations of well differentiated lymphatic vessels. Epididymal localization is rare, especially in adults.We report a case of a 35 years old patient who had consulted for a swelling left scrotal. The physical examination revealed a nodule in the epididymis, which was confirmed by ultrasound examination of the scrotum. The diagnosis of epididymal lymphangioma was made by histological examination after orchiectomy.
Keywords: Lymphangioma; Adult; Epididymis
Introduction
Lymphangioma is a benign tumor caused by localised malformations of the well differentiated lymphatic vessels [1]. It is mostly seen in children and is most often located in the cervix (75%) or axillary region (20%) [2]. The epididymal location is exceptional, particularly in adults [3,4]. Epididymal lymphangioma can pose the problem of differential diagnosis with epididymitis tuberculosis or epididymal tumor. The diagnosis is usually histological.
Observation
Mr. A.D, a 35 years old patient, was admitted for a swelling, painless left scrotal which had been evolving for 12 months. The patient did not report any notion of tuberculosis contagion, trauma or scrotum surgery. On examination, there was a firm, painless, intra-scrotal mass of about 1 cm long axis with preservation of the epididymal-testicular sulcus. The facing skin was normal. The contralateral scrotum was unremarkable. The intradermal tuberculin reaction was positive at 15 mm. The various tumor markers of the testis were determined: lactate dehydrogenase (LDH) = 475 IU/L, alpha fetoprotein (αFP) = 4.01ng/ml and human chorionic globulin (ΒHCG) = 3.05ng/ml. There was an increase in α FP and LDH. Ultrasound examination of the bursae showed a well encapsulated tumor mass in the head of the epididymis. The diagnosis of epididymal tuberculosis or a tumor of the epididymis has been evoked.The indication for a left inguinal orchiectomy was placed and performed after first clamping the spermatic cord.On macroscopic examination, there was a very limited tumor formation of 1x 0.8 cm whitish on section. On microscopic examination, it was a well circumscribed para-testicular tumor formation, made up of vascular cavities of variable size, containing rare red blood cells and surrounded by normal endothelial cells. These cavities are separated by a connective and fibrous tissue of variable density. There was no sign of malignancy (Figure 1).Thus the diagnosis of left epididymal lymphangioma was retained.
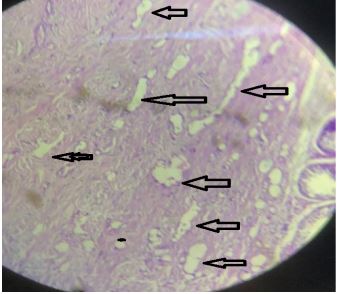
Figure 1: Haematoxylin eosin staining (x10) a proliferation of vessels of variable size coated with regular cubic cells (endo- thelium).
Discussion
Lymphangioma is a benign lymphatic malformation of the skin and subcutaneous cell, tissue diagnosed at birth or in childhood [5]. It accounts for about 26% of benign vascular tumors in children [5]. It presents clinically as painless masses in the cervical region (95%) [5]. Rarely does it develop in the retroperitoneum or the abdominal wall [5]. In the genital area, the scrotal location is the most described [1,2,6]. Locations in the spermatic cord and ovary have been reported [5,7].Epididymal lymphangioma in adults can be a primary neoplasm or a consequence of lymphatic obstruction after surgery or trauma [3]. In our patient, it was probably a primary neoplasm as the patient reported no history of surgery or trauma. Ultrasound imaging is the fundamental examination to make the diagnosis. It also allows us to look for an underlying lymphatic malformation, to determine the extent of the lymphangioma [3,6]. The main diagnostic hypothesis was epididymal tuberculosis in front of IDRT positivity; but especially epididymal tumor in front of α FP and LDH elevation.In our patient the diagnosis was difficult to establish before histology and the main diagnostic hypotheses were epididymal tuberculosis, but above all epididymal tumor in front of the elevation of LDH and α FP. So we opted for an orchiectomy by inguinal route. Classically the treatment of lymphangioma is surgical and is based on a broad excision to avoid recurrences [4]. Other therapeutic alternatives have been reported, including: repeated irradiation with X-rays, aspiration and injection of sclerosing agents. However, the results are variable, with considerable local or systemic side effects [1].
Conclusion
Our observation is atypical because of its location and the terrain. Thus, in front of any epididymal mass in adults, it is necessary to mention an epididymal lymphangioma in order to avoid radical surgery.
Conflicts of Interest
The authors stated that they had no conflict of interest.
Authors' Contributions
All authors have read and approved the final version of the manuscript.
References:
- Hamada Y, Yagi K,Tanano A,Kato Y,Takada K,Sato Met al. Cystic lymphangioma of the scrotum. Pediatr. Surg. Int. 199 ;13:442-444.
- Hurwitz R S , Shapiro E, Hulbert W C , Diamond D A , Casale A J, Rink R C. Scrotal cystic lymphangioma : the misdiagnosed scrotal mass. J Urol. 1997;158:1182-5.
- Postius J, Manzano C, Concepción T, Castro D, Gutierrez P, Bañares F. Epididymal lymphangioma. J Urol. 2000;163:550-1.
- Kok KY, Telesinghe PU. Lymphangioma of the Epididymis. Singapore Med J. 2002;43:249-50.
- Jamal YS, Abdel-Halim AR, Moshref SS, Kurdi MO, Sandugji HI. Cystic lymphangiomas of spermatic cord: A case report and literature review. JKAU Med Sci. 2009;16:103-111.
- Rastogi R, Meena GL, Kumar R, Rastogi V. Cystic lymphangioma scroti: A common tumor at a rare location. Saudi J Kidney Dis Transpl. 2010;21:1132-34.
- Derdabi H, Akerraz A, El Fazazi H, Kouach J, Moussaoui R D, Dehayni M. Lymphangiome ovarien: A propos d’un cas et revue de la littérature. International Journal of Innovation and Applied Studies. 2014;7 (1):111-114.

