Rare Presentation of Unilateral Chorio-Retinal Coloboma in a Patient with Bilateral Retinitis Pigmentosa
Indranil S*
Consultant, Vitreo-Retina, Sitaper Eye Hospital, India
Received Date: 15/08/2020; Published Date: 28/08/2020
*Corresponding author: Indranil Saha, Christian Medical College and Hospital, Vellore-632002, Tamil Nadu, India. indranil124saha@yahoo.co.in
Clinical Image
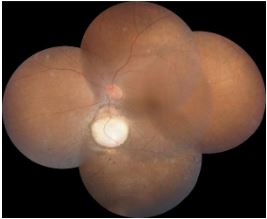
Inherited Retinal diseases are an incurable cause of visual morbidity occurring in children and young adults. Retinitis pigmentosa is one of the commonest examples of inherited retinal diseases with a prevalence of 1 per 4000 individuals [1,2]. Colobomas are known to occur in approximately 1 per 10000 people. Colobomas occur due to defective closure of the embryonic fissure between 6th – 7th week of development fetal life, and are under diagnosed as they don’t cause symptoms until they involve the disc or macula or both [3]. Retinitis pigmentosa and choroidal coloboma are known to usually exist as two separate entities. The fundus photo shows features of Retinitis pigmentosa, with an isolated chorio-retinal coloboma inferior to disc, in a 30 years old lady, who, presented with decreased peripheral vision and nyctalopia. There was no history of consanguinity. On evaluation she was found to have 6/6 vision bilaterally. Anterior segment was unremarkable in both eyes. Right eye fundus showed features of Retinitis pigmentosa. Humphrey Visual Fields 24-2 tests showed bilateral visual field defects, explaining the loss in peripheral vision. After extensive literature review, such association of unilateral coloboma in a patient with bilateral Retinitis pigmentosa, with no other systemic anomalies is extremely rare, and has been reported only in a few cases [4,5].
References:
- Pierrache LHM, Kimchi A, Ratnapriya R, et al. Whole-Exome Sequencing Identifies Biallelic IDH3A Variants as a Cause of Retinitis Pigmentosa Accompanied by Pseudocoloboma. Ophthalmology. 2017;124(7):992-1003.
- Haim M. Epidemiology of retinitis pigmentosa in Denmark. Acta Ophthalmol Scand Suppl. 2002;(233):1-34.
- Stoll C, Alembik Y, Dott B, Roth MP. Epidemiology of congenital eye malformations in 131 760 consecutive births. Ophthalmic Paediatr Genet. 1992;13:179-186.
- Agarwal P, Karande PS, Vadhel L, Naheed A. Retinitis pigmentosa with unilateral Choroidal coloboma. A rare association. J ClinOphthalmol Res. 2013;1:187.
- Parmeggiani F, Mlan E, Costagliola C, Giuliano M, Moro A, Steindler P, et al. Macular coloboma in siblings affected by different phenotypes of retinitis pigmentosa. Eye (Lond). 2004;18:421-8.

