Coronary Embolism Myocardial Infarction: About Two Observations of Patients in Complete Arrhythmia By Atrial Fibrillation
Nuance Divine TCHILOEMBA TCHIBINDA*, Christelle MPEMBA RAPAGA, Chimène KITIHOUN, Fatimatou Zarha COULIBALY, Latifa OUKERRAJ, Mohammed CHERTI
Department of Cardiology B, CHU IBN SINA, Mohammed V University of Rabat, Morocco.
Cardiology Residents, Mohammed V University of Rabat, Morocco
Professor in cardiology, Mohammed V University of Rabat, Morocco
Professor and head of cardiology department, Mohammed V University of Rabat, Morocco
Received Date: 20/10/2021; Published Date: 25/11/2021
*Corresponding author: Nuance Divine TCHILOEMBA TCHIBINDA, resident in cardiology, CHU IBN SINA, Mohammed V University of Rabat, Morocco.
Summary
Myocardial Infarction (MDI) is, in the vast majority of cases, attributable to coronary thrombosis developed on a pre-existing atheromatous lesion. However, other causes are possible and, among them, coronary embolism seems to occupy a significant place.
Coronary embolisms can occur through various mechanisms, including a thrombus of the left auricle due to AF, valvular vegetation secondary to infection or autoimmune endocarditis; Deep venous thrombus paradoxically embolizing by a permeable Foramen Ovale (FOP), or iatrogenic secondary to coronary interventions. Of these, AF is considered the most common etiology of coronary embolism, although there are few reported cases in the literature. Two observations of myocardial infarction by probable coronary embolism are described occurring in patients in Complete Arrhythmia by Atrial Fibrillation (ACFA).
Keywords: Myocardial infarction; Coronary embolism; Atrial fibrillation
Introduction
Atrial fibrillation carries a significant risk of embolism, on average multiplied by 5, but variable depending on the underlying heart disease; it can be multiplied by 18 in case of mitral narrowing. Anticoagulation is the mainstay of treatment to reduce the risk of stroke and peripheral embolization. However, a myocardial infarction by coronary embolism is a rare entity. We report the observation of two patients followed for ACFA who had acute coronary syndrome with angiographically healthy coronary arteries.
Case Clinique 1
Mrs. C.A aged 74 years, hypertensive in Cardiac Arrhythmia by Atrial Fibrillation (ACFA) for 8 years Under sintrom and digoxin; admitted for chest pain infarction having consulted at H2. At her admission the patient kept a painful background, with signs of left ventricular failure, and a diastolic roll in the mitral focus; The electrocardiogram (Figure 1) finds an ACFA with an average ventricular rate (CVM) at 100bpm, a planing of the R wave in antero-septal, negative T waves in circumferential. The X-ray (Figure 2) of the chest shows cardiomegaly with sub-diaphragmatic tip, a straight left middle arc, a double contour appearance with right overhang, bilateral hilar overload. At the biological assessment: the INR was outside the therapeutic zone (1.86), and a positive troponin at 36ng/l. At ETT (Figure 3) we find a tight mitral narrowing (S = 1.18cm2) fibrous rheumatic, a moderately tight aortic narrowing; an undilated left ventricle in moderate systolic dysfunction, with hypokinesia of the apex and adjacent segments, an ectasia left atrium seat of spontaneous contrast. Coronary angiography (Figure 4) shows angiographically normal coronaries outside of a thrombotic, non-occlusive and small-extent image of the anterior Interventricular Artery (IVA) which is treated with intravenous heparin relayed by a VKA and an antiplatelet agent P2Y12. The evolution is simple, the patient is in ACFA slowed down by beta-blockers with an INR 2.6 and a troponin in kinetics of decrease from 36 to 2ng / l.
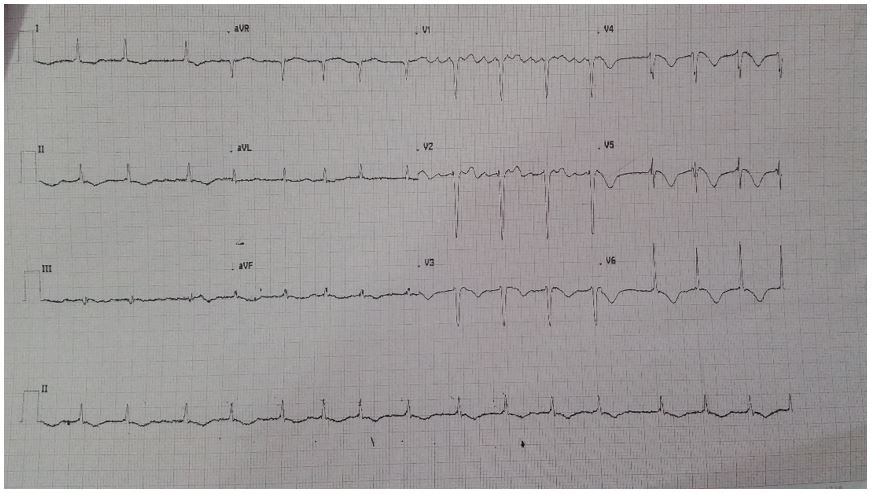
Figure 1: ACFA ECG with a Mean Ventricular Rate (CVM) at 100bpm, planning of the R wave in antero-septal, negative T waves in circumferential.

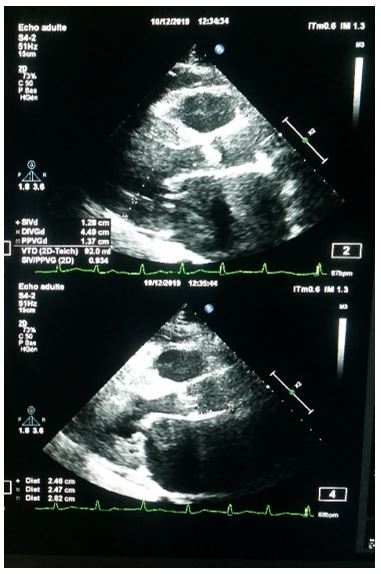

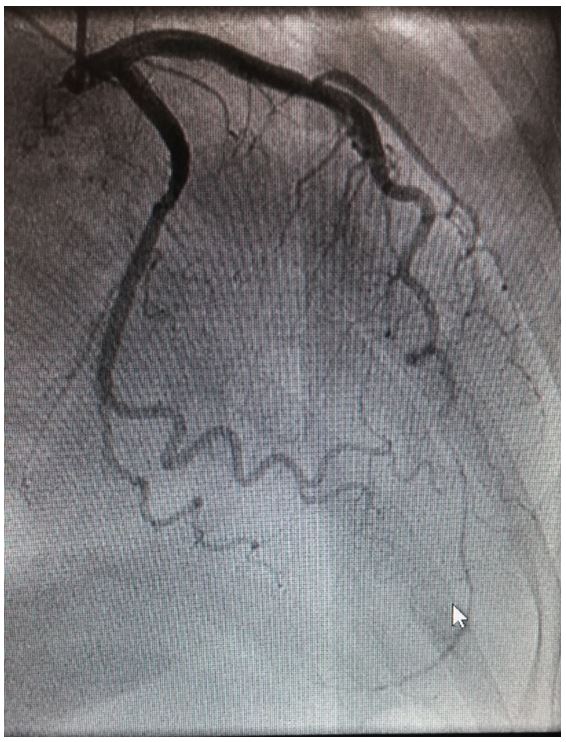
Figure 4: coronary angiography: thrombotic, non-occlusive and small-extent image of the anterior interventricular artery (IVA).
Clinical Case 2
Mrs. L.M 60 years old; followed for 02 years for non-valvular Atrial Fibrillation (AF); admitted to hospital for chest pain on Day 8 complicated by angina recurrence and left ventricular failure; the ECG (Figure 5) shows AF with a mean ventricular rate (CVM) at 70bpm, an extra shift of the ST segment, Q wave of necrosis in anterosepto-apical and negative T waves in deep septal; echocardiography finds a dilated left ventricle, seat of akinesia of the apex and adjacent segments with hypokinesia of the rest of the walls; severe impairment of systolic function, and dilation of the atria; in the biology assessment we find a positive troponin at 53ng / l and an INR at 1.3 (under dose); coronary angiography (Figure 6) performed shows an intermediate lesion of the upper distal IVA followed by a thrombus with TIMI III flow; under medical treatment (triple therapy by AVK plus double anti platelet aggregation for 01 months; and dual AVK and P2Y2 therapy for 12 months; finally AVK alone.

Image 5: ECG: FA with CVM at 70bpm; plus ST segment offset and ASA necrosis Q waves; deep septal negative T-waves.

Figure 6: Coronary Angiography: thrombotic intermediate lesion of the upper distal IVA followed by a thrombus with TIMI III flow.
Discussion
Myocardial Infarction (MDI) by coronary embolisms is considered rare. The explanations given call for: the narrowness of the coronaries in relation to the diameter of the aorta and the importance of the aortic flow; diastolic filling of the coronaries while most of the aortic flow is in systole; to the "protection" of the coronary ostia in systole by the opening of the aortic sigmoids.
72% of cases involve the left network and occlusions are most often distal. In 15% of cases, coronary embolisms are multiple. In 40% of cases, extracardiac embolic localizations are associated. They conclude that although "valve damage remains the leading cause of coronary embolism," bacterial endocarditis appears less frequently responsible.
Coronary embolisms are frequently associated with mur mur mur murbus, especially in patients with ACFA and those with dilated cardiomyopathy (CMD).
Coronary embolism infarction may be less rare than published observations suggest. This apparent rarity may be due to the difficulty of proving the mechanism of embolism, so that many cases are not published. Makino and Al-Sadir [13], for example, collect 12 cases of suspected coronary embolism found in three years in their center. 294 C. Gully et al. / Annales de Cardiologie et d'Angéologie 57 (2008) 290–294 Si.
These publications, like ours, most often carry out "suspicions of coronary embolisms". Indeed, "proof" of coronary embolism is not made. The criteria in principle required are: the coronarographic aspect; identification of the origin of the thrombus (ultrasound, CT, MRI); it is accepted that the existence of a spontaneous contrast in the OG in ETO is a strong argument to identify the origin of the thrombus; endodocron ultrasound with demonstration of the normality of the intima would be the third criterion.
However, the absence of stenosis at coronary angiography immediately after clot lysis or remotely is an accepted argument in favor of diagnosis. Clinically it is most often a caricatural picture of Acute Coronary Syndrome (ACS). Patients generally do not have a history of angina. Nevertheless, data from the literature demonstrate that the clinic can range from silent infarction to sudden death. In our series, these are limited infarctions revealed by chest pain.
The left coronary artery is the artery most often affected. The classic causes form a catalog from which valvulopathies and endocarditis emerge. ACFA is often associated with classical causes, but non-valvular ACFA is likely to be an increasingly common possibility due to the increase in the number of patients with ACFA and thromboembolic risk and the increase in coronarographic explorations in the elderly. In the same vein, we can ask ourselves the question of looking for unnoticed strokes in these patients. Clinical cases described in vivo as ours, it should be noted that absolute proof of the mechanism is only rarely provided and that these are most often diagnoses of (high) probability. This may explain why many suspicions of coronary embolisms are not published.
In acfa, published observations often report imperfect hypocoagulability, discontinuation of anticoagulant therapy or the possibility of an associated procoagulant factor. Treatment of early diagnosed acute infarction may involve thromboaspiration combined with distal protection. Background treatment depends on the suspected origin of the thrombus and the mechanism of embolism. He most often uses long-term VKAs.
In our case report, patients were medically managed with anti-vitamin K in addition to an antiplatelet agent P2Y12 given the absence of significant damage to coronary angiography.
Conclusion
The prevalence of IDM by coronary embolism is estimated to be close to 3%. Its biggest cause is atrial fibrillation which is far from being taken into account. Patients often have varying levels of concomitant atherosclerosis that can worsen or confuse the picture. Distinctions can, however, be made angiographically. Management is the same for both: anticoagulation; thrombolysis and stent setting. Thrombo-aspiration may be considered in patients with a heavy thrombotic load. In addition, it is important to consider bleeding risks given the need for both anticoagulant and antiplatelet therapy in these patient groups.
The authors consider that coronary embolism infarction is more common than we think, but remains "underdiagnosed", they propose to look for embolic risk factors when the diagnosis of normal coronary infarction is made.
References
- Gully C, et al. Annales de Cardiologie et d'Angéiologie, 2008; 57: 290-294.
- Shibata T, et al. coll: Prev alence, Clinical Features, and Prognosis of Acute Myocardial Infarction Attributable to Coronary Artery Embolism. Circulation 2015; 132: 241-250.
- Hussein Daoud et Ashraf Abugroun / Case Reports in Cardiology / 2019 / Article ID 9347198: Acute Coronary Syndrome (ACS) due to Coronary Artery Embolism in a Patient with Atrial Fibrillation
- Ravi Kumar Garg, Neeraj Jolly / j. ijcard.2006.11.095/ PMID: 17291607: Acute myocardial infarction secondary to thromboembolism in a patient with atrial fibrillation.
- Waller BF. Atherosclerotic and nonatherosclerotic coronary artery factors in acute myocardial infarction. Cardiovasc Clin 1989; 20: 29-104.
- Wenger NK, Bauer S. Coronary embolism. Review of the literature and presentation of 15 cases. Am J Med 1958; 25: 549-557.
- Prizel KR, Hutchins GM, Bulkley BH. Coronary artery embolism and myocardial infarction, a clinicopathologic study of 55 patients. Ann Intern Med 1978: 88155-88161.
- Marcu CB, Israel DH, Donohue TJ. Paradoxal coronary embolism, extensive pulmonary embolism and deep venous thrombosis. J Invasive Cardiol, 2005; 17(9): 487-488.
- Takenaka T, Horimoto M, Igarashi K, Yoshie H, Tsujino I, Morihira M. Multiple coronary thromboemboli complicating valvular heart disease and atrial fibrillation. Am Heart J, 1996; 131: 194-196.
- Cheng T. Coronary embolism (letter). Am Heart J 1996;132: 1314-1316.
- Mejia VM, Woo YJ, Herrmann HC. Left main coronary embolism. J Invasive Cardiol 2006; 18: 296.
- Canali G, Girardi P, Barbieri E. Coronary embolus and acute myocardial infarction in a patient with dilated cardiomyopathy and chronic atrial fibrillation. G Ital Cardiol 2006; 7: 365-368.
- Makino H, Al-Sadir J. Myocardial infarction in patients with mitral valve prolapse and normal coronary arteries. JACC 1983; 1(2): 661.

