The Neurosurgical Approach Algorithm in the COVID-19 Pandemic: A Comprehensive Approach to Neurosurgical Case Prioritizaton and Management in Paraguay
Juan Jose J and Noor-ul-Huda M*
Institute of Neurosciences, Pakistan
Received Date: 16/09/2020; Published Date: 25/11/2020
*Corresponding author: Noor-ul-huda Maria, Punjab Institute of Neurosciences, Pakistan, E-mail: iii_glow_iii@ymail.com
Just before 31st December 2019, nobody could believe to be recalling and repeating the historical wordsof Marcus Terentius Varro(116 BC-27BC) as far back as 100BC for Sepsis who historically quoted “small creatures, invisible to the eye, fill the atmosphere, and breathed through the nose causing dangerous diseases.” And these words echoed through the era of the “Black Death” and re-emerged again after man has conquered the space and planted his foot on the moon. Combating with our shared invisible enemy has now challenged us to our limits.We are in it together as “one world”. We are now facing the reality of the limitations imposed by our resources , instead of directing our resources in terms of manpower and finances, our resources are driving us to divert and manage wisely and save as much lives as we can while no patient of ours suffers. The health sector has been hugely overlooked in several parts of the world as nobody was ready to foresee an unforeseen and there were poor preparations for a health emergency [1].
Back in time, let’s recall, In 1900, infectious disease was a leading cause of death; in 2000, infectious diseases were responsible for only a small percentage of deaths in developed nations [2]Following the discovery of the first antibiotics, the field of antibiotic research went through a boom from 1930 to 1970 with the discovery of many of the clinically used antibiotics. This golden era was followed by a 30-year slump with a sharp drop in the number of new natural product antibiotics discovered [3]. In medicine ,specialties who deal with serious and potentially lethal and crippling pathologiesin which Neurosurgery is on top, the ongoing COVID-19 crisis has put forward a special challenge to deal with our patients. We share several resources such as ICU equipment and staff, monitors and special nursing care with the emergency department and ICUs who are now overwhelmed with the victims of COVID-19. It is a challenging time for us to smartly allocate slots for only those patients whom cannot be deferred at any cost. And this is just one aspect, the other aspects include receiving neuro emergencies of patients who are COVID-19 positive, predicting your asymptomatic patients about their COVID-19 status and reducing transmission of COVID-19 .Every country and continent has introduced their guidelines which are wisely tailored according to the incidence of COVID-19 cases in their countries and the workload on their departments.

Figure 1: Algorithm introduced at Paraguay.
Designed to filter the cases that cannot be deferred this algorithm describes a balanced well crafted approach to first detect and filter the “elective cold cases” that may wait such as carpal tunnel syndrome surgery and other pathologies which do not emergently compromise spinal cord and brain function and are not potentially “fatal”. Here we want to specially emphasize at one’s level of clinical assessment which is of utmost importance. Ideally teams should be made with the most experienced one acting as leader and hierarchy be followed. The consultant should be in contact through telemedicine if need arises, making it able to properly filter away only those who can really fulfil the criteria of deferring surgery and not to miss the cases wrongfully which may lead to mortality and morbidity out of one’s lack of expertise. The cases ideal for operative management are the ones that can be managed with a relatively “ simpler” and “shorter” surgical procedure. As many international guidelines have indicated, endoscopic surgery needs to be avoided.Similarly drilling in and around the areas of sinus should be performed carefully. There should be profuse irrigation to avoid aerosol during drilling. After identifying the cases in whom surgery is unavoidable, we will now have to determine the Covid-19 status of the given patients.
As per guideline by the Society of Neurosurgery Paraguay , the given checklist should be followed
Management of Suspected Patients/Confirmed Cases Of COVID-19 that Require Surgical Intervention
A) Unavoidable Scheduled Surgery
An evaluation prior to surgery must be performed by the Anesthesiology service, evaluating:
- Pathological chest radiography:Yes / No. In case of YES, perform chest CT.
- Presentation atany respiratory clinic(outdoor) during the previous 14 days:
- Fever of non-affiliated origin: Yes / No
Before the affirmative answer to any of the previous questions, aCOVID investigation and will wait for the result.If the result is positive, the institutional action protocol must be followed inOperating rooms / resuscitation for patients with SARS-CoV-2 infection.
B)Emergency Surgery
An evaluation prior to surgery must be carried out by the responsible anesthesiologist evaluating:
- Pathological chest radiography: Yes / No. In case of YES, perform chest CT.
- Presence of respiratory clinic during the previous 14 days: Yes / No
- Fever of non-affiliated origin: Yes / No
Before the affirmative answer to any of the previous questions, aCOVID research. If the result is positive, the institutional action protocol must be followed inOperating rooms / resuscitation for patients with SARS-CoV-2 infection.In the event that the result is not available before surgery, it will act as if it were positive until you have the result. In order to minimize exposure it is recommended to limit the number of professionals to as few as possible during surgery we recommend having the maximal level of expertise of the professionals involvedin the management of this type of patients [4].
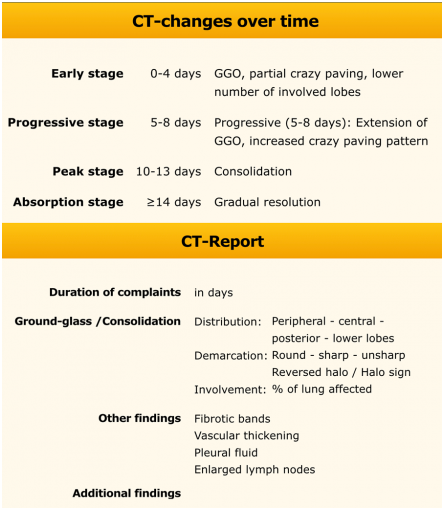
As we all know, all around the world, there still is a lack of availability of tests especially rapid testing. This would impose a special dilemma if patient is in a need of emergent surgery such as neurotrauma, intracranial hematomas, coning, intracranial hypertension and others. In that case one needs to rely on “epidemiological” link, of course patient will be thoroughly inquired regarding any symptom that can be as subtle as anosmia and history should be taken while practicing necessary precautions. Temperature should be recorded . In case there is no epidemiological risk ,carry out conventional surgery taking standard precautions ,however this is still debatable but it is the only feasible way for management. Where there is an epidemiological risk, the patient should be to immediately sent for a “chest CT scan” [5]. If the CT indicates suspicion of Covid-19 , surgery should be undertaken with special precautionary protocols. In patients having positive epidemiological linkage but without CT findings indicating Covid-19 infection , an option of minimally invasive surgery should be explored if it is possible. If it is not possible and one has to go for conventional surgery then it should be undertaken using proper PPE. As per guidelines we now want to share the details of what we refer to as the PPE needed to manage the Covid-19 positive confirmed or suspected cases.
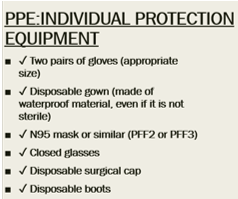
Guide for the Placement and Removal of Personal Protective Equipment (PPE) for aerosol-generating procedures in Covid-19 positive or suspects
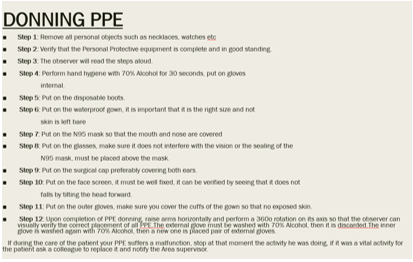
Donning Personal Protective Equipment
- There will be a specific placement area divided into two zones; Clean Area and Dirty Area
- The placement of PPE must be done in the Clean Area
- An observer will supervise the entire process
- A list of instructions, verbal commands and visual verification will be used to ensure the proper completion of all steps
All the steps must be carried out slowly to avoid accidents.
- Step 1: Remove all personal objects such as necklaces, watches etc
- Step 2: Verify that the Personal Protective equipment is complete and in good standing.
- Step 3: The observer will read the steps aloud.
- Step 4: Perform hand hygiene with 70% Alcohol for 30 seconds, put on gloves internal.
- Step 5: Put on the disposable boots.
- Step 6: Put on the waterproof gown, it is important that it is the right size and not skin is left bare
- Step 7: Put on the N95 mask so that the mouth and nose are covered
- Step 8: Put on the glasses, make sure it does not interfere with the vision or the sealing of the N95 mask, must be placed above the mask.
- Step 9: Put on the surgical cap preferably covering both ears.
- Step 10: Put on the face screen, it must be well fixed, it can be verified by seeing that it does not falls by tilting the head forward.
- Step 11: Put on the outer gloves, make sure you cover the cuffs of the gown so that no exposed skin.
- Step 12: Upon completion of PPE donning, raise arms horizontally and perform a360o rotation on its axis so that the observer can visually verify the correct placement of all PPE. The external glove must be washed with 70% Alcohol, then it is discarded. The inner glove is washed again with 70% Alcohol, then a new one is placed pair of external gloves. If during the care of the patient your PPE suffers a malfunction, stop at that momentthe activity he was doing, if it was a vital activity for the patient ask a colleague to replace it and notify the Area supervisor.
Removal of Personal Protective Equipment
- It must be done with conscience and slowly.
- Go to the Dirty Area, an observer will supervise you during the process.
- Remember that the most contaminated areas of your PPE are: the external face, the anterior face of the
gown, the outer face of the sleeves, the outer face of the goggles and the outer face of the mask.
- Wait until you receive the complete instructions before carrying them out.
The observer will read aloud the EPP withdrawal sequence and verify the correct performance
of the steps.
- Step 1: Disinfect the external gloves with 70% alcohol for 30 seconds, remove the external gloves slowly and gently so as not to tear the internal gloves, using the beak technique, then discard them. Dispose of in Type 2 container (Red Bag).
- Step 2: Inspect the inner gloves, if you find a break notify the Area supervisor. Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 3: Remove the face shield, taking the strips from the back. Discard in the Type 2 container (Red Bag).
- Step 4: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 5: Remove the knot from your gown, taking with both hands at the anterior superior level of the Chest stretch forward from the center of your gown, so that the magnetic closure opens back, the gown is lowered to the chest area and carefully removed2 (Red Bag).
- Step 6: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 7: Remove the cap by tilting your head forward and grasping it with both hands.
- the back (of the nape) and taking care that the external face
- Step 8: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 9: Remove the glasses by grasping the back of the straps while tilting your head forward. Place in the container with Sodium Hypochlorite Solution, avoiding splashes, for washing and disinfection.
- Step 10: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 11: Remove the N95 mask by tilting the head forward and initially taking the lower strip at the back and passing over the upper strip, later take the upper strip and pass over your head completely removing the mask, so that at no time does it touch her face.
- Step 12: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 13: Stand on a chair in the Dirty Area to remove your boots taking care to only step on the Clean Area once they have been removed. Dispose of in Type 2 container (Red Bag).
- Step 14: Disinfect the inner gloves with 70% Alcohol for 30 seconds.
- Step 15: Remove the inner gloves being careful not to touch the outer part of them, using the beak technique.
- Step 16: Disinfect your hands with 70% Alcohol for 30 seconds.
Recommendations
The solution where the glasses are disinfected will have a concentration of 1 to 10, that is, 10ml of Sodium Hypochlorite in 1000ml of Water.
Action in Case of Contact with Suspected COVID-19
We must act in the following way depending on the presence of clinic and exposure in function of:
- Type of exposure: low / high risk.
- Exposure time:> 15 min less than 2 meters away.
- Service in which the healthcare activity is carried out: in units with patients especially
vulnerable (ICU, OER, haemato / oncology, burn unit). It is suggested that one needs to be self isolated immediately after exposure for 14days.
References:
- Mohr K. History of Antibiotics Research. Curr Top Microbiol Immunol. 2016;398:237-272.
- Lara R. Fremont,Antibiotic Discovery.Labome 2018;8:2671.
- https://radiologyassistant.nl/chest/lk-jg-1.

