Evaluation of Patient Satisfaction in the Covid Period at the Retrocession Unit
Aboubacar Sekou Kaba1,*, Badr Adouani1, Hajar ZHAR1, Mohamed Réda Sefrioui2, Yasmina Tadlaoui1, Jamal Lamsaouri1
1Laboratory of Pharmacology-Toxicology, Faculty of Medicine and Pharmacy of Rabat, Mohamed V University of Rabat, Morocco
2Laboratory of Medicine Sciences, Biomedical and Biotechnological Research, Faculty of Medicine and Pharmacy of Casablanca, Hassan II University of Casablanca, Morocco
Received Date: 21/05/2022; Published Date: 06/06/2022
*Corresponding author: Aboubacar Sekou Kaba, Resident in clinical pharmacy, Mohamed V Military Training Hospital of Rabat, Faculty of Medicine and Pharmacy, Mohamed Vde Rabat University, Morocco
Abstract
Objective: The main objective of this study conducted with patients is to know the accessibility of drugs intended for patients and the secondary objectives of measuring the pharmaceutical service rendered to the patient, assessing the level of patient satisfaction, and determining retrocessions that require pharmaceutical maintenance.
Methods: This was a prospective study carried out in the retrocession unit of the Mohamed V Military Hospital in Rabat during the COVID-19 pandemic. A satisfaction survey was conducted over a three-month inclusion period during the lockdown. A questionnaire was submitted to the volunteer patients during the dispensing of their medications. The sample was made up of a random survey.
Results: A total of 280 patients were enrolled in our study. The average age was 50+ or -35 years. For 75 (27%) patients’ treatment was unavailable, 205 (73%) patients were satisfied with the availability of treatments. The rupture concerned certain mandatory essential medicinal products in particular methotrexate, 5 fluorouracil, cisplatin, oxaliplatin, vincristine, lenalidomide, anastrozole, exemestene filgrastim.
Conclusion: The results of our study show that patient satisfaction is based on effective reception and communication from the pharmaceutical team and the creation of a patient-pharmacist link.
This study demonstrated a high satisfaction rate for both outpatients and inpatients.
Keywords: Covid 19; Rupture; Hospital pharmacy; Anticancer; Treatment
Key Messages
State of scientific knowledge of the subject before the study:
Retrocession consists of dispensing by a pharmacy for indoor use, drugs not available in city pharmacies to outpatients to meet their satisfaction. Unfortunately, in this COVID 19 period the main critical point related to the circuit of retroceded drugs is the supply of hospital pharmaceutical products which has experienced a disruption.
Why did this study need to be carried out?
This study was conducted to describe patient satisfaction-related failures in a retrocession unit, which will allow us to perform corrective actions.
Following this study, we can be sure that all factors related to supply will be taken into account in order to avoid the disruption of drugs to the retrocession unit.
Introduction
Pharmacies for domestic use (PUI) of public or private establishments participating in the public hospital service (PSPH) are authorised by way of derogation to dispense at retail to non-hospital patients’ medicinal products reserved for hospital use belonging to the category of medicinal products subject to restricted prescription for which the prescription is reserved for certain health professionals [1].
Hospital retrocession is a derogatory activity of pharmacies for domestic use (PUI) and consists in the dispensing of particular drugs to outpatients, these are drugs registered on a list called "retrocession list". This dispensing process presents health risks, the role of the pharmacist is to improve the information given to the patient during a dispensing of drugs requiring special care and / or monitoring and in particular during a retrocession [2,3].
Retrocession is a critical pharmaceutical activity requiring security and a global approach to care for which the pharmacist is the last link in the drug circuit and whose economic profitability raises questions. In this context, risk mapping and economic assessment appear to be necessary [4,5].
In a context of ISO 9001 certification, the formalization and harmonization of dispensations during retrocessions is a commitment of our PUI. To be retrocedable, the medicinalproducts must be entered on the list of specialties approved by a committee and the expensesare then not charged to the hospital's budget but are reimbursed. The medicinal products on this list are generally dispensed by the PUIs. These include antivirals, hormonal therapy drugs, oral cytotoxic anticancer drugs and oral targeted therapies. These are drugs identified as high risk, given their narrow therapeutic range and intrinsic toxicity. However, a patient treated with oral chemotherapy is also an identified high-risk patient. His care path is complex, his therapeutic management is heavy [6,7].
The role of the pharmacist evolves and new activities are entrusted to him. In order to support this evolution, we are interested in patient satisfaction, the impact and benefits of the pharmacist's activities. The hospital pharmacist carries out at the retrocession unit the activities of supply, dispensing, traceability of medicines, pharmaceutical analysis of prescriptions but also information for doctors and outpatients. The pharmacist is a key player in public health involved in the entire drug chain, he is at the heart of patient care [8,9].
Retrocession is therefore one of the most risky activities of indoor pharmacies (PUIs), placing the pharmacist as the last lock before the administration of the drug. Retrocession consists of dispensing drugs not available in a city pharmacy to outpatients through a PUI [10,11]. In this COVID 19 period the main critical point related to the circuit of retroceded drugs is the supply of hospital pharmaceutical products. Pharmaceutical activities have been impacted in our unit. The COVID-19 pandemic (SARS-CoV-2 virus) has brought a major impact on our pharmaceutical practices. Since the beginning of the crisis, our supply system has experienced a disruption in hospitals [12,13].
The management of these drugs is an international issue in the therapeutic care of the patient given the constraints related to supply times. The medicinal products dispensed most often correspond to risky medicinal products with a Marketing Authorisation (MA) or a temporary recommendation for use (RTU), hospital preparations as well as specialities under temporary authorisation for use (ATU) or import authorisation (AI). These treatments often require management as soon as the patient is discharged from hospital. In this drug supply chain, the pharmacist is the last step before the drug is administered and the economic profitability is questionable [14,15].
The main objective of this study conducted with patients is to know the accessibility of drugs intended for patients and the secondary objectives of measuring the pharmaceutical service rendered to the patient, assessing the level of patient satisfaction, and determining the retrocessions that require pharmaceutical maintenance.
In a context of continuous improvement of the quality and safety of service delivery in the patient's medication management, the measurement of patient satisfaction is an imperative criterion to be taken into account in the retrocession unit of the HMIMV in Rabat [16].
Patient satisfaction is a quality indicator of good hospital pharmacy practice for any indoor pharmacy in general and the retrocession unit in particular [17].
Materials and Method
As part of a quality approach, a prospective study was conducted with outpatient and inpatient patents in order to propose areas for improvement to better meet their requirements. It makes it possible to question individuals about their degree of agreement or disagreement with a statement. We therefore aimed to assess patient satisfaction with the retrocession unit [18,19].
This was a prospective study carried out within the retrocession unit of the Mohamed V Military Hospital in Rabat during the COVID-19 pandemic. A satisfaction survey was conducted over a three-month inclusion period during the lockdown. A questionnaire was submitted to the volunteer patients during the dispensing of their medications. The sample was made up of a random survey.
The frame corresponded to children and adult patients regardless of their gender or reasons for treatment. Patients who did not lend to questionnaires were excluded from the study. It included 11 questions assessing 6 aspects: level of the quality of the reception, level of satisfaction during the dispensation, level of satisfaction of the organization, level of the quality of the cleanliness of the premises, satisfaction of the dispensing time, waiting of patients on their treatments. A four-point scale (Very Satisfactory, Satisfactory, Unsatisfactory and Unsatisfactory) was used to estimate patient satisfaction.
A number of treatments concerned our study including hormone therapy, oral cytotoxic anticancer drugs and oral targeted therapies.
Results
A total of 280 patients were enrolled in our study. The average age was 50+ or -35 years.
Classes of managed drugs include antihormonals, oral and injectable cytotoxic anticancer drugs (oral and injectable anti-metabolites, platinum salts, taxanes, intercalants), oral and injectable targeted therapies (monoclonal antibodies, tyrosine kinase inhibitors), retrovirals, emetics and others with special status. The analysis of the 6 aspects made it possible to group the satisfaction rate into three dimensions (organization, information and management of ruptures).
Dispensing Period:
25 (9%) disabled and elderly patients were dissatisfied with the distance between the provision of care and our pharmacy, 4 (1%) patients were not satisfied with the dispensing time, 251 (90%) patients were satisfied with the dispensing time of the retrocession unit (Figure 1).
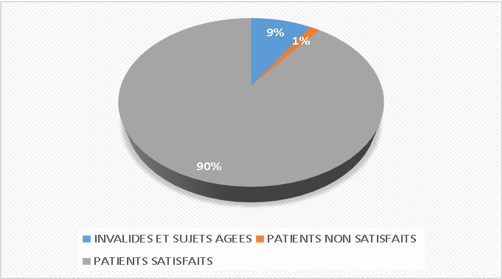
Figure 1: The number of times spent receiving treatment.
Availability of Treatments
For 75 (27%) patients’ treatment was unavailable, 205 (73%) patients were satisfied with the availability of treatments (Figure 2).
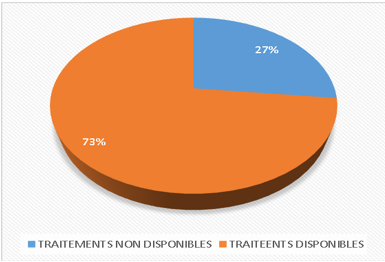
Figure 2: The availability status of treatments.
Organizational Side:
The overall satisfaction was related to the quality of the welcome, the cleanliness of the premises and the quality of the treatment. 23 (8%) patients requested the installation of an identification plate of the retrocession unit, 195 (70%) patients were satisfied with the quality of the reception, the cleanliness and the quality of the service, 44 (16%) patients mention an insufficient number of staff of the retrocession unit, 18 (6%) patients not satisfied with the quality of the treatments (Figure 3).
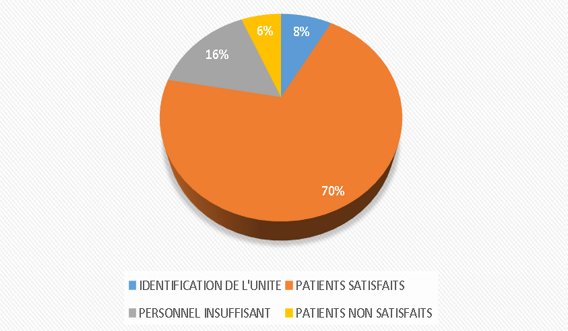
Figure 3: The number of patients satisfied and not with the organization of the retrocession unit.
Quality of therapeutic education:
58 (21%) patients did not accept the advice, because they are already used to their long-term treatment, 84 (30%) patients did not receive the advice of good use, 107 (38%) patients are satisfied with the quality of the advice of good use, 31 (11%) patients are not satisfied with the quality of the advice of good use (Figure 4).
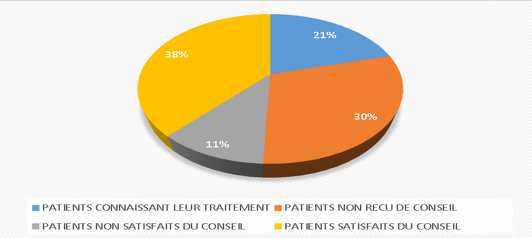
Figure 4: The quality of the advice provided to patients.
Breaks:
The rupture concerned certain mandatory essential medicinal products in particular methotrexate, 5 fluorouracil, cisplatin, oxaliplatin, vincristine, lenalidomide, anastrozole, exemestene filgrastim.
For 89 (32%) patients, treatment was out of order, 191(68%) patients were satisfied with their treatment (Figure 5).
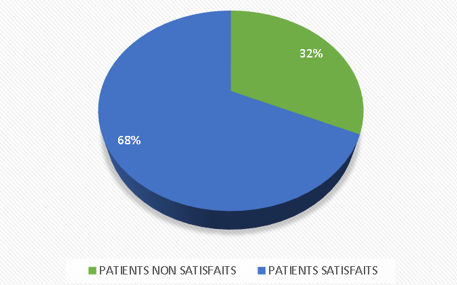
Figure 5: The number of patients who received or did not receive the treatment in this study.
Termination deadlines:
The break period can range from 7 days to 3 months per time more.
For 10 (10%) patients the rupture was national, for 02 (2%) patients the rupture time was 3 months, for 05 (5%) patients the rupture time was 2 months, for 42 (44%) patients the rupture time was 30 days,
For 02 (2%) patients the rupture time was 25 days, for 10 (11%) patients the rupture time was 20 days, for 16 (17%) patients the rupture time was 15 days, for 09 (9%) patients the rupture time was 07 days
The recommendation of the retrocession unit and the management of the remainders was related to the management of ruptures and the confidentiality of patient care (Figure 6).

Figure 6: The number of accusable days for the acquisition of treatments.
Discussion
Compared to previous years, despite the impact of the disruption during this period of the COVID-19 pandemic, patients were satisfied with the products and services and their satisfaction rate was higher.
There is a relationship between satisfaction and fidelity, but the specific case of the retrocession unit, we receive immunocompromised patients in real need of management.
In general, the responses were positive with regard to organization and the quality approach.
- Dispensing period:
The 25 (9%) disabled and elderly patients found the time taken longer to receive their treatment. This was independent of the retrocession unit, given the distance between the care centre and the retrocession unit.
4 (1%) patients were not satisfied with the time taken to receive their treatment, given the number of patients presenting per day and which is on average 50 patients per day and sometimes at the same time for a very small number of staff for the care of all patients.
On the other hand, 251 (90%) patients are satisfied with the time taken to receive their treatment.
- Availability of treatment:
A study carried out in 2004 on the hospital retrocession of medicinal products shows that the public health objective sought by the legislator presupposes that retrocession favours, for these often chronic patients, the accessibility of treatment, the continuity of care and the coordination of health actors [1].
Since the COVID-19 pandemic, pharmacists have faced the problem of stock-outs. The difficulty is the availability of retrocedable treatments within the authorized PUIs resulting in a break in treatment or a delay in care. The patient satisfaction survey is generally positive for all items except accessibility. However, it reports a significant proportion of patients reporting that they have not received full treatment. This answer can be interpreted by dissatisfaction with the information provided [4].
For 75 (27%) patients, treatments were not available. This situation depended on several factors related to the COVID 19 pandemic: disruption of the treatment circuit, change in delivery time, increase in the number of patients than expected, increase in demand and a decrease in supply, etc.
205 (73%) were satisfied with their treatment. This may be related to proximity and means of travel to the retrocession unit.
Whatever the explanation, an improvement will have to be made to the dispensations currently carried out, for example through the acquisition of certain clinical pharmacy skills. For some patients, the care pathway is complex, constituting risk factors for disruption in the chain of care. This rupture is all the more problematic as these patients have rare and/or serious pathologies and that an interruption of treatment can be quickly deleterious.
From a pharmaceutical point of view, retrocessions are complex, because they are intended for patients who are often polymedicated because they are polypathological. On the other hand, dispensed drugs can be qualified as drugs at risk. This risk is increased when it comes to specialties under ATU status (sometimes little known and poorly documented) and often requiring enhanced monitoring and compliance with therapeutic use protocols (PUT).
Organization of the unit:
The quality approach exists at the retrocession unit, but needs improvement, which is why:
23 (8%) patients requested the installation of an identification plate of the retrocession unit in order to provide proper patient orientation.
195 (70%) patients were satisfied with the reception, cleanliness and quality of service delivery to the various patients in the retrocession unit.
44 (16%) wanted an increase in the number of pharmaceutical staff at the retrocession unit level in order to increase the operational capacity of the drug management of patients.
This low number of staff may be due to the reduction of all indoor pharmacy activities impacted by the COVID 19 pandemic in order to avoid the spread of the COVID 19 virus.
18 (6%) patients were not satisfied with the distribution of working hours in which there was no permanence or guard for the satisfaction of patients who lived very far away. Under normal conditions, retroceded drugs are dispensed for 1 to 6 months allowing patients very far away to access the different treatments. During this COVID 19 period, supply has been disrupted, very reduced and impacted in order to avoid the spread of the pandemic.
- Quality of therapeutic education:
Advice on proper use is an essential element for the patient. It optimizes adherence, improves tolerance and minimizes adverse effects.
58 (21%) patients did not accept the advice, because they are already used to their long-term treatment, 84 (30%) patients did not receive the advice of good use. In our unit, given the frequency of the number of patients received per day, it is practically difficult to take enough time for a single patient, 107 (38%) patients are satisfied with the quality of the advice of good use, 31 (11%) patients are not satisfied with the quality of the advice of good use.
- Break up:
The rupture may be partial or national. It concerned all the essential medicines dispensed in the retrocession unit.
In this study, 89 (32%) patients did not receive their treatment. The reason was simple, linked in particular to the disruption of the supply system, the distance between the patient and the retrocession, or the disruption at the national level following the closure of air borders.
- 8%) patients were satisfied with their treatment.
- Termination deadlines:
The break period can range from 7 days to 3 months per time more.
For 10 (10%) patients the rupture was national, for 02 (2%) patients the rupture time was 3 months, for 05 (5%) patients the rupture time was 2 months, for 42 (44%) patients the rupture time was 30 days,
For 02 (2%) patients the rupture time was 25 days, for 10 (11%) patients the rupture time was 20 days, for 16 (17%) patients the rupture time was 15 days, for 09 (9%) patients the rupture time was 07 days.
Conclusion
The results of our study show that patient satisfaction is based on effective reception and communication from the pharmaceutical team and the creation of a patient-pharmacist bond.
This study demonstrated a high satisfaction rate for both outpatients and inpatients.
References
- Taboulet F, Dulin R, Bonnin M, Saux MC. Hospital retrocession of medicines: what pharmaceutical service to the patient? Example of Aquitaine, 2004.
- Darcissac C, Duvert L, Hoegy D, Chappuy M, Pivot C, Janoly-Dumenil A. Risk analysis a priori in hospital retrocession units: focus on the dispensation process,
- Laoubi D, Hallouard F, Remy E, Leroy F, Bougle C, Monzat D, Bounoure F. Retrocession, a profitable but risky activity,
- Lattard C, Orsini C, Fuss D, Chenailler C, Varin H. Optimization of dispensations made by pharmacy preparers: Quality approach in retrocession, 2020.
- Guérin A, Lebel D, Maranbo N, Prot-Labarthe S, Bourdon O. Bussiéres JF. Determinants of the evolution of hospital pharmacy in France and Quebec: perception of hospital pharmacists,
- Brreton M, Demers E, Busssière JF. Roles and Impacts of Pharmaceutical Activities: Perceptions of Pharmacy Students, 2015.
- Jenniongs P, Lotito A, Baysson H, Pineau-Blode E, Berlioz J. Clinical pharmacy in a hospital setting: a satisfaction survey among prescribers, 2017.
- Roge M, Kramer L, Senhadj F, Moad M, Vanpoperinghe K, Menneglier B, et al. Return of medicines to the hospital: what are patients' expectations? 2018.
- Bouaiti E, Zidouh S, Boufaress A, Kessouati J, Mrabet M, BelyamaniL. Determining factors of the satisfaction of patients consulting in the emergency room of the Mohamed V military training hospital in Rabat, Morocco, 2016.
- Sarah LT, Stéphane H, Pierrick B, Emmanuelle F, Stéphane P, Patrick LG. Interest of the pharmaceutical file during the retrocession in a cancer center, 2018.
- http://www.omedit-normandie.fr/boite-a outils/rétrocession/retrocession.2541.2914.html.
- Nucci J, Le Roy C, Deville L, Madelaine I, Fontaine J-P, Touratier S. Place of the pharmaceutical file among the other sources available on the treatments of patients upon their arrival in the emergency room. Pharm Hosp Clin, 2017.
- Dupuis C, Flatres A, Chatron C, Muzard C, Hecquard C, Baveux R. Hospital retrocession or officinal dispensation: how to facilitate the referral of patients. Hopipharm, 2017.
- Le LMM, Reitter D, He S, Bonle FT, Launois A, Martinez D, et al. Safety analysis of occupational exposure of healthcare wor-kers to residual contaminations of cytotoxic drugs using FMECAsecurity approach. Sci Total Environ, 2017.
- Gridchyna I, Aulois-Griot M. The return of medicines by hospitals: what are the benefits for the actors? Med Law, 2011.
- Darcissac C, Duvert L, Hoegy D, Chappuy M, Pivot C, Janoly-Dumenil A. [Prospective risk analysis in a retrocession unit: Focus on drug dispensation process], 2020.
- Audrey Lehmann. Securing the return of drugs to the hospital: optimization of the dissemination of information. Pharmaceutical Sciences, 2006.
- French Society of Clinical Pharmacy. Memo Sheet – Pharmaceutical Interviews – SFPC [online], 2019.
- Contract for the Improvement of the Quality and Efficiency of Care. Decree No. 2017-584 of 20, 2017.

