A Rare Case of Traumatic Neuroma in the Tarsal Tunnel
David H Truong, DPM, MS*
Assistant Chief of Podiatry, Surgical Service - Podiatry Section, VA North Texas Health Care System, Dallas, Texas, USA
Assistant Professor of Orthopaedic Surgery, Department of Orthopaedic Surgery, University of Texas Southwestern Medical Center, Dallas, Texas, USA
Received Date: 17/01/2022; Published Date: 31/01/2022
*Corresponding author: David H Truong, DPM, MS, Assistant Chief of Podiatry, Surgical Service - Podiatry Section, VA North Texas Health Care System, Dallas, Texas, USA
Abstract
Traumatic neuroma is a pathological condition of the nerve after an injury. It is a rare entity, and its occurrence in the tarsal tunnel has not been reported in the literature. The condition causes a triad of symptoms: pain, paresthesia, and numbness. It can be debilitating since the symptoms commonly occur during ambulation and at night. Most are initially treated conservatively, with surgical intervention after six months of no improvement. However, surgical success rate highly varies, ranging from 44% to 91%, with diminished success rate the longer the symptoms persisted. We present a case of a 52-year-old male who sustained a puncture injury to his right ankle four years prior. Patient presented with pain in his medial right ankle with numbness and occasional radiating pain to the toes. After surgical excision of the lesion, patient regained sensation to his plantar foot and relief of pain. Pathology report confirmed a traumatic neuroma. This case demonstrates a rare incident of a traumatic terminal neuroma in the tarsal tunnel in which the patient regained sensation and maintain function after the procedure.
Keywords: entrapment neuropathy, nerve compression, soft tissue mass, tibial nerve, trauma
Introduction
Tarsal Tunnel Syndrome (TTS) is a condition that is caused by compression of the tibial nerve and its branches. It is a compressive neuropathy that can be caused by either intrinsic and/or extrinsic compression. Currently, there are no literature that evaluates the prevalence or incidence of traumatic neuromas in the tarsal tunnel. Over 80% of the cases can be diagnosed based on history and physical exam alone [1,2].
The earliest description of the syndrome was discussed by Kopell and Thompson in 1960 [3]. Keck and Lam introduced the term “tarsal tunnel syndrome” in 1962 [4,5]. The tarsal tunnel is a fibrous-osseous structure, consisting of the flexor retinaculum medially, tibia anteriorly, and the posterior process of the talus and calcaneus laterally. In the tunnel, the tibial nerve splits into three terminal branches: medial calcaneal nerve, Medial Plantar Nerve (MPN), and Lateral Plantar Nerve (LPN) - entrapment can occur at any of the branches. Davis and Schon found that the tibial nerve bifurcates within 2 cm of the medial malleolus in 90% of their cadaveric study [6].
TTS is a common pathology that foot and ankle specialists often see in their clinical setting. Electromyelography (EMG) and Nerve Conduction Studies (NCS) are common electrodiagnostic tests used for TTS workup. A positive result can confirm TTS, while a negative result does not exclude TTS. Petal et al. performed an evidence-based literature review of EMG and NCS in diagnosing TTS, and based on their findings, they are unable to determine the specificity and sensitivity of either test [7]. However, both EMG and NCS are beneficial in ruling out proximal entrapment neuropathy, but TTS remains a clinical diagnosis [2,8,9].
When symptoms persist for more than 6 months, surgical decompression may be warranted to relieve the symptoms and help induce neural repair [10]. However, ongoing symptoms for greater than one year, tend to have a lower success rate with surgical decompression [11,12]. Successful surgical treatment of TTS involves releasing all potential compression sites acting on the nerves. The success rate of Tarsal Tunnel Release (TTR) report varies from 44%-91% based on surgeon preference of TTR methods [1,2,9,12,13].
Currently, there are no literature that describes traumatic neuroma in the tarsal tunnel. We present a case report that demonstrates a successful surgical treatment of TTS secondary to a traumatic neuroma, in which the patient regained sensation after experiencing four years of paraesthesia in the foot.
Case Report
Patient is a 52-year-old healthy male who presented to the clinic with concerns of right ankle pain. He denies any major medical or surgical history, but had a significant smoking history, one pack per day for the past 32 years. Patient reported that he climbed a fence four years ago where he slipped, and the fence post penetrated his medial right ankle. At the time of injury, he presented to the Emergency Room (ER) immediately for an evaluation. Radiographs were negative for fracture; thus, the ER physician irrigated the wound and performed a primarily closure. Patient reported that he did not follow up with any specialist and over the next few months, the area developed a prominent lump and was beginning to cause him pain.
During patient first visit with the authors, he described the pain as a 5/10 that was located on the inside of his right ankle with occasional shooting pains and numbness to the toes. Physical exam revealed diminished Range of Motion (ROM), but no pain of the ankle and subtalar joints. Positive Tinel’s sign was present upon percussion of tibial nerve around the tarsal tunnel, radiographs were negative for acute fracture or dislocation, and only mild tibiotalar spurring was noted. A Magnetic Resonance Imaging (MRI) was ordered to evaluate the Posterior Tibialis (PT) tendon and tibial nerve.
On a subsequent visit, he reported that the pain has worsened to 9/10. He stated that he could no longer wear high top boots due to the pressure on the medial ankle and that any pressure to that area elicited electrical shock sensations to his toes.
MRI with and without contrast revealed a soft tissue mass at the inferior margin of the tarsal tunnel involving the MPN and a chronic high grade partial tear of the PT tendon and Flexor Digitorium Longus (FDL) tendon. The mass measured 1.4 x 0.9 x 1.7 cm (Figures 1, 2). At this time the authors suspected a traumatic neuroma given the patient history. Patient was scheduled for a right tarsal tunnel release, exploration and possible excision of neuroma, and debridement with repair of PT tendon.
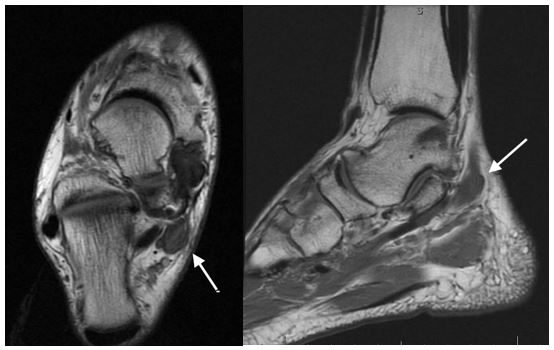
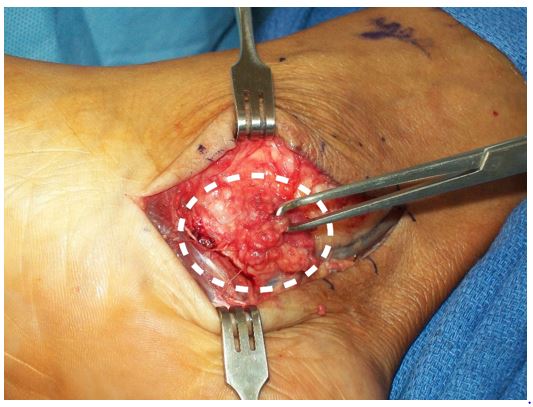
Figure 2: The dotted circle indicates the soft tissue mass/neuroma.
Intraoperatively, the authors observed that the MPN and PT tendon were fibrosed together to the deep fascial layer (Figure 3A). It was very difficult to differentiate between the two, as the two had form a large bulbous structure. After debridement of the fibrosed tissue and PT tendon, the MPN neuroma was identified and measured 2.6 x 1.0 x 1.5 cm (Figure 3B). The remaining tendon appeared healthy and was retubulized. Upon further dissection, the LPN and medial calcaneal nerve were identified and appeared normal (Figure 4).

Figure 3: A) The soft tissue mass adhered to the PT tendon dorsal to the neuroma. B) Neuroma visualized after debridement of PT tendon mass.
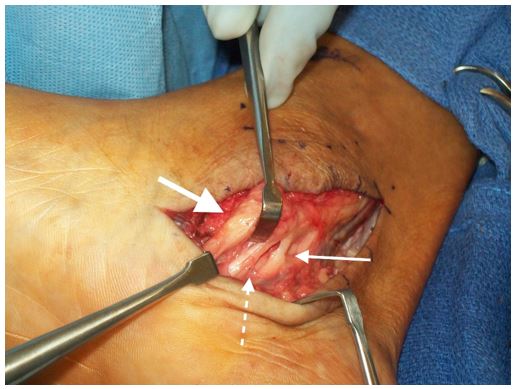
Figure 4: Medial calcaneal nerve (thin solid arrow). Lateral plantar nerve (dashed arrow). Medial plantar nerve (thick solid arrow).
A nerve stimulator was used intraoperatively to evaluate the MPN and LPN function (Figure 5). When the neuroma was stimulated distally with the nerve stimulator, motion of the hallux was noted; thus, confirming the neuroma involves the MPN. In contrast, when the LPN was stimulated, flexion of the lesser digits was noted. Upon further inspection, the neuroma was firm and had no vascular striations. At this time, the authors were able to remove the neuroma while keeping part of the MPN intact (Figure 6). The authors decided to excise the neuroma because it was significant in size and leaving it intact will only cause further compression of the nerve. After excision of the neuroma, the nerve stimulator was used once again to confirm intact motor function of the MPN. The MPN was then wrapped in a nerve wrap to help reduce inflammation and adhesion. The excised neuroma along with the excised tendon were sent to pathology, report was consistent with traumatic neuroma (Figure 7).
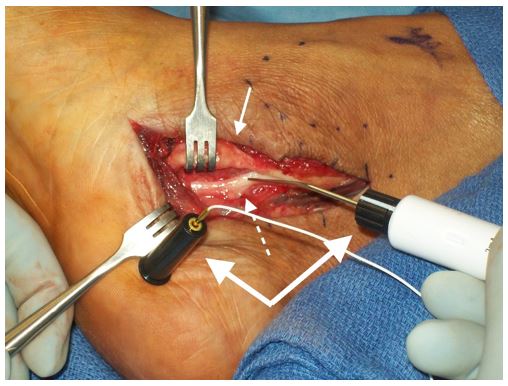
Figure 5: Nerve stimulator (thick solid arrow) used to confirm the lateral plantar nerve (dashed arrow) was not involved in the neuroma, and the neuroma (thin solid arrow) was part of the medial plantar nerve.
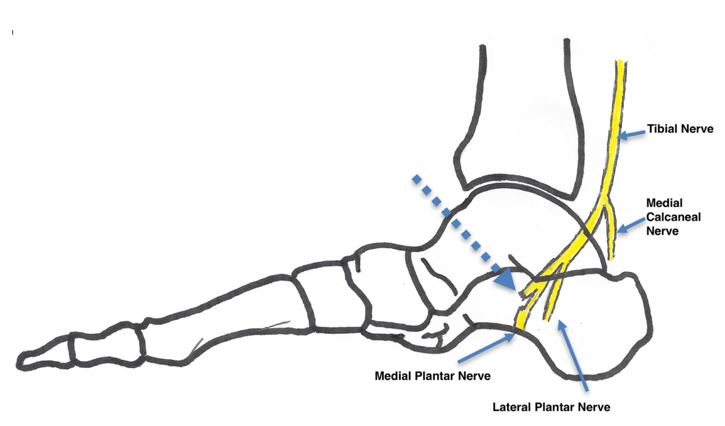
Figure 6: Author cartoon drawing of the damage to the medial plantar nerve and which portion was removed. The dashed arrow indicated the neuroma site that was excised. The authors believe that when the patient injured himself four years ago, the fence post severed part of the medial plantar nerve, causing a neuroma to develop.
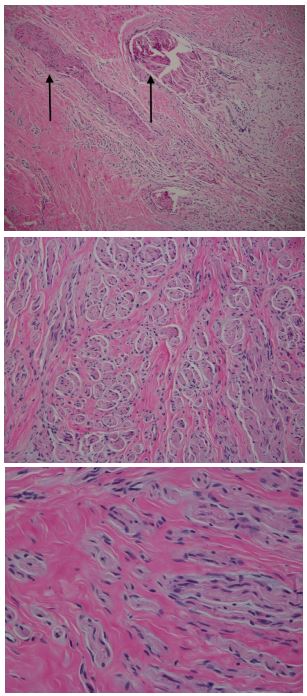
Figure 7: Histology sections reveal tissue with entrapped proliferated nerve twiglets. The histology is typical of a traumatic neuroma. A) 10x magnification: Entrapped nerve twiglets (solid arrows) are visible. B) 40x magnification: Cross-section of entrapped nerve twiglets. C) 100x magnification: Longitudinal section of entrapped nerve twiglet on magnification.
The patient was followed at 2-week post-operative and related that he had normal sensation on the bottom of his foot for the first time in years. The patient rated the pain a 5/10, but denied any sharp electrical sensations. Physical exam revealed negative Tinel’s sign. All sutures were removed at two weeks, and the patient began partial weight bearing in a controlled ankle motion walker.
The patient was followed at 1 month, and he reported that the sensation and pain continued to improve. He reported no numbness, tingling, or shooting pain. Patient was advanced to full weight bearing in regular shoe gear with arch support. Patient was briefly lost to follow up afterward.
At nine months follow-up visit, patient reported that at around five months after the surgery, he started experiencing pain in his right plantar foot, especially along the medial arch and heel. Patient described his pain consistent with post-static dyskinesia. He reported no discomfort in shoe gear at the surgical site. Upon physical examination, it was determined that patient had plantar fasciitis and conservative treatment was initiated. Patient also reported that his right foot plantar skin was becoming drier than the left. He was advised to start applying lotion to his feet. In addition, he had hypersensitivity over the incision site with direct palpation. His motor function was intact with a 4/5 muscle strength.
The patient was followed at 1 year, and he reported his plantar fasciitis pain has resolved, and he reported no pain in his feet. Patient stated that he had no numbness or hypersensitivity in the tarsal tunnel area, and he regained sensation to his right foot in areas that were numb prior to the surgery. Overall, the patient had a full recovery with sensation regained to the affected area.
Discussion
Traumatic neuroma is a rare pathology that commonly occurs secondary to direct trauma. It is a result of excessive repair and hyperplasia of the nerve, and thus, is not consider a tumour [14-17]. Traumatic neuromas can be classified into two categories: terminal and spindle neuromas.
Terminal neuromas occur after transection of the nerve. As the nerve repairs itself, the Schwann cells of the distal nerve will create a channel for the ingrowth of the proximal nerve. However, if the distance between the two nerves is significant, the growth will become bulbous-like [14,18-20].
Spindle neuromas occur due to chronic friction and inflammation or traction injury to a nerve. The chronic irritation causes the nerve to repair in a disorganized fashion, causing fusiform swelling [14,19-21]. Histopathology of both traumatic neuromas will show non-encapsulated, tangled masses formed by fibroblasts, endoneurial cells, perineurial cells, and Schwann cells [14,21].
To the authors’ best knowledge, this is the first reported case in the literature of a traumatic terminal neuroma in the tarsal tunnel. This case report is unique in the findings where the patient had regained sensation with mild motor function loss after a duration of four years versus in the literature with classic TTS, where the success rate, even with surgery, is diminished if not treated within a year. Patient was asymptomatic for five months after the surgery, then he developed plantar fasciitis in the right foot, which was resolved with conservative treatment. Patient regained sensation in areas that was previously numbed and experience no nerve pain at 1-year post-surgical intervention. The authors attributed this to the decompression of the nerve. However, the onset of xerosis after the procedure could suggest that there could be a degree of impaired underlying eccrine function after the excision of the neuroma. Despite this, the patient was able to carry out normal daily activities with no limitation.
The limitations of this report include the brief lost to follow up, the low number of subjects, and that an EMG and NCS was not performed prior to the surgery; thus, the authors are unable to evaluate the nerve functions post-operatively. This limits the authors ability to evaluate whether the nerve functions improve after the decompression. In addition, because the patient did not follow up with any specialist, it is difficult to determine whether the neuroma has been present or gradually developed over four years after injury. This itself can change the treatment outcome.
This case report is unique in that the patient was able to regain sensation to the affected area after sustaining a nerve injury four years prior. This suggests that the duration of nerve injury may not play as significant of a role as in nerve regeneration as we initially thought. The degree of nerve damage seems to be the major factor in this case. More future studies evaluating the duration and degree of nerve injury are needed to establish the relationship between the duration of nerve damage and its repair.
Disclosure: None
Conflict of Interest: None
References
- Antoniadis G, Scheglmann K. Posterior tarsal tunnel syndrome: Diagnosis and treatment. Dtsch Arztebl Int, 2008; 105(45): 776-781.
- Bailie DS, Kelikian AS. Tarsal tunnel syndrome: Diagnosis, surgical technique, and functional outcome. Foot Ankle Int, 1998; 19(2): 65-72.
- Kopell HP, Thompson WA. Peripheral entrapment neuropathies of the lower extremity. N Engl J Med, 1960; 262: 56-60. doi: 10.1056/NEJM196001142620202 [doi].
- Keck C. The tarsal tunnel syndrome. J Bone Joint Surg Am, 1962; 44: 180-182.
- Lam SJ. Tarsal tunnel syndrome. J Bone Joint Surg Br, 1967; 49(1): 87-92.
- Davis TJ, Schon LC. Branches of the tibial nerve: Anatomic variations. Foot Ankle Int, 1995; 16(1): 21-29. doi: 10.1177/107110079501600105.
- Patel AT, Gaines K, Malamut R, Park TA, Toro DRD, Holland N. Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: An evidence-based review. Muscle Nerve, 2005; 32(2): 236-240. doi: 10.1002/mus.20393.
- Skalley TC, Schon LC, Hinton RY, Myerson MS. Clinical results following revision tibial nerve release. Foot Ankle Int, 1994; 15(7): 360-367.
- Pfeiffer WH, Cracchiolo A. Clinical results after tarsal tunnel decompression. J Bone Joint Surg Am, 1994; 76(8): 1222-1230.
- Ducic I, Felder JM, 3rd. Tibial nerve decompression: Reliable exposure using shorter incisions. Microsurgery, 2012; 32(7): 533-538. doi: 10.1002/micr.21987.
- Baba H, Wada M, Annen S, Azuchi M, Imura S, Tomita K. The tarsal tunnel syndrome: Evaluation of surgical results using multivariate analysis. Int Orthop, 1997; 21(2): 67-71.
- Sammarco GJ, Chang L. Outcome of surgical treatment of tarsal tunnel syndrome. Foot Ankle Int, 2003; 24(2): 125-131.
- El Shazly O, El Shazly A, Desouky A, El Zohiery AK, Sakr HM. Anatomical bases of endoscopic tarsal tunnel release: Anatomical and ultra-sonographic study with a preliminary clinical report. Surg Radiol Anat, 2011; 33(10): 929-936.
- Kang J, Yang P, Zang Q, He X. Traumatic neuroma of the superficial peroneal nerve in a patient: A case report and review of the literature. World J Surg Oncol, 2016; 14(1): 6.
- Yabuuchi H, Kuroiwa T, Fukuya T, Tomita K, Hachitanda Y. Traumatic neuroma and recurrent lymphadenopathy after neck dissection: Comparison of radiologic features. Radiology, 2004; 233(2): 523-529.
- Rainsbury JW, Whiteside OJ, Bottrill ID. Traumatic facial nerve neuroma following mastoid surgery: A case report and literature review. J Laryngol Otol, 2007; 121(6): 601-605.
- Lee EJ, Calcaterra TC, Zuckerbraun L. Traumatic neuromas of the head and neck. Ear Nose Throat J, 1998; 77(8): 676.
- Boutin RD, Pathria MN, Resnick D. Disorders in the stumps of amputee patients: MR imaging. AJR Am J Roentgenol, 1998; 171(2): 497-501.
- Donnal JF, Blinder RA, Coblentz CL, Moylan JA, Fitzpatrick KP. MR imaging of stump neuroma. J Comput Assist Tomogr, 1990; 14(4): 656-657.
- Provost N, Bonaldi VM, Sarazin L, Cho KH, Chhem RK. Amputation stump neuroma: Ultrasound features. J Clin Ultrasound, 1997; 25(2): 85-89.
- Ashkar L, Omeroglu A, Halwani F, Alsharif S, Loutfi A, Mesurolle B. Post-traumatic neuroma following breast surgery. Breast J, 2013; 19(6): 671-672.

