Complete Heart Block in Patient with Acute Coronary Syndrome due to Ticagrelor
Rutvik Trivedi*, Khanjan Shah, Dhruve Upadhyay
Department of Cardiology, Zydus hospital, India
Received Date: 16/10/2021; Published Date: 17/11/2021
*Corresponding author: Rutvik Trivedi, Department of Cardiology, Zydus hospital, India
Abstract
Ticagrelor has been advised as a first line therapy in combination with aspirin in patients with acute coronary syndrome. Ticagrelor being the only direct acting P2Y12 inhibitor also possesses better platelet inhibition with rapid onset of action. Although reported rarely, ticagrelor causes conduction abnormality in some patients. The exact mechanism for such is unknown. Here, we present a case of a 50-year-old male who was diagnosed with total occlusion of left anterior descending artery treated with primary percutaneous coronary intervention, later developed conduction abnormality while on ticagrelor therapy.
Keywords: Acute coronary syndrome; Complete heart block; Ticagrelor
Introduction
The exposed atherosclerotic plaque in the coronary artery activate the platelets which ultimately results in Acute Coronary Syndrome (ACS), atherothrombosis and acute ischemic stroke [1]. Aspirin in combination with a P2Y12 inhibitor, Dual Antiplatelet Therapy (DAPT), is a standard of care in patients with ACS with or without ST-segment elevation [2]. Clopidogrel has been the standard of care until newer and more potent P2Y12 inhibitors were beneficial in term decreasing the rate of ischemic events [3,4]. Of the clopidogrel, prasugrel and ticagrelor, the former two are prodrugs and need to undergo enzymatic activation. However, ticagrelor binds to receptor reversibly and acts directly without undergoing enzymatic metabolism. In addition to that, ticagrelor has rapid onset of action as it does not require hepatic activation post gastrointestinal absorption and has higher degree of platelet inhibition [5]. Considering these qualities, ticagrelor is endorsed as first-line agent in patients with ACS and scrutinised extensively.
Here, we have a unique case of a complete heart block in patient who had successful revascularization of his culprit lesion, secondary to ticagrelor treatment.

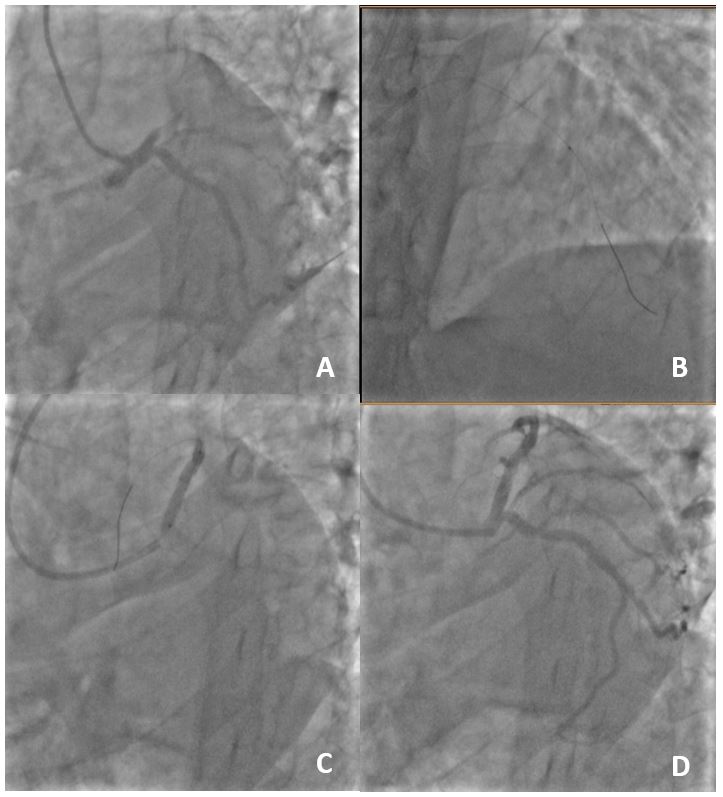
Figure 2: (A) Angiogram of left artery revealed proximal of LAD total occlusion with heavy thrombus burden (B) Thrombus suction is done (C) Negotiating & deploying of Ultimaster stent 3.5 x 28 (D) Final post stent TIMI flow
Case Report
A 50-year-old male presented to our facility in emergency department with complaints of breathlessness since last three hours. He had a known history of hypertension and denied any history of diabetes mellitus. On arrival, his heart rate was 137 beats/min, blood pressure was 170/110 mmHg and blood oxygen saturation on room air was 80%. He was initially suspected to be covid-19 positive. However, he was afebrile on presentation and also denied any history of coughing. Furthermore, he reported history of chest pain and epigastric pain since morning. He was tested negative on covid-19 rapid antigen testing kit. His echocardiography showed 30% left ventricular ejection fraction and hypokinesia in the left anterior descending region.
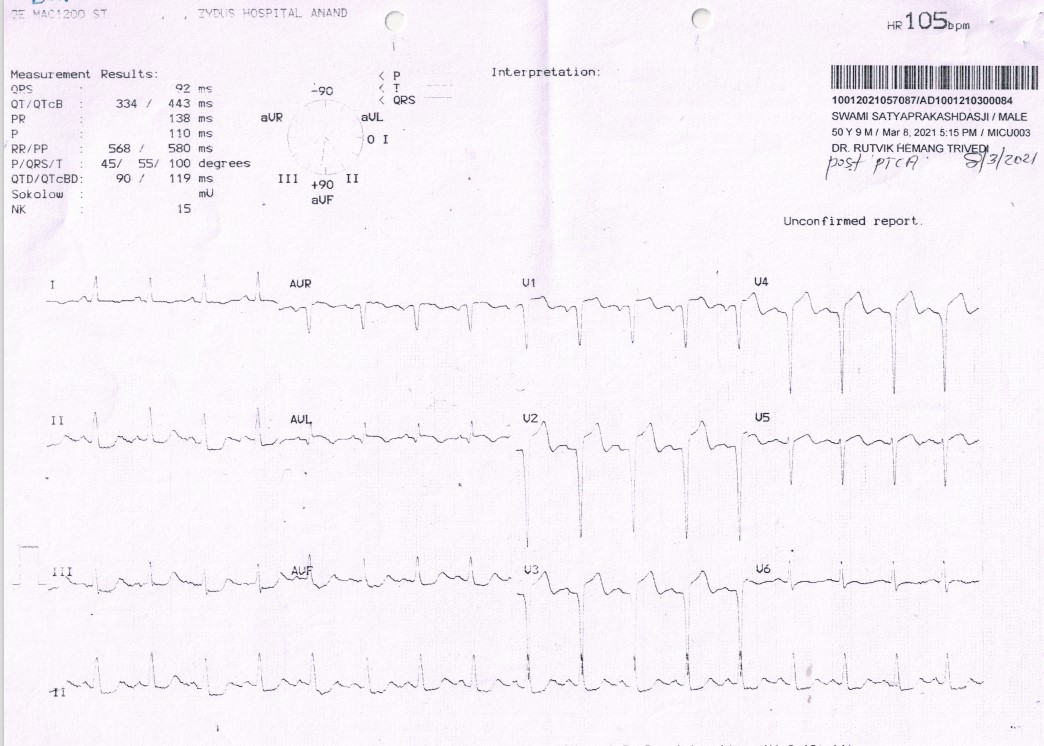
Considering his blood oxygen saturation levels, he was put on Bipap support and his electrocardiogram (ECG) showed anterior wall myocardial infarction (Figure 1). His blood oxygen saturation levels improved with bipap support. Patient was given 180 mg ticagrelor and 300 mg aspirin. He was put on nitroglycerine drip and was advised for coronary angiography. His angiography revealed normal right coronary artery and left circumflex artery. Total occlusion with heavy thrombus burden was observed in proximal left anterior descending artery (LAD) (Figure 2A). After thrombus suction (Figure 2B), the lesion was predilated with a short length balloon. A 3.5 x 28 mm sirolimus-eluting stent (Ultimaster [Terumo, Tokyo, Japan]) was negotiated in the lesion and deployed (Figure 2C). The lesion was postdilated with a 4 x 12 mm balloon. Final check shoot showed TIMI III flow with no residual stenosis (Figure 2D). His chest discomfort was relieved post percutaneous coronary intervention (PCI). Post PCI, his ECG showed >50% resolution in ST segment (Figure 3). He tolerated the procedure well in the first 24 hours.
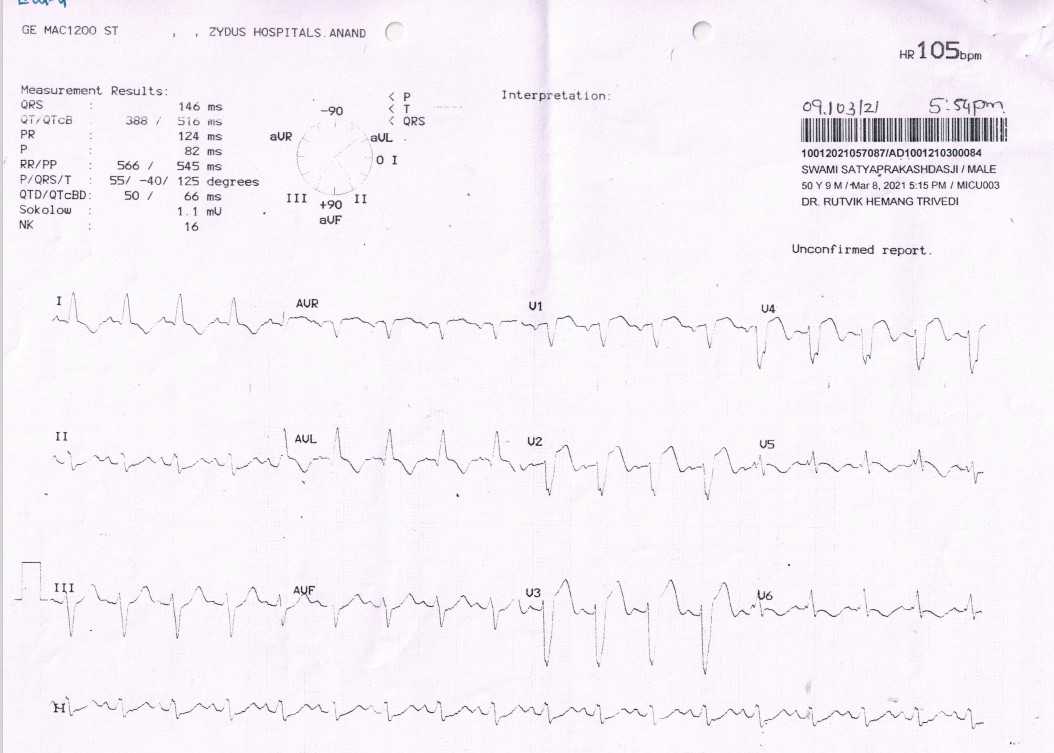
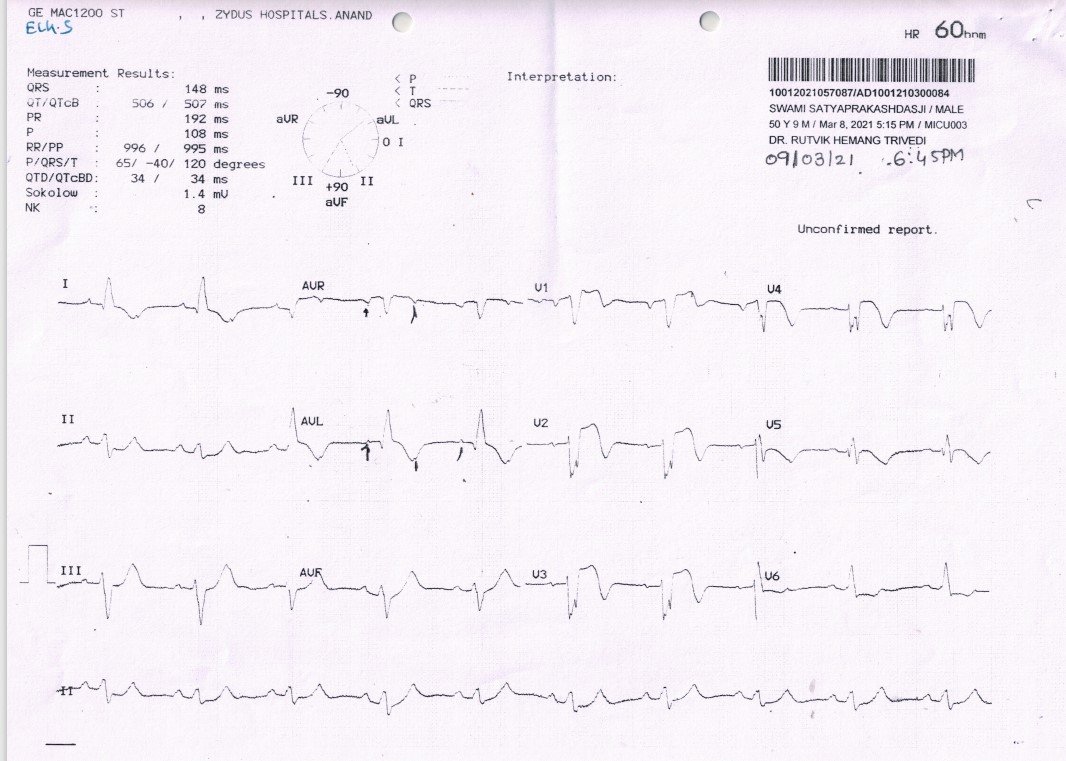
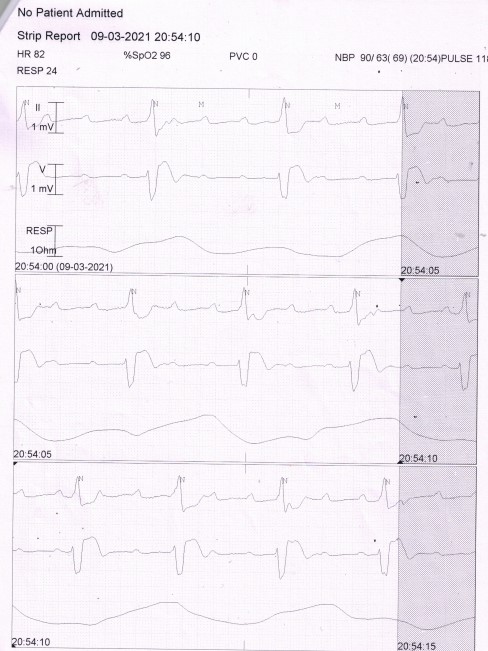
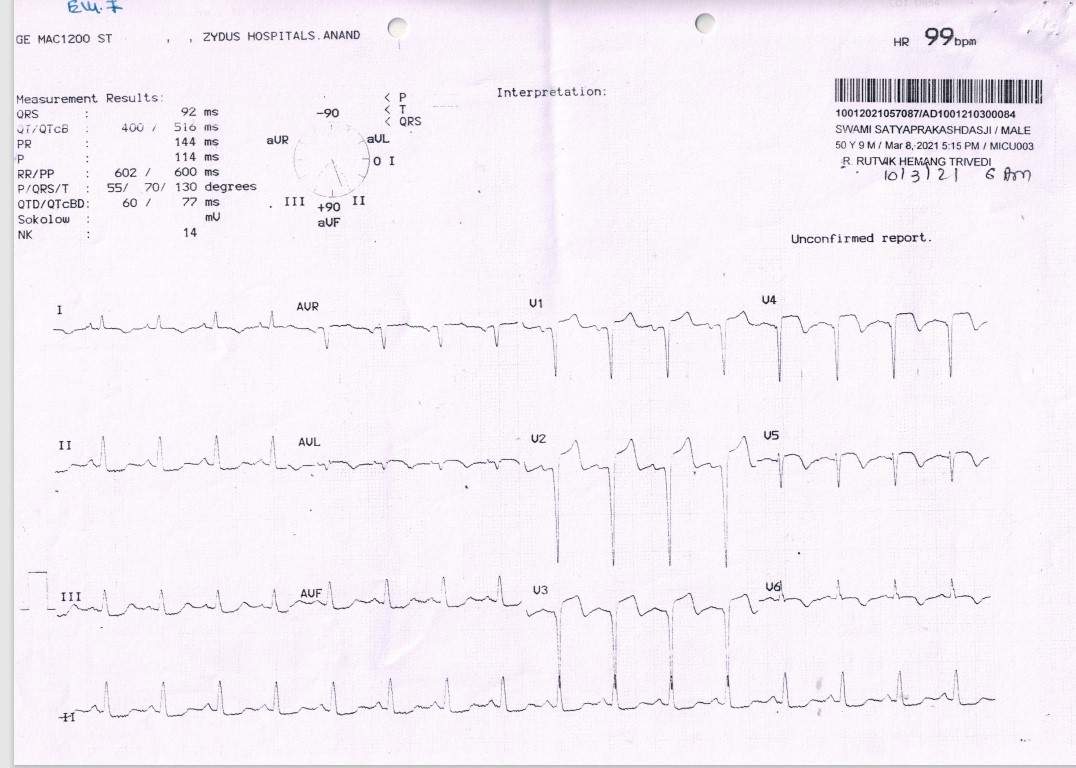
On the next day, he was taken off the Bipap support, his morning electrolytes and ABG were in normal range. Later that day around 5 pm, he complained of giddiness with some perspiration. His ECG was taken immediately which showed, normal sinus rhythm with new onset Left Bundle Branch Bock (LBBB) with QRS interval of 146 ms and PR interval was 124 ms (Figure 4). We did his check angiography which showed flowing stent. Post angiography after 30 min, He again had giddiness and felt transient loss of consciousness. His ECG showed LBBB bradycardia with heart rate of 57/min and had transient, 2:1 AV block pattern on the monitor. which immediately reverted to normal sinus rhythm with LBBB (Figure 5). We suspected that, the use of ticagrelor might have caused the conduction abnormality, Hence, he was switched from ticagrelor to prasugrel. He was closely monitored in the coronary care unit, and, we also planned to do temporary pacing if needed. Patient had episode of complete heart block for a duration of about 10 seconds at night which was reverted with intravenous use of Theophylline (5mg/kg) (Figure 6). On the next day, his ECG showed NSR and resolution of LBBB (Figure 7). He was continued on prasugrel and was discharged after 48 hours of uneventful observation.
Discussion
Here, we presented a case of a 50-year-old male with coronary artery disease who underwent percutaneous coronary intervention eventually developed complete heart block subsequent to ticagrelor therapy. The landmark PLATO trial also reported incidents of ventricular pauses in patients on ticagrelor treatment. However, it was believed that it was not clinically significant [6]. In the past, several cases have also reported conduction disorders in patients post ticagrelor therapy [7-12]. The European society of cardiology has recommended use of ticagrelor in DAPT treatment approach in patients with acute coronary syndrome [13]. However, a recent study comparing ticagrelor and prasugrel in patients with or without ST-elevation myocardial infarction reported significantly better outcomes in the prasugrel arm compared to the ticagrelor arm [14]. In the present case, patient suffered LBBB followed by 2:1 AV block and later complete heart block for duration of 10 s was observed in the ECG while on ticagrelor therapy. Clopidogrel can be prescribed to patients if ticagrelor of prasugrel are contraindicated. Ticagrelor has proven superiority over clopidogrel in patients with ACS. Thus, the patient was switched to prasugrel.
A theory suggests that the sinoatrial and atrioventricular nodes are affected by increased tissue concentration of adenosine. Interference due to ticagrelor causes inhibition of adenosine uptake by blood cells which eventually increases adenosine concentration [15]. This is a proposed theory and the exact mechanism of ticagrelor-induced bradycardia is unknown. Ticagrelor has dyspnoea (10-15 %) and bradycardia as most common side effects. Bradycardia with ventricular pauses for 3 s has been reported in around 6% patients during the first week of treatment while pauses more than 5 s is reported in only 2% of patients. In present case also, the patient showed declined heart rate (57 beats/min from 105 beats/min) secondary to ticagrelor therapy.
Conclusion
Bradycardia and severe form of conduction abnormalities can occur with the use of ticagrelor, although transient, but may require close observation and meticulous management. Immediate discontinuation and its replacement with another P2Y12 inhibitor with additional (optional) use of theophylline derivatives generally reverts the bradyarrhythmia episodes.
Acknowledgment: None
Conflicts of interest: None
References
- Linden MD, Jackson DE. Platelets: pleiotropic roles in atherogenesis and atherothrombosis. The international journal of biochemistry & cell biology. 2010; 42(11): 1762-1766.
- Sharma M, Mascarenhas DA. Ticagrelor associated heart block: the need for close and continued monitoring. Case reports in cardiology, 2017.
- Wallentin L, Becker RC, Budaj A, Cannon CP, Emanuelsson H, Held C, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. New England Journal of Medicine, 2009; 361(11): 1045-1057.
- Wiviott SD, Braunwald E, McCabe CH, Montalescot G, Ruzyllo W, Gottlieb S, et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. New England Journal of Medicine, 2007; 357(20): 2001-2015.
- Dobesh PP, Oestreich JH. Ticagrelor: pharmacokinetics, pharmacodynamics, clinical efficacy, and safety. Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy, 2014; 34(10): 1077-1090.
- Scirica BM, Bansilal S, Davoudi F, Armstrong PW, Clare RM, Schulte PJ, et al. Safety of ticagrelor in patients with baseline conduction abnormalities: a PLATO (Study of Platelet Inhibition and Patient Outcomes) analysis. American heart journal, 2018; 202: 54-60.
- Baker NC, Nadour W, Friehling M. Clinically significant ticagrelor induced conduction abnormalities following percutaneous coronary intervention. International journal of cardiology, 2016; 214: 21-22.
- Goldberg A, Rosenfeld I, Nordkin I, Halabi M. Ticagrelor therapy in patients with advanced conduction disease: is it really safe? International journal of cardiology, 2016; 202: 948-949.
- Nicol M, Deblaise J, Choussat R, Dubourg O, Mansencal N. Side effects of ticagrelor: sinus node dysfunction with ventricular pause. International journal of cardiology, 2015; 191: 56-77.
- Ozturk C, Unlu M, Yildirim AO, Erdogan S, Demir M, Balta S, et al. The progressed atrioventricular block associated with ticagrelor therapy may not require permanent pacemaker after acute coronary syndrome; it may be reversible. International journal of cardiology, 2016; 203: 822-824.
- Goldberg A, Rosenfeld I, Nordkin I, Halabi M. Life-threatening complete atrioventricular block associated with ticagrelor therapy. International journal of cardiology, 2015; 182: 379-380.
- Ünlü M, Demirkol S, Yildirim AO, Balta Ş, Öztürk C, Iyisoy A. Atrioventricular block associated with ticagrelor therapy may require permanent pacemaker. International journal of cardiology. 2016; 202: 946-947.
- Valgimigli M, Bueno H, Byrne RA, Collet J-P, Costa F, Jeppsson A, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. European journal of cardio-thoracic surgery, 2018; 53(1): 34-78.
- Schüpke S, Neumann F-J, Menichelli M, Mayer K, Bernlochner I, Wöhrle J, et al. Ticagrelor or prasugrel in patients with acute coronary syndromes. New England Journal of Medicine, 2019; 381(16): 1524-1534.
- Waldmann V, Laredo M, Nigam A, Khairy P. Cyclical sinus bradycardia and atrioventricular block induced by ticagrelor. HeartRhythm case reports, 2018; 4(11): 527.

