Metabolic Profiles differences of Overweight Patients on Olanzapine, Clozapine and Risperidone
Siew Fai Liew* and Bhanu Gupta
Department of General Psychiatry, Institute of Mental Health, Singapore
Received Date: 14/08/2021; Published Date: 06/09/2021
*Corresponding author: Siew Fai Liew, Department of General Psychiatry, Institute of Mental Health, 10 Buangkok View, Buangkok Green Medical Park, Singapore, 539747
Abstract
Aim: We set out to examine the differences in metabolic profiles of at risk (overweight) patients across commonly used atypical antipsychotics (Olanzapine, Risperidone, Clozapine). We hypothesized that Olanzapine and Clozapine group will have more metabolic abnormalities compared to Risperidone.
Methods: This study is based on the data of 67 subjects who were recruited into a 12-week open-labelled trial looking at the effects of adjunctive Aripiprazole in atypical antipsychotics for weight reduction and improvement in metabolic profile. Metabolic profiles including weight, waist circumference, fasting blood glucose, HbA1c, serum total, HDL and LDL cholesterol levels and triglycerides were measured at baseline. The measurements were then compared across the different subgroups of atypical antipsychotics (Olanzapine, Risperidone, Clozapine). The definition of metabolic syndrome proposed by the Third Report of the National Cholesterol Education Program (National Institutes of Health, United States) Expert Panel (Adults Treatment Panel III) was used.
Results: The atypical antipsychotics were grouped into Olanzapine (n=27), Risperidone (n=24) and Clozapine (n=16). More than 50% of clozapine-treated and Olanzapine-treated overweight patients were demonstrated to have metabolic syndrome at baseline. There was a statistically significant difference in serum triglycerides (p=0.012), LDL (p= 0.046) and HbA1c (p=0.045) across the three groups as demonstrated by one-way ANOVA. A Tukey post hoc test showed that both the Olanzapine (p=0.032) and Risperidone (p=0.013) groups demonstrated statistically significant lower serum triglycerides when compared to Clozapine. Interestingly, the mean serum HbA1c was significantly lower in Clozapine when compared to Olanzapine group (p=0.045), perhaps reflecting the closer monitoring of fasting blood sugar in clozapine patients. When controlled for age and BMI, the significant differences in serum triglycerides remain between Clozapine and Risperidone groups [but not for serum HbA1c]. There were no statistically significant differences across the groups with respect to other metabolic parameters.
Conclusion: At baseline, metabolic dysregulation was demonstrated in all subgroups of overweight patients. As hypothesized, patients on Olanzapine and Clozapine groups fared worse than Risperidone. Further studies examining long term effects of atypical antipsychotics in a larger sample of patients are warranted to confirm these findings. These findings have clinical significance in terms of choosing the first antipsychotic for drug naïve patients or where there is no clinically significant difference in efficacy.
Keywords: Atypical antipsychotics; Differences; Metabolic profiles; Overweight
Introduction
Overweight and obesity are associated with abnormal metabolic changes such as insulin resistance and dyslipidemia which themselves are risk factors for cardiovascular diseases. Cardiovascular diseases remain the leading cause of morbidity and mortality among people with schizophrenia. It has also been associated with a more than 3-fold increase in mortality associated with cardiovascular causes. Their life span is shortened by 20 years when compared to general population because of premature cardiovascular disease. Since the introduction of atypical antipsychotics, there is cumulative evidence of their association with metabolic abnormalities. Young, neuroleptic naïve patients with lower baseline body mass index are particularly vulnerable and the effects are most applicable in the first week of treatment [1]. Clozapine and Olanzapine are known to constitute the highest metabolic risks amongst atypical antipsychotics.
Purpose of the Present Study
We set out to examine the differences in metabolic profiles of at risk (overweight) patients across commonly used atypical antipsychotics (Olanzapine, Risperidone, Clozapine). We hypothesized that Olanzapine and Clozapine will have more metabolic abnormalities compared to Risperidone.
Method
The study was reviewed and approved by NHG DSRB and HSA and was conducted in accordance with the ethical principles that have their origin in the Declaration of Helsinki and that are consistent with the Singapore Good Clinical Practice and the applicable regulatory requirements.
This study is based on the data of 67 subjects who were recruited into a 12-week open-labelled trial looking at the effects of adjunctive Aripiprazole in atypical antipsychotics for weight reduction and improvement in metabolic profile. Eligible patients were selected for the study if they: (1) aged between 21 and 65 years old, (2) with diagnoses of Schizophrenia or schizoaffective disorder, (3) On stable doses of atypical antipsychotics, either Olanzapine, Clozapine, or Risperidone for at least 1 month, (4) not on other concomitant medications. Patients can be on antipsychotic polypharmacy, but there should not be more than 1 of the above 3 atypical antipsychotics in a single prescription, (5) able to provide written informed consent, and (6) with a BMI ≥ 25 (Overweight) and/or ≥7% increase in weight from pre-antipsychotic treatment.
The exclusion criteria included: patients with allergy to Aripiprazole/contraindication to use of Aripiprazole, mental retardation, current substance misuse, eating disorder, any major or unstable medical or neurological illness, severe personality disorder, serious suicidal thoughts, who are pregnant or breastfeeding, use of any medication for weight loss within the past one month to the study entry, clinically significant abnormalities in physical examinations, ECG or lab assessments, baseline BMI < 18.5kg/m2 (cut-off point for underweight adults as per WHO guidelines) and who are unable to read or speak English.
We set out to examine the differences in metabolic profiles of at risk (overweight) patients across commonly used atypical antipsychotics (Olanzapine, Risperidone, Clozapine). We hypothesized that Olanzapine and Clozapine group will have more metabolic abnormalities compared to Risperidone. Metabolic profiles including weight, waist circumference, fasting blood glucose, HbA1c, serum total, HDL and LDL cholesterol levels and triglycerides were measured at baseline. The measurements were then compared across the different subgroups of atypical antipsychotics (Olanzapine, Risperidone, Clozapine). The definition of metabolic syndrome proposed by the Third Report of the National Cholesterol Education Program (National Institutes of Health, United States) Expert Panel (Adults Treatment Panel III) was used. Data were analyzed using the Statistical Package for Social Sciences, version 22 (SPSS Inc, Chicago, Illinois).
Results
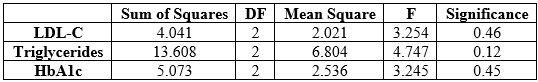
Table 1 presents the demographics and baseline characteristics of the participants of the study. The atypical antipsychotics were grouped into Olanzapine (n=27), Risperidone (n=24) and Clozapine (n=16). More than 50% of clozapine-treated and Olanzapine-treated overweight patients were demonstrated to have metabolic syndrome at baseline. There was a statistically significant difference in serum triglycerides (p=0.012), LDL (p= 0.046) and HbA1c (p=0.045) across the three groups as demonstrated by one-way ANOVA (Table 2). A Tukey post hoc test showed that both the Olanzapine (p=0.032) and Risperidone (p=0.013) groups demonstrated statistically significant lower serum triglycerides when compared to Clozapine. Interestingly, the mean serum HbA1c was significantly lower in Clozapine when compared to Olanzapine group (p=0.045), perhaps reflecting the closer monitoring of fasting blood sugar in clozapine patients. When controlled for age and BMI, the significant differences in serum triglycerides remain between Clozapine and Risperidone groups [but not for serum HbA1c]. There were no statistically significant differences across the groups with respect to other metabolic parameters.
Table 1: Baseline Demographic and Clinical Characteristics of The Study Sample.
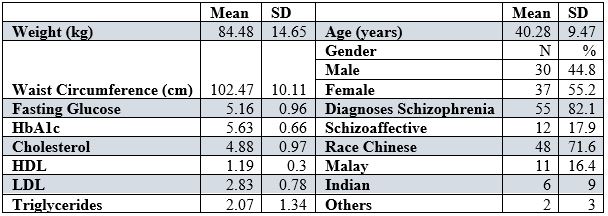
Table 2: One-way ANOVA demonstrating differences in serum LDL-C, Triglycerides and HbA1c across three groups.
Discussion
The results of the study demonstrated that clozapine and olanzapine constitute the highest metabolic risks compared to other atypical antipsychotics. Of note, the differences in serum triglycerides remained significant between Clozapine and Risperidone groups after controlled for age and BMI.
The results of this study are consistent with previous studies [1-5]. In a systematic review done which included 48 studies, Clozapine is shown to produce the most weight gain whereas Olanzapine is shown to produce more increase in serum cholesterol and glucose as compared to other second-generation antipsychotics [6].
According to Asenjo Lobos et al., 2010, weight gain resulted from clozapine usage was not seen with risperidone [7]. A statistically significant result (≥7% increase in body weight from baseline) was reported for Clozapine, Olanzapine, Risperidone and other antipsychotics by Alonso Pedrero et al., 2010 [8]. In terms of weight gain side effects, olanzapine was worse than all other compared to non-clozapine SGAs, and risperidone was significantly worse than several other SGAs [9]. A review paper by Hirsch et al., 2017 demonstrated that clozapine and olanzapine were most consistently strongly associated with metabolic effects like type 2 diabetes mellitus but however the evidence was mixed for risperidone [3]. Another network meta-analysis showed that olanzapine caused more gains in weight and body mass index (BMI) than other SGAs except for clozapine in the short term [10].
Another comprehensive review paper which considers the evidence for and against an association between glucose or lipid dysregulation and eight separate second-generation antipsychotics currently available in the US and/or Europe compare the mean weight changes and relative percentages of patients experiencing specific levels of weight increase from controlled, randomized clinical trials [4]. The results are aligned with the results from previous studies that clozapine and olanzapine were most consistently strongly associated with metabolic effects such as diabetes mellitus and dyslipidemia.
As for dyslipidemia, the association with dyslipidemia was found in clozapine (odds ratio 1.26, 95% confidence interval 1.16-1.38), olanzapine (odds ratio 1.29, 95% confidence interval 0.89-1.87) and risperidone (odds ratio 1.05, 95% confidence interval 0.80-1.37) compared with first-generation antipsychotics, but heterogeneity was high (all I2 > 50%, p < 0.05). Clozapine was found to be associated with increased triglycerides (standardized mean difference = 0.51, 95% confidence interval 0.21-0.81, I2 = 5.74%), but not with cholesterol [11].
The etiology and mechanism by which schizophrenia patients are susceptible to cardiometabolic disorders are complex which include the interplay between the environmental factors (psychosocial and socioeconomic risk factors, lifestyle, antipsychotics adverse effects) and genetic vulnerabilities. These further explained the importance of choosing the first antipsychotics in our patients after careful consideration and optimal balance of the risk of metabolic side effects against the efficacy.
There is other several limitations for this study. First, the sample size is small and the study duration is short. In addition, concurrent medications like mood stabilizers or antidepressants usage may have contributed to weight gain side effects albeit subjects will be withdrawn from the study if there are any changes to the medication dosages. Furthermore, dietary and lifestyle changes (exercises) are potential confounders for the subjects’ metabolic profiles. Last but not least, this is an open-labelled study which lacks randomization, placebo controls and blinding. We believe that the findings from this study will provide the necessary preliminary evidences for further randomized control trials.
Conclusion
At baseline, metabolic dysregulation was demonstrated in all subgroups of overweight patients. As hypothesized, patients on Olanzapine and Clozapine groups fared worse than Risperidone. Further studies examining long term effects of atypical antipsychotics in a larger sample of patients are warranted to confirm these findings. These findings have clinical significance in terms of choosing the first antipsychotic for drug naïve patients or where there is no clinically significant difference in efficacy.
Author Note
We have no conflicts of interest to disclose.
References
- Musil R, Obermeier M, Russ P, Hamerle M. Weight gain and antipsychotics: a drug safety review. Expert opinion on drug safety. 2015; 14(1): 73–96.
- Hasnain M, Vieweg WV, Hollett B. Weight gain and glucose dysregulation with second-generation antipsychotics and antidepressants: a review for primary care physicians. Postgraduate medicine. 2012; 124(4): 154–167.
- Hirsch L, Yang J, Bresee L, Jette N, Patten S, Pringsheim T. Second-Generation Antipsychotics and Metabolic Side Effects: A Systematic Review of Population-Based Studies. Drug safety. 2017; 40(9): 771–781.
- W NJ. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS drugs. 2005; 19 Suppl 1: 1–93.
- Smith RC, Leucht S, Davis JM. Maximizing response to first-line antipsychotics in schizophrenia: a review focused on finding from meta-analysis. Psychopharmacology. 2019; 236(2): 545–559.
- Rummel-Kluge C, Komossa K, Schwarz S, Hunger H, Schmid F, Lobos CA, et al. Head-to-head comparisons of metabolic side effects of second-generation antipsychotics in the treatment of schizophrenia: a systematic review and meta-analysis. Schizophrenia research. 2010; 123(2–3): 225–233.
- Asenjo Lobos C, Komossa K, Rummel-Kluge C, Hunger H, Schmid F, Schwarz S, et al. Clozapine versus other atypical antipsychotics for schizophrenia. Cochrane Database Syst Rev. 2010; 11: CD006633.
- Alonso-Pedrero L, Bes-Rastrollo M, Marti A. Effects of antidepressant and antipsychotic use on weight gain: A systematic review. Obes Rev. 2019; 20(12): 1680–1690.
- Kishimoto T, Hagi K, Nitta M, Kane JM, Correll CU. Long-term effectiveness of oral second-generation antipsychotics in patients with schizophrenia and related disorders: a systematic review and meta-analysis of direct head-to-head comparisons. World Psychiatry. 2019; 18(2): 208–224.
- Pillay J, Boylan K, Carrey N, Newton A, Vandermeer B, Nuspl M, et al. First- and Second-Generation Antipsychotics in Children and Young Adults. Systematic Review Update, 2017.
- Buhagiar K, Jabbar F. Association of first- vs. Second-generation antipsychotics with lipid abnormalities in individuals with severe mental illness: A systematic review and meta-analysis. Clin Drug Investig. 2019; 39(3): 253–73.

