Challenges in Management of Soft Tissue Defect in Type III Open Tibia and Fibular Fractures at the Jos University Teaching Hospital–A Ten Year Review
Mancha DG¹,*, Ode MB¹, Amupitan I¹, Onche II¹ and AkintayoAJ²
¹Department of Orthopedics and Traumas, Jos University Teaching Hospital Jos, Plateau State, Nigeria
²Plastic Surgery Unit, Department of Surgery, Jos University Teaching Hospital Jos, Plateau State, Nigeria
Received Date: 19/07/2021; Published Date: 06/08/2021
*Corresponding author: Dr. Mancha DG, Department of Orthopedics, Jos University Teaching Hospital Jos, P.M.B. 2076 Jos, Plateau State, Nigeria
Abstract
Background: Soft tissue injuries impose additional challenge to fracture management due to high risks of infection. Adequate skin cover, early immobilization and other interventional steps are necessary to minimize further risk of infection. This facilitates union and further reduce chances of infection.
Aim: To review our challenges in the management of skin and soft tissue closure in Gustilo and Anderson type III fractures in Jos University Teaching Hospital, Jos.
Method: A retrospective study of consecutive patients treated for Gustilo and Anderson type III diaphyseal tibia and fibula fractures in our institution from June 2003 to May 2013. Type III fractures involving were recruited after clinical and radiographic review and bones stabilized with external fixators at presentation.
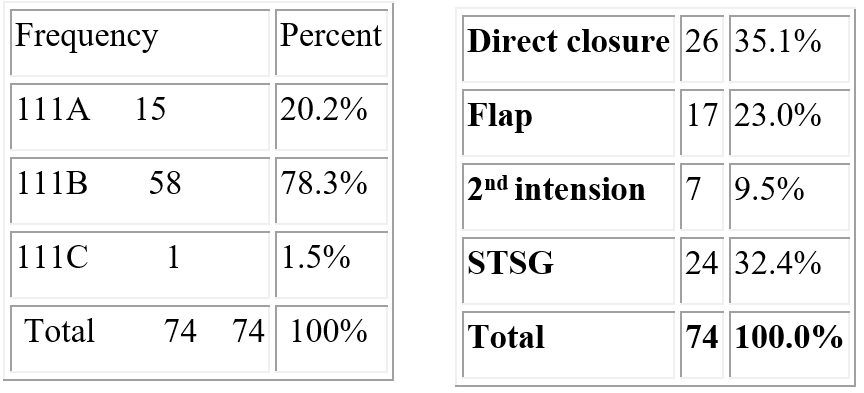
Results: There were 2040 fractures over this period 720 were tibia and fibula fractures and 480 were open. Most of which were type 1 and II. Seventy-four patients made our indications,63(85.1%) males and 11(14.9%) females with male: female ratio of 1.7:1 had type III tibia and fibula fracture between January 2004 to December 2013.There were 15(20.2%) type IIIA,58 (78.4%) type IIIB and 1(1.4%) type IIIC. The mean time interval before presentation was 13.4 days. Skin cover was achieved by direct closure (delayed primary closure) in 26 (35%),split thickness skin closure 24(32.4%) healing by secondary intention in 7(9.4%) and flap cover in 17(23%). Complications included wound infection in 12(22.2%), delayed union in 22(29.7%), wound dehiscence and loss of graft. The meantime taken to achieve wound cover was 15.7 days (Range of 3 days to 87 days). Other complications noted include wound infection, pin tract infection and chronic osteomyelitis.
Conclusion: Preponderance of late presentation of patients increases the rate of infection, multiple interventions that further worsened the wound size which could only be restored by secondary coverings.
Keywords: Type III; Open Tibia Fractures; Soft tissue cover
Introduction
Open fractures are common and challenging orthopedic emergencies [1,2]. Over 3.5 and 6 million individuals sustain open fractures yearly in the United States of America [2,3]. These open injuries range from a simple laceration to a mangled lower extremity. They could also be associated with major neurovascular complications, which may require amputation if not treated appropriately, and on time [2]. Septic complications arise in over half of severe open fractures despite modern antibiotic therapy and improvementin operating techniques [4,5]. Gustilo and Anderson Type III fractures may result from various forms of trauma including pedestrian, motor vehicle crash, motorcycle crash and missile injuries. They are associated with significant morbidity including prolonged hospital stay and high cost of care [6]. Severity of open fractures is dictated by the amount of external energy transmitted resulting in soft-tissue devitalization, microbial contamination, neurovascular compromised, and underlying patients’ co-morbid states. Access to care, that is often, delayed in our setting results in upgrade of injury at presentation and during the process of debridement [5]. Early intervention entails recruitment of surgical prophylaxis and therapeutic protocols.This implies that our intervention must rescue and restore the tissues from threats to live and limb [6].
Appropriate and optimal skin and soft tissue cover is an important component in management of open fractures. Success rate of closure of type IIIB is often as high as 50% [6]. This is enhanced by structured guideline with a management protocol that allows careful adherence to laid down surgical technique. This is of utmost importance since the amount of soft tissue damage, its management and sequelae are critical to the outcome of open fracture management. In extremely severe cases of open fractures, amputation could be an option in the evolution of care. However, with early and appropriate intervention this is avertable. Various recommendations in the care of open wounds revealed timing of closure adduced as an inexact science [6]. However, when closure is performed appropriately and in time, outcome improves.
This is our experience in the management of skin and soft tissue covering in patients with Gustilo and Anderson type III tibia and fibula fractures in our institution.We sought to verify the challenges associated with closure of type III wounds of varying etiology, presenting at different time intervals with different morbid states. The role of various mode of wound closure and their indications are also highlighted.
Patients and Method
This is a ten-year retrospective study of management of Gustilo and Anderson type III fractures of tibia and fibula between January 2004 and December 2013 at the Jos university teaching hospital (JUTH). There were 2040 fractures over this period 720 were tibia and fibula fractures and 480 were open. Seventy-four certified our criteria which were mainly type III diaphyseal fractures of the tibia and fibula. Patients with mangled extremities and injuries that were meant for amputation, multiply injured were excluded. Metaphyseal, intra articular fractures, type I and II fractures and any tibia and fibula fracture not treated with external device were also excluded. Patients with gangrene, those with severe co-morbid states warranting ICU care, those who left against medical advice were also excluded. There were 63(85.1%) males and 11(14.9%) females with male: female ratio of 1.7:1 and all had type III tibia and fibula fracture. Resuscitative interventionism forms of corrections of electrolyte derangements, correction of anemia, control of pain and bleeding and toileting with control of foul putrescent smells. Subsequent debridement and external fixation used as means of stabilization of the fractures. All the treatment were offered in the orthopedic department of the same hospital. Treatment involved debridement, daily wound care, inspection routine microbial prevention and surveillance, with the goal of achieving various forms of cover. Fractures were stabilized after resuscitation and debridement by external device. Interventions were in collaboration with the Plastic and Reconstructive surgeons of the surgery department of same hospital Data were extracted from patient files, theater records and operation register. We sought for bio-data, mode of admission, surgical interventions and the overall outcome. Ethical approval obtained from the committee on ethics of Jos University Teaching Hospital. Data was analyzed using epi info version 3.5.3.
Results
There were 2040 fractures over this period 720 were tibia and fibula fractures and 480 were open amounting to 66.7% prevalence over ten years. Among those that fulfilled our indications, sixty-three patients were male and eleven were female (M: F 5.7:1). The age of patients ranged from 15 to 70 years with a mean age of 37.97±13.57 years. Most injuries were within the age groups of 31 to 40 years and 21 to 30 years with 22(29.7%) and 20(27.0%) respectively. Table 1 shows the age groupings at which the accidents occur with age range of 11 to 70 years. Table 2 shows the mechanisms of injuries in which 25 (33%) were due to motorcycle crash, 20(27%) were due to gunshot wounds, 19(25.7) from motor vehicle crash, pedestrian injuries 9(21.2%) and falls 1(1.45). Table 3 shows the various sub-sets of grade III injuries were 15(20.2%) grade IIIA, 58(78.4%) with IIIB and one (1.4%) with grade IIIC Table 4 show the respective method of skin closure.
Mean duration of hospitalization was 76 days. Forty-one injuries (55.4 %) were on the right leg while 33(44.6%) on the left leg. On the day of injury, twenty-five patients (33.8%) presented, 34(45.9%) presented between the second and seventh day of injury, 7(9.4%) presented within the eight to fourteenth day while 8 (10.8%) presented after two weeks of injury. Those with frank soft tissue and bone infection were 40(54.1%) most of which were those that presented late and had sought treatment in peripheral hospitals and traditional bone setters. Those without evidence of infection were 22(29.8%) while12(22.2%) that developed infection on the ward were type IIIB. Directly closed wounds were 26(35%) with dehiscence in 5(6.7%), 24(32.5%) had split thickness skin grafting with 3(4%) having over 50% lyses while in 17(23%) flap that were raised 2(2.7%) were loss to infection, 7(9.5%) were allowed to heal by secondary intention. Patients with delayed presentation had prolonged hospitalization and type IIIB had more infection rate.
Table 1: Age range of patients.
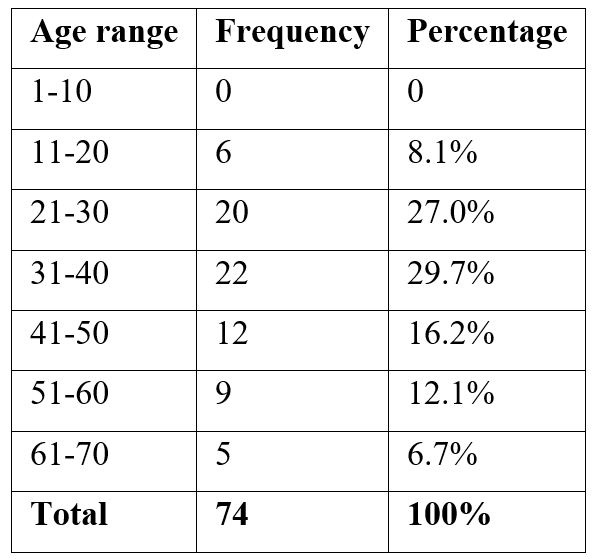
Table 2: Mechanisms of injury.
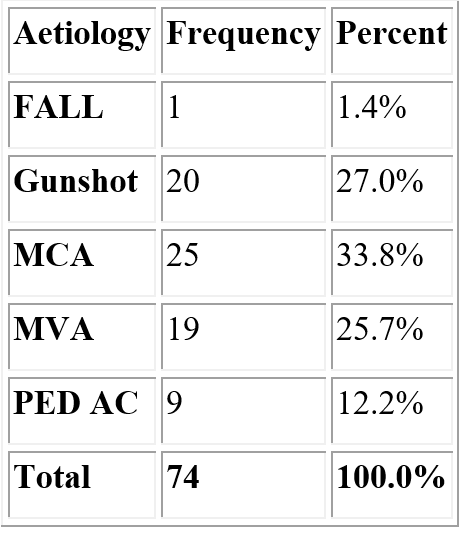
Abbreviations: MCA- Motorcycle Accident; MVA- Motor vehicle Accident; PED AC- Pedestrian Accident
Table 3: Grades of Gustillo and Andersson Type III.
Discussion
The predominance of tibia fractures over other fractures in term of occurrence have been highlighted.7Out of 720 tibia and fibula fractures that presented during the ten-year period 480 were open. There is a gross preponderance of young adults sustaining open fractures; this is similar to findings within the region and worldwide where it is found in significant number of victims of high energy trauma [7]. Indeed, trauma is a disease of the young (Table 1) [7,8]. Various traumatic conditions can be responsible for type III fractures among these were gunshots, falls, motorcycle injuries, motor vehicle crash, pedestrians and direct assaults (Table 2). The high number of motorcycle accidents constituting the highest 25(33.8%) and gunshot injuries 19(25.7%) reveal increasing civilian cosmopolitan high-energy injuries with attacks occurring at the fringes of the city by unknown assailants. Others were motor vehicles accidents and pedestrian injuries. The common denominator among these injuries is their similarity to injuries with high velocity missiles presenting with bone comminution and large soft tissue defect which make their healing process prolonged and prone to numerous complications [9].
Treatment of Gustilo and Anderson type III fractures of tibia requires aggressive debridement, adequate fixation and early flap coverage of soft tissue defect [6,10]. This therefore requires a multidisciplinary approach in order to achieve a favorable outcome.
Restoration of both structure and function require varying interventional treaties [10]. But our patients presented on two different timelines. The early presenters were rescued from immediate life and limb threats while the late presenters were rescued from potential limb threatening conditions. In spite of these, all had to be resuscitated as they presented with varying degree of constitutional derangement such as anemia, sepsis, dehydration, severe pain, electrolyte imbalance and poor glycemic control. Only 25(33.7%) patients presented within the first day of injury. Therefore, intervention and demand of this category of patients must involve commence with ATLS protocol.10 In this setting, life threatening conditions included acute blood loss, derange electrolytes, malnutrition and co-morbid conditions emanating from other ailing diseases like diabetic mellitus, retroviral diseases and sickle cell disease. Early review of the wound with the plastic surgeons and involvement of the vascular surgeon at the slightest suspicion of major vascular compromise to the extremity is of import. Clinical photography allows for easy review of the wound without causing further distress to the patient with repeated change of dressings [8,10]. It also allows for comparison of real time status of the wound with the initial appearance. Control of pain and the administration of anti-tetanus prophylaxis and antibiotics were of utmost importance at this stage too.
Initial provisional stabilization devoid of pain is necessary to prepare for imaging and other investigations that may involve movement of patient or the body parts. However, most of them present wounds at various stages of healing and deterioration. Deodorization and toileting was of necessity among the late presenters who often had foul smelling and discharging necrotic wounds. At this stage initial use of agents such as hydrogen peroxide or metronidazole with copious irrigation have been of immense usefulness. However, the fear of infection and further breakdown usually makes the timing of wound closure in open fractures very controversial [11-13]. In most of these wounds, infection was already established 40(54.1%). This was a consequence of delay in presentation that further led to more devitalization of tissues of skin, fascia and the bone, requiring further excision. Additional larger soft tissue and bone defects are created in the process. This situation, in which 40(54.1%) presented with established infection, the need for thorough and radical excision of necrotic, non-viable and devitalized tissues is mandatory. However, this may not be achieved in single session. Therefore, serial intervention to render the wound bed clean and healthy is required. It is in view of this that open fractures of the extremity are regarded not only orthopedic emergencies but leading cause of devastating complications and prolonged rehabilitation [13].
However, no clinical guidelines or protocols are available to determine which wounds are amenable to immediate closure [15]. In order to ameliorate this, adequate knowledge of various methods of wound covering suffices. The wound is relieved of sequestrum, foreign bodies, undermined dead space and pockets of purulent fluid that are toxic to healing and callus formation. Consequence of delayed presentation and the attendant established infection is the infliction of extensive tissue loss in this group of traumatic wounds. Apart from tissue necrosis cause by infection, wound excision further creates extensive soft tissue and bony defect that must be filled.
Delayed definitive wound closure is the worldwide acceptable standard while immediate wound closure may be inappropriate in this scenario because of the questionable status of the underlying tissue beds [12]. Since no ideal timing of wound closure is defined there is need to prioritize protocols with use of wound cultures obtained before and after debridement and irrigation [14]. A scientifically based knowledge of reconstructive ladder is therefore noteworthy and provides alternatives to successful management of these wounds after infection is controlled. This will aim at restoring contaminated, traumatic or infected wounds to a near physiologically clean surgical wound. The traditional delay in closure of open fractures after initial debridement was meant to minimize the risk of complication especially deep-seated organ site infection [5,15].
Advancement in debridement protocol and antibiotic usage now puts the six-hour golden rule into question [9,16]. But it is known that inflammatory phase begins at approximately 6 hours; cytokines and other chemical mediators are released, which attract lymphocytes, granulocytes, and other inflammatory cells to the area and the numbers of these cells peak at about 24 hours [16]. Nevertheless, it still suffices to embark on this in order to obtain favorable outcome.
Moreover, the preponderance of farmyard and gunshot injuries with unlimited contaminants and the high tendency to further deteriorate entails that all protocols available in surgical prophylaxis must be applied in open fractured wounds. Other useful measures of reducing bacterial load such as jet and pulse lavage, suction dressings, use of antibiotic beads and pouches in the wounds were useful in reducing duration of preparing the tissue bed for secondary procedure [17]. Antibiotics were administered based on sensitivity pattern after the empirical usage at peri-operative period. It was stopped five days after wound cover was achieved against the 3 days recommended [4.10,18].
Although all the wounds were from traumatic injuries and presented at different morbid states none of the patients resulted in amputation. All the wounds however, required similar intervention protocol but to a varying extent of aggression. This is in line with the suggestion that open fractures of tibia that requires closure should be treated with high priority of early debridement, rigid fixationnd early flap coverage [11,18]. To a large extent these wounds required multiple interventions at the slightest suspicion of structural deterioration and microbial invasion. These interventions created further extensive wound excision hence larger wounds were created. These large defects of varying sizes present with management challenges that required both scientific and contextual experience and early corroboration with plastic surgeons. This, not withstanding, requires basic knowledge of local vascular anatomy that assists in flap design of appropriate local and regional flap that enables the management of vast majority of open fractures such as in the tibia.11Favorable outcome was achieved in all cases except in one free flap that failed.
A low-pressure delivery of normal saline was of great importance as it does not reduce its diluting ability in reduction of bacterial load in the wound. Its role by virtue of its accessibility, availability tissue compatibility has been alluded to [11]. However, more irrigation fluid had to be used for patients that presented late in addition to dilute disinfectant to further reduce the burden of microbial load. Although high pressure irrigation is said to have greater prowess of dilution ability its accessibility and cost does not encourage its frequent use in our setting. Besides its comparative efficacy is not superior to the low-pressure method [11]. The use of tap water had been reported and is equally effective but the chance of growing pseudomonas species can be high [10,20].
Most of those presenting on the first day were gunshots which precluded immediate wound closure. Where bones were exposed and desiccated with impending sequestrum treatment was dictated by evolving status of the wound. Among treatment offered were initial toileting, trephining to permit granulation tissue sprouts and neurectomy in order to rid the wound of extensive microbial load. With these, revascularization is enhanced; healthy granulation tissue bed established for split thickness skin grafting and free flap and for fracture union to establish
Several methods of wound covering procedures undertaken range from simple direct skin cover, split thickness skin cover, local flap, healing by secondary intention. Despite a better early outcome of closure in type IIIA wounds, 5(6.7%) had wound dehiscence but were salvaged subsequently. In split thickness skin cover, 3(4%) had over 50% lyses while 2(2.7%) free flaps lost to infection. In all these pseudomonas spp were involved. The type of skin closure offered to each grade depends on several factors such as the sub type of the injury as determined by the degree of soft tissue loss, site of skin loss, the duration between injury and presentation, extent of skin and facial necrosis, muscle loss and the extent to which bone is exposed. It is a known fact that early closure of open fractures prevents infection and encourages revascularization of the underlying periosteum. It also decreases the requirement for subsequent debridement and soft tissue procedures with shortened hospital stay and minimal morbidity [13,14]. Unfortunately, we do not have the chance of having early patient presentation in our setting. Only 25(33.7%) of our patients presented on the day of injury while the rest presented between the second and thirteen weeks.
Although most of the wounds were successfully covered using the known methods, a category of open fractures exist that require methods that are more sophisticated. These were distal third tibia defects and pose formidable challenge to the orthopedic and plastic and reconstructive surgeons [10]. Distally based pedicle flaps had to be employed to yield satisfactory results. This is evident by the flap take and incorporation using the short-term outcome measures. The large sizes of the wound potent the use of cross leg flaps as an option especially where size of the wounds is greater than 1.5 zones or 1.5 compartments especially where microvascular flaps are not readily available [10]. Microvascular flaps have broadened the latitude of treatment offered to grade IIIB fractures. Free vascularized osteoseptocutaneous flap has been described as effective alternative in the management of type IIIB tibia fracture using one stage procedure [14,19].
The role of stabilization of the fracture with external fixators cannot be underestimated in managing these fractures. This need arises because most grade III open tibia fractures were managed by some degree of delayed soft tissue cover [2] and the need for regular unobstructed access to the wound is required. Delay was in order to ensure a healthy tissue bed so that a simpler split thickness graft can be unhindered. It has been alluded that immediate primary closure of open fracture wounds after thorough debridement appear to cause no increase in infection [13] especially in selected few that presented early and devoid of gross contamination. Primary closure could not be embarked in a third of the patients because they had gunshot injuries. The need for delay was predicated on the background status of the wound which were grossly contaminated, presence of devitalized tissues and established infection. In our study 40(54.1%) presented with established infection and the need for thorough debridement involving neurectomy and radical wound excision and copious irrigation was mandatory. Thereafter, there was the need to accompany such with serial unrelenting debridement in order to create a healthy tissue bed.
Considering the extensive open injuries that were at different stages of contamination and infection, various methods were devised to achieve favorable outcome. Although bone union and the limbs were salvaged in all cases, some developed chronic discharging sinus, ugly scars and hyperpigmentation.
Wound covering of type III fractures is major challenge and requires early multidisciplinary approach [10,19]. In order to achieve proper fracture union in contaminated and infected wounds, early intervention in form of debridement, copious irrigation and stabilization and adequate skin cover is required to forestall morbidity associated with open wounds. Proper attention and meticulous painstaking strict aseptic protocol must be undertaken early since this provides an index of outcome of care. Recent advances in stabilization depicted by external fixation provides main support and allows room for easy access for routine inspection, cleaning and decision making and reconstructive procedures have improve the outcome of management [19,21].
Most importantly, these injuries require dedicated team approach with a team leader that has vast knowledge not only in functional anatomy22 but also biomechanics of the lower extremity.
In conclusion, open wound resulting from fractures of the extremities result from various causes may be a source of threat to limbs and life. Early and aggressive intervention in form of serial debridement and copious irrigation, stabilization with external device can ameliorates these. Knowledge of soft tissue care required to achieve acceptable wound coverage. Prompt evaluation and collaborative intervention with plastic and reconstructive surgeons in achieving wound coverage is of immense importance. Interestingly, more complex injuries require more aggressive and early intervention. This was cardinal in the successful rescue of the only major (type IIIC) vascular injury treated.
The limitation of the study is that it is hospital based retrospective study. Statistics are limited to the available records. Equally important was the great variation in time of presentation to the hospital among the patients. A prospective will be more succinct, sorting out of patients in different injury – presenting time and monitor their challenges with respect to healing and complications.
References
- Praemer A, Furner S, Rice D, editors. Musculoskeletal conditions in the United States Park Ridge. American Academy of Orthopedic Surgeons, 1992.
- Cross III WW, Swiontkowski MF. Treatment principles in the management of open fractures. Indian journal of orthopaedics, 2008; 42(4): 377.
- Giannoudis P, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. The Journal of bone and joint surgery British volume, 2006; 88(3): 281-289.
- Lenarz CJ, Watson JT, Moed BR, Israel H, Mullen JD, MacDonald JB. Timing of wound closure in open fractures based on cultures obtained after debridement. JBJS, 2010; 92(10): 1921.
- Giannoudis PV, Papakostidis. Surgical Debridement of Open Fractures. Mark S Granick, MD, FACS, 2007: 57.
- Philipa U, Mobashb M, Osemogie W. Early Management of Open Tibial Fractures in Benin-City-Result of a Structured Treatment Protocol, 2006.
- Babalola O, Salawu ON, Ahmed B, Ibraheem G, Olawepo A, Agaja S. Epidemiology of traumatic fractures in a tertiary health center in Nigeria. Journal of Orthopedics, Traumatology and Rehabilitation, 2018; 10(2): 87.
- Freedy JR, Magruder KM, Mainous AG, Frueh BC, Geesey ME, Carnemolla M. Gender differences in traumatic event exposure and mental health among veteran primary care patients. Military Medicine, 2010; 175(10): 750-758.
- Elniel AR, Giannoudis PV. Open fractures of the lower extremity: current management and clinical outcomes. EFORT open reviews, 2018; 3(5): 316-325.
- Jordan DJ, Malahias M, Khan W, Hindocha S. Suppl 2: M2: The Ortho-Plastic Approach to Soft Tissue Management in Trauma. The open orthopaedics journal, 2014; 8: 399.
- Crowley D, Kanakaris N, Giannoudis P. Irrigation of the wounds in open fractures. The Journal of bone and joint surgery British volume, 2007; 89(5): 580-585.
- Singh J, Rambani R, Hashim Z, Raman R, Sharma HK. The relationship between time to surgical debridement and incidence of infection in grade III open fractures. Strategies in trauma and limb reconstruction, 2012; 7(1): 33-37.
- Pollak AN, Jones AL, Castillo RC, Bosse MJ, MacKenzie EJ, Group LS. The relationship between time to surgical debridement and incidence of infection after open high-energy lower extremity trauma. The Journal of Bone and Joint Surgery American, 2010; 92(1): 7.
- Lenarz C, WatsonJT, Moed BR. Timing of wound closure in open fractures based on cultures obtained after debridement, J Bone &J surg, 2010; 92(10): 1921-1926.
- Naique SB, Pearse M, Nanchahal J. Management of severe open tibia fractures: the need for combined orthopedic and plastic surgical treatment in specialist centers. J Bone surg. Br, 2006; 88(3): 351-357.
- Gonzalez AO. Costa TF, Andrade ZA Medrado ARAP. Wound healing- a literature review. A Bras. Dermatol, 2016; 91(5): 614-620.
- Shetty R, Barreto E, Paul KM. Suction assisted pulse lavage:Randomized control studies comparing its efficacy in healing of chronic wounds.Int. Wound J, 2014; 11(1): 55-62.
- Ikem IC, Oginni LM, Ogunlusi JD. Determinants of management outcome in open tibia fractures in Ile-Ife.Nig.J.Surg.Res, 2006; 1-2: 81-83.
- Luo Z, Luo I, Jiang H, Song C, Gong M, Wang Y. Pedicle flap transfer combine with external fixator to treat open fracture with soft tissue defect.
- Bresler D, Balzer M, Dannehl A, Fleming HC. WingenderJ.Persistence of pseudomonas aeriginosa in water biofilmson elatrometricmaterial.Water supply, 2009: 9(1).
- Howard M, Court-Browm CM. Epidemiology and management of open fractures of the lower limb. Br. J Hosp Med,1997; 57(11): 582-587.
- Burg A, Nachum G, Salai M, Haviv B, Holar S, Volkas S, et al. Treating civilian gunshot wounds to the extremities in a level I trauma center: Our experience and recommendations. Isr Med. Assoc. J, 2009; 11(9): 546-551.

