A Decompression Illness Induced Spine Atrophy With 12 Years Follow-Up and Literature Review
Yangliang Huang1,*, Yi Zhong2
1Department of Spine Surgery, the First Affiliated Hospital, Sun Yat-Sen University, China
2Key Laboratory of Neuroscience, School of Basic Medical Science, Guangzhou Medical University, China
Received Date: 22/08/2021; Published Date: 15/09/2021
*Corresponding author: Yangliang Huang, Department of Spine Surgery, the First Affiliated Hospital, Sun Yat-Sen University, Guangzhou, 510700, China
Abstract
Decompression Illness (DCI) has been deemed a rare clinical entity in different diver populations. The incidence of DCI varies from 0.010% to 0.095% per dive. The DCI is a collective term including two disorders. The first one is caused by evolution of bubbles from dissolved inert gas; the second one is caused by introduction of air to the systemic circulation by pulmonary barotrauma. The gold standard treatment for DCI is recompression in a hyperbaric chamber with administration of hyperbaric oxygen during the treatment. We report a case of a 46-year-old technical diver complained decrease motor and sensory function of lower limbs 50 minutes after diving mission had been completed. He had received first aid 100% oxygen and sought medical attention right after the accident. After hyperbaric chamber treatment, the lower limb muscle power recovered from 2/5 to 3/5. He was discharged from hospital after rehabilitation for 3 months when he could walk by himself. After follow up for 12 years, his lower limb muscle power had no improvement while he complained increase of walking instability. The MRI scan discover thoracic spinal cord atrophy. The side effect of spinal cord atrophy induced by DCI has not been reported before.
Keywords: Decompression illness; hyperbaric chamber; spinal cord atrophy
Introduction
Diving is a popular recreational pastime, as well as an activity with numerous applications in the scientific, commercial, military, and exploration realms. Although diving can be done safely, the underwater environment is unforgiving. Problems may arise during a dive due to insufficient medical or physical fitness, improper use of equipment, or inadequate management of the high-pressure environment.
Decompression Illness (DCI) is a term used to encompass injuries due to Arterial Gas Embolism (AGE) and decompression sickness (DCS) [1]. AGE typically results from pulmonary barotrauma-induced damage to the alveolar wall and introduction of gas into the systemic arterial circulation. DCS, colloquially known as the bends, results from the uncontrolled release of gas from tissues during or after surfacing with inadequate time for decompression [2,3].
We report a 46-year-old technical diver complained lower limb muscle weakness after repeat diving. He receives routine treatment of DCI. After rehabilitation, he could walk without aid. After 12 years, he complained walking instability, MRI exam revealed thoracic spinal cord atrophy. To our knowledge, DCI induced spinal atrophy has not been reported before.
Case Report
History
A 58-year-old man with history of 12 years of lower limb muscle weakness presented to our department. He complained progressive gait disturbance for half a year. The discomfort cannot be relieved by any spinal movement or posture. Bed rest could not improve the symptom. 12 years ago, he had experience a decompress illness when he was a technical diver. Before the accident, he had been diving for 2 times. After the third diving mission had been complete for 50 minutes, he complained decrease motor and sensation function of lower limbs. He had received first aid 100% oxygen right after the accident by his teammates and consulted medical attention at local hospital, then transfer to regional hospital 8 hours later for hyperbaric chamber treatment. After hyperbaric chamber treatment, the lower limb muscle power recovered from 2/5 to 3/5. He was discharged from hospital after rehabilitation and repeat hyperbaric oxygen therapy for 3 months when he could walk by himself. After follow up for 12 years, his lower limb muscle power had no improvement while he complained increase of walking instability. The MRI scan discover thoracic spinal cord atrophy. He denied any other systemic diseases, there was no thoracic trauma during this time.
Examinations
Physical examination did not reveal any deformity of the thoracic spine. The manual muscle strengthtest demonstrated 4/5 strength on the left and 4/5 on the right. No complain about bowel movement or dysuria function was recorded. Increase of deep tendon reflex was significantly noted. Babinski sign was positive bilaterally. Muscle tonus of lower extremities was increased. Sensory function was decreased below abdominal.
X-ray images showed no pathological destruction and loss of spinal column support. MRI scans revealed no hyper-intense changes on T2-weighted images. No spondylodiscitis signs could be discovered by MRI scans. However, obvious spinal atrophy could be observed at T5 and 6 levels. The Laboratory examinations consisted of complete blood count, electrolytes, liver, renal function tests, urinalysis. Except increased ESR, CRP, blood sugar, and white blood cells, they were all normal (Figure 1).
After consultation of neurology department, the patient discharged with per oral neurotrophic drugs.
The design and performance of this study conformed to ethical standards of Helsinki Declaration and our national legislation. It was approved by Medical Ethical Committee of our institution. The patient was enquired whether or not willing to take part in a scientific report and informed consent forms were signed by himself.
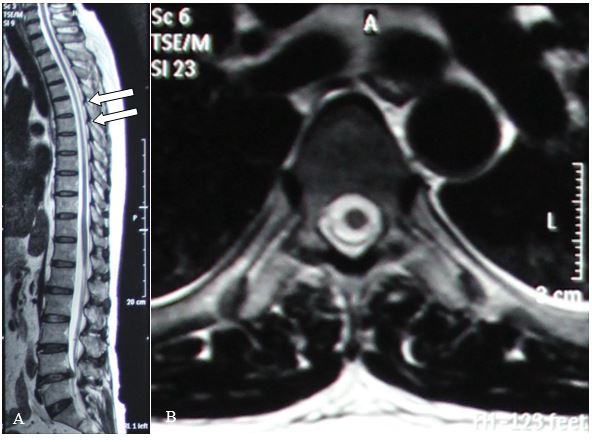
Figure 1: Atrophy changes on T2-weighted images at the T5 and 6 level, there is a herniated disc at L4/5 level without symptom. An axial cut (white arrow); B transverse cut.
Discussion
The incident of DCI is low, 0.324 per 10,000 person-dives was reported by scientific diving community, while commercial decompression diving has been reported to be higher, as high as 35.3 per 10,000 person-dive [4]. The incident depends highly on the dept of dive operations. Decompression illness (DCI) is a term used to described injuries due to Arterial Gas Embolism (AGE) and Decompression Sickness (DCS). AGE typically results from pulmonary barotrauma-induced damage to the alveolar wall and introduction of gas into the systemic arterial circulation. DCS results from the uncontrolled release of gas from tissues during or after surfacing with inadequate time for equilibration (decompression) [5,6]. One common classification system of DCS was described as type 1 or type 2. Type 1 DCS is usually characterized by musculoskeletal pain and mild cutaneous symptoms. Skin manifestations include itching and mild rashes, Musculoskeletal manifestations of type 1 DCS are articular or periarticular pain. Common locations include shoulders, elbows, wrists, hips, knees, and ankles. Type 2 symptoms are more serious. They typically fall into 3 categories: neurologic, inner ear, and cardiopulmonary. Neurologic symptoms include numbness; paresthesia or tingling; muscle weakness; impaired gait, physical coordination or bladder control; paralysis; or change in mental status. Inner ear symptoms include tinnitus, hearing loss, vertigo or dizziness, nausea, vomiting, and impaired balance. Cardiopulmonary symptoms, known as the chokes, include a dry cough, retrosternal pain, dyspnea, and sometimes pink-stained, frothy sputum. Severe neurologic DCS symptoms usually appear within 10 minutes of surfacing and in 90% of cases symptoms will be present within the first 3 hours. In some cases, it can take up to 24 hours for symptoms to be noticed by the diver [7-9]. The reporting case should be classified as neurologic Type2.
The clinical assessment is important for diagnosis of DCI. Onset of symptoms less than 10 minutes after surfacing could indicate AGE. Onset of symptoms more than 10 minutes after surfacing are more likely associated with DCS [10]. Depth-time exposure, ascent rate, ascent stops and patterns of repetitive dives are also important factors affecting DCI [11]. Being warm during the descent and/or bottom phase of a dive will increase inert gas uptake, increasing the subsequent decompression stress. Being cold during the ascent and/or stop phase inhibits inert gas elimination, increasing the decompression stress. Exercise during the descent and/or bottom phase of a dive will increase inert gas uptake, increasing the subsequent decompression stress. Light exercise during the ascent and/or stop phase promotes inert gas elimination, reducing the decompression stress. Health history and medical usage are contributing factors [12]. However, there are no specific diagnostic investigations that can establish the diagnosis of DCS. Chest radiographs are utilized to exclude pneumothorax and pneumomediastinum in cases in which pulmonary barotrauma is suspected. An untreated pneumothorax is a contraindication for recompression in a hyperbaric chamber. It may also be crucial to recognize and treat a pneumothorax before any medical evacuation to the hyperbaric center [13].
High partial pressure oxygen is the primary first aid measure for DCI. High oxygen concentration in the lungs will accelerate inert gas elimination. High oxygen partial pressure in the bloodstream can also alleviate ischemic insults produced by bubble blockages. Sustained oxygen delivery can reduce or even eliminate symptoms [14]. The definitive treatment of DCI is Hyperbaric Oxygen Therapy (HBOT), the delivery of oxygen at a partial pressure substantially higher than that achievable at normal atmospheric pressure. The course of HBOT will vary according to the particulars of each case. Full resolution of DCS symptoms can often be achieved with 1 or sometimes multiple HBOT treatments. In some cases, resolution will be incomplete, even after many treatments. The normal clinical approach is to continue treatments until no further improvement is seen in the patient’s symptoms. Modest residual symptoms will then often resolve slowly, after the treatment series is ended. Full resolution of symptoms can sometimes take months to achieve and in some instances may never be realized [15].
Spinal atrophy could be commonly seen in demyelinating spinal diseases, such as Multiple Sclerosis (MS) and Neuromyelitis Optica Spectrum Disorder (NMOSD). The atrophy pattern of these diseases is not the same. Computer-aided artificial intelligent using the pipeline efficiently quantifies the SC volume of MRI images and can be utilized as an affordable tool for diagnostic purposes [16]. However, the side effect of spinal atrophy induced by DCI has not been reported before. It has not been confirmed that DCI will develop spinal atrophy or not, this case report is considered to be one of the evident that hypoxia induced spinal atrophy is possible. However, larger case collection is demanded.
Conclusion
Diving is becoming popular as a recreation event. However, the side effect of DCI should not be ignored. hyperbaric oxygen therapy and first aid pure oxygen are effective treatments for DCI. Our case suggests that when neurological defect is sustained for a long time without improvement, spinal cord atrophy should be considered.
References
- Pollock NW, Dunford RG, Denoble PJ, et al. Annual diving report - 2008 edition. Durham (NC): Divers Alert Network; 2008; 139.
- Imbert JP, Fructus X, Montbarbon S. Short and repetitive decompressions in air diving procedure: the commercial diving experience. In: Lang MA, Vann RD, editors. Proceedings of repetitive diving workshop. Costa Mesa (CA): American Academy of Underwater Sciences; 1992; 63-
- Luby J. A study of decompression sickness after commercial air diving in the Northern Arabian Gulf: 1993-95. Occup Med (Lond) 1999; 49: 279-2
- Vann RD, Butler FK, Mitchell SJ, et al. Decompression illness. Lancet 2011; 377: 153-1
- Koch GH, Weisbrod GL, Lepawsky M, et al. Chest radiographs can assist in the diagnosis of pulmonary barotrauma. Undersea Biomed Res, 1991; 18(Suppl): 100.
- Warren LP, Djang WT, Moon RE, et al. Neuroimaging of scuba diving injuries to the CNS. Am J Roentgenol 1988; 151: 1003-100
- Levin HS, Goldstein FC, Norcross K, et al. Neurobehavioral and magnetic resonance findings in in two cases of decompression sickness. Aviat Space Environ Med 1989; 60: 1204-12
- Moon RE, Massey EW, Debatin JF, et al. Radiographic imaging in neurological decompression illness. Undersea Biomed Res 1992; 19(Suppl): 42.
- Gempp E, Blatteau JE, Stephant E, et al. MRI findings and clinical outcome in 45 divers with spinal cord decompression sickness. Aviat Space Environ Med, 2008; 79: 1112-1116.
- Gempp E, Morin J, Louge P, et al. Reliability of plasma D-dimers for predicting severe neurological decompression sickness in scuba divers. Aviat Space Environ Med 2012; 83: 771-775.
- Thom SR, Milovanova TN, Bogush M, et al. Microparticle production, neutrophil activation and intravascular bubbles following open-water scuba diving. J Appl Physiol, 2012; 112: 1268-1278.
- Longphre JM, Denoble PJ, Moon RE, et al. First aid normobaric oxygen for the treatment of recreational diving injuries. Undersea Hyperb Med, 2007; 34: 43-49.
- Loveman GAM, Seddon FM, Jurd KM, et al. First aid oxygen treatment for decompression illness in the goat after simulated submarine escape. Aerosp Med Hum Perform 2015; 86: 1020-102
- Pollock NW, Natoli MJ. Performance characteristics of the second-generation remote emergency medical oxygen closed-circuit rebreather. Wilderness Environ Med 2007; 18: 86-
- Pollock NW, Natoli MJ. Chemical oxygen generation: evaluation of the Green Dot Systems, Inc. portable non-pressurized emOx device. Wilderness Environ Med 2010; 21: 244-24
- Ciccarelli O, Cohen JA, Reingold SC, et al. Spinal cord involvement in multiple sclerosis and neuromyelitis optica spectrum disorders. Lancet Neurol, 2019; 18: 185-197.

