Establishing Posterior Occlusal Support: A Case Report
Evangelos Ximinis, Maria Tsiafitsa, Dimitrios Dionysopoulos, Olga Naka*
School of Dentistry, Faculty of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
Received Date: 02/07/2021; Published Date: 21/07/2021
*Corresponding author: Olga Naka, DDS, MClinDent, PhD, School of Dentistry, Faculty of Health Sciences, Aristotle University of Thessaloniki, 176 Karamanli Avenue, Thessaloniki, 54248, Greece. E-mail: naka@dent.auth.gr, Tel: +30-2310-307.444, ORCID: https://orcid.org/0000-0003-2234-4229
Abstract
Loss of posterior teeth impacts a patient’s function as well as their facial esthetics. Changes in the Occlusal Vertical Dimension (OVD) may result in anterior crossbite or Pseudo-Class III malocclusion. This clinical report describes the prosthodontic management and stabilization of a patient with reverse anterior articulation due to loss of posterior occlusal support. The comprehensive diagnostic approach, the information gathered from the provisional phase and the consistent sequence of clinical and laboratory stages led to a definitive treatment outcome that guaranteed the success of the prostheses and the patient’s comfort and satisfaction.
Keywords: Malocclusion; Crossbite; Partial denture; Fixed partial denture; Occlusal guidance
Introduction
Loss of posterior teeth impacts not only a patient’s function, but their facial esthetics, as well. Indeed, changes in the occlusal vertical dimension (OVD) did occur, making the management of its consequences remarkably challenging [1,2]. Early loss of posterior teeth could result in anterior crossbite or Pseudo-Class III malocclusion, i.e., a positional relationship related to an acquired neuromuscular reflex necessary for occlusion to be achieved in the posterior area [3-5]. While Class III malocclusion is described as a condition of abnormal maxillo-mandibular relationship, usually of skeletal etiology, Pseudo-Class III malocclusion is associated with dental factors [5-7]. It has been argued that when posterior occlusal support is lost bilaterally, mastication is performed only by the anterior teeth and the temporomandibular joints are displaced into a superior-anterior position [8].
A diagnosis of anterior reverse articulation requires a thorough clinical and radiographic examination to differentiate between dental and skeletal malocclusion [9]. Once patients presenting a Class I skeletal pattern with a forward shift of their mandible on closure, due to loss of posterior occlusal support, are guided to a centric relation (CR) position, they will most likely present an edge-to-edge incisal relationship [4,10,11].
The therapeutic approach of such collapsed occlusion cases and the management of the subsequent OVD increase are challenging and require a detailed rehabilitation protocol. This clinical report describes the therapeutic approach for establishing posterior occlusal support in a patient with anterior reverse articulation.
Methods
A 52-year-old man sought treatment complaining of chewing difficulty and poor esthetics. The patient’s medical history included Hypertension, Hyperlipidemia and Obesity. Extraoral, intraoral and radiographical examinations revealed loss of all but one posterior teeth, a maxillary 10-unit Fixed Partial Denture (FPD) with metal acrylic design, a mandibular 4-unit FDP and severely damaged lower teeth (Figure 1). The patient’s oral hygiene was deemed poor. Anterior reverse articulation, corresponding wear of maxillary FPD and reduced OVD were also noted (Figure 2). However, it was observed that when the patient was guided to the CR position, an incisal edge relationship was achieved, while the OVD increased proportionately.
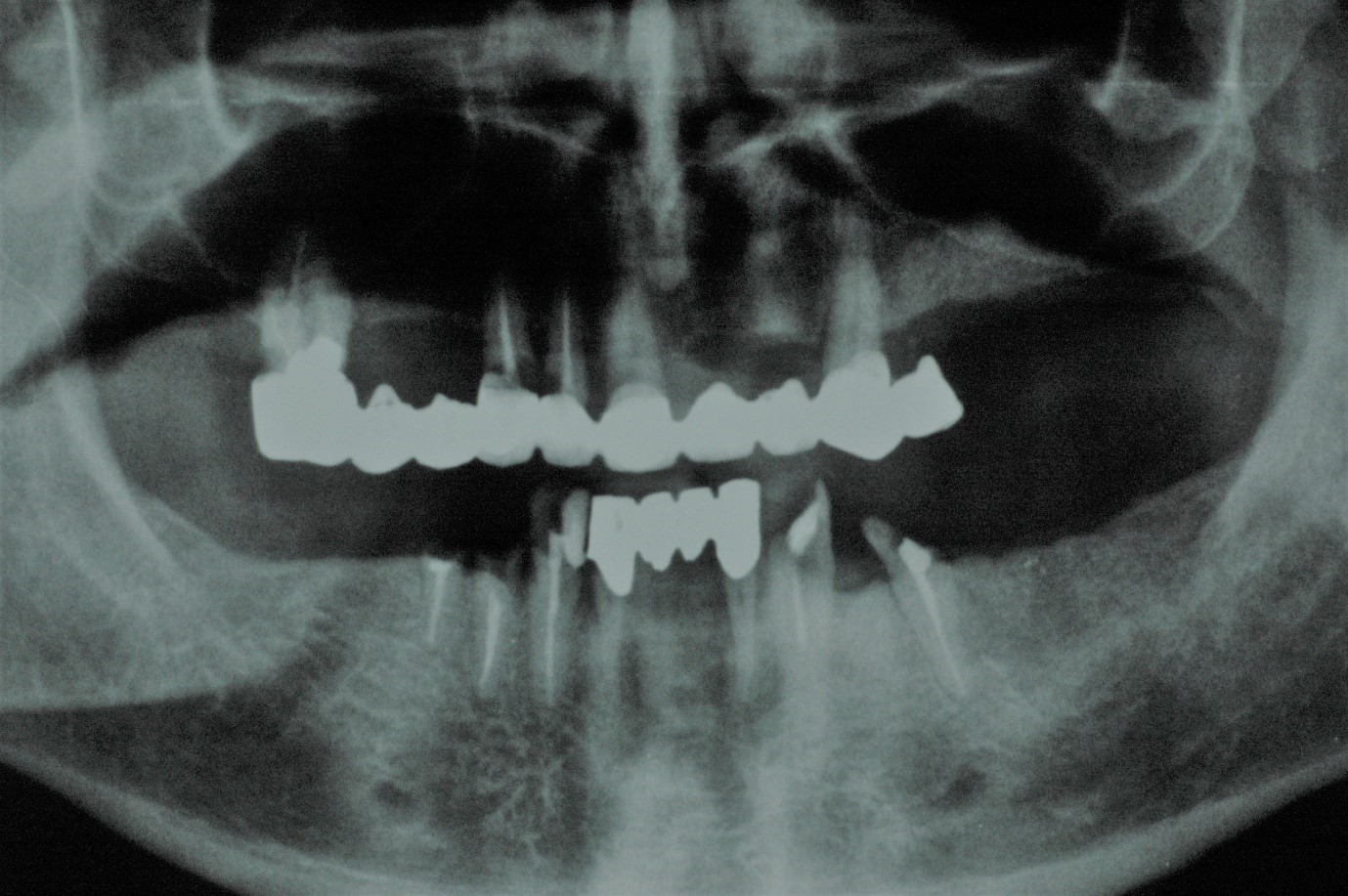
Figure 1. Radiographic image of the patient’s pre-treatment status.

Figure 2. Loss of VDO with anterior reverse articulation.
Diagnostic data were collected to develop an individualized treatment plan for the patient. Preoperative extra- and intraoral photographs, as well as primary upper and lower impressions were taken. The mandible was related to the maxilla using a Lucia jig deprogrammer (Figure 3), in conjunction with bimanual manipulation, and the CR position was recorded [12]. Casts mounted on the semi-adjustable articulator were analyzed. A diagnostic wax-up was fabricated to design the anterior guidance necessary for the increased OVD and to calculate the prosthetic space (Figure 4) [13]. Possible treatment options were discussed. Implant placement had been rejected by the patient from the outset of treatment. Thus, the treatment plan suggested included porcelain fused to metal FPDs combined with Removable Partial Dentures (RPDs) and extra coronal precision attachments.

Figure 3. Using the Lucia jig to take an accurate centric relation registration.

Figure 4. Diagnostic wax up;re-establishment of anterior guidance with increased OVD.
An informed consent form was signed by the patient. Mouth preparation, including oral hygiene measures, periodontal treatment and extractions of ‘hopeless’ teeth (#32, #42) and the root of the right mandibular second premolar (#45), was performed. Subsequently, the upper and lower prostheses were removed, and the remaining teeth were assessed. The maxillary right molar underwent endodontic treatment and root resection therapy, while the palatal root was preserved. Endodontic retreatment was performed on #12, #13, and mandibular canines and premolars (#33, #35, #43, #44) were treated with cast post and cores (Figure 5). The teeth were prepared, impressions were taken and record bases with wax rims were used to orient the occlusal plane, to define the appropriate OVD and to record the postural position of the mandible in relation to the maxilla.
Provisional acrylic resin prostheses reinforced with metal casting and interim RPDs with metal clasps were placed until complete soft tissue healing took place (Figure 6). Anterior guidance, phonetics and esthetics were carefully checked at this stage to ensure the patient had adapted to the new situation.

Figure 5. Teeth preparations and cast post and cores.

Figure 6. Provisional restorations.
After 12 weeks, the experience of the provisional treatment was reviewed and, once stability had been achieved and the patient was satisfied with the esthetics, the final prosthetic phase could be initiated. Tooth preparations were refined, and definitive impressions taken using addition silicone impression material. Centric relation recording and registration ensued.
During the laboratory steps care was taken to render all elements of interim restorations, namely the shape, the contours, the incisal edge position and the anterior guidance and occlusal parameters satisfactorily. The metal framework was constructed according to this information. The subsequent bisque try-in step was performed, forocclusion, marginal integrity, and anterior ceramic contours to be evaluated. The RPDs were connected to the FPDs via extra coronal precision attachments that provided increased retention and enhanced the esthetics of the definitive restoration. Moreover, porcelain denture teeth were selected to maintain the OVD achieved more securely, as occlusal stability was considered a high priority [14].
At the delivery appointment, final occlusal adjustments were made to ensure posterior stability [15] (Figure 7). The patient was delighted with the outcome and was accepting of the esthetics and function. He was given instructions regarding oral and denture hygiene, while regular follow-up appointments were scheduled.

Figure 7. Final result. Porcelain fused to metal FPDs combined with removable partial dentures (RPDs) establishing posterior occlusal stabilization and anterior guidance.
Discussion
There is no norm that works for every patient who has lost posterior support of the occlusion and suffers from consequent reduced dimension and anterior reverse articulation. Although a tailored approach is required, standard, established clinical and laboratory steps can methodically and predictably lead to the result anticipated. A thorough occlusal analysis is a fundamental step for the differential diagnosis of Pseudo-Class III malocclusion [4]. Αs in this case of reduced dimension with anterior reverse articulation, the OVD increase alone is the key step for the successful management of the case [15]. The diagnostic wax up is an essential tool that provides all necessary information to build an individualized, full mouth rehabilitation, while the final prostheses intended are designed and confirmed through the reversible and modifiable provisional phase [13]. Finally, appropriate recall and maintenance intervals ensure the longevity of hard and soft tissues, as well as that of the restorations.
Conclusion
The clinical case described above indicates that the prosthodontic management of pseudo-Class III malocclusion, when carefully planned, can be a safe procedure that aims to ensure the immediate and longitudinal improvement of a patient’s function and esthetics.
Author Contributions
Conceptualization: Ximinis E. Data curation: Ximinis E. Formal analysis: Naka O. Funding acquisition: N/A. Investigation: Tsiafitsa M. Methodology: Ximinis E. Project administration: Tsiafitsa M, Naka O. Resources: N/A. Software: Tsiafitsa M. Supervision: Naka O. Validation: Dionysopoulos D. Visualization: Ximinis E, Tsiafitsa M. Writing - original draft: Ximinis E, Tsiafitsa M. Writing - review & editing: Dionysopoulos D., Naka O.
Conflict of Interest
No potential conflict of interest relevant to this article has been reported
References
- Turner KA, Missirlian DM. Restoration of the extremely worn dentition. J Prosthet Dent 1984; 52: 467-474.
- Abduo J, Lyons K. Clinical considerations for increasing occlusal vertical dimension: a review. Aust Dent J 2012; 57: 2–10.
- Moyers RE. Handbook of Orthodontics. 4th ed. London: Year Book Medical Publishers; 1988.
- Cardoso AC, Ferreira CF, Oderich E, Pedroso ML, Wicks R. Occlusal rehabilitation of pseudo- Class III patient. J Prosthod 2015; 24: 78-82.
- Giancotti A, Maselli A, Mampieri G, Spanò E. Pseudo-Class III malocclusion treatment with Balters' Bionator, J Orthod 2003; 30: 203–215.
- Angle EM. Classification of malocclusion. Dental Cosmos 1899; 41: 248-264, 350-357.
- The Glossary of Prosthodontic Terms. 9th ed. J Prosthet Dent 2017; 5S: e1-e105.
- Igarashi Y, Yamashita S, Kyroiwa A. Changes in interarch distance and condylar position related to loss of occlusalsupport for partially edentulous patients. A pilot studies. Eur J ProsthodontRestor Dent 1999; 7: 107-111.
- Ngan P, Hu AM, Fields HW. Treatment of class III problems begins with differential diagnosis of anterior cross bites. Pediatric Dentistry 1997; 1: 386-395.
- Hagg U, Tse A, Bendeus M, Rabie ABM. A follow-up study of early treatment of pseudo class III malocclusion. Angle Orthodontist 2004; 74: 465-472.
- Bowman SJ. A quick fix for pseudo-class III correction. J Clin Orthod2008; 42: 691–697, 727.
- Lucia VO. A technique for recording centric relations. J Prosthet Dent 1964; 14: 492-505.
- Romeo G, Bresciano M. Diagnostic and technical approach to esthetic rehabilitations. J Esthet Restor Dent 2003; 15: 204-216.
- Ghazal M, Yang B, Ludwig K, Kern M. Two-body wear of resin and ceramic denture teeth in comparison to human enamel. Dent Mater 2008; 24: 502-507.
- Dawson PE. Functional occlusion. 1st ed. St Louis: CV Mosby; 2007.

