Abdominal Dystocia: A Case Report of a Fetal Abdominal Distention Leading to Labor Dystocia in Second Stage
Melissa Helmich*, Taylor Ghahremani and Nafisa Dajani
Department of Obstetrics and Gynecology, University of Arkansas for the Medical Sciences, Arkansas
Received Date: 14/05/2021; Published Date: 27/05/2021
*Corresponding author: Melissa Helmich, MD, Department of Obstetrics and Gynecology, University of Arkansas for the Medical Sciences, 4301 W. Markham St., Slot # 518, Little Rock, AR 72205-7199. Tel: 501-686-6797 Fax: 501- 526-5892, Email: mshelmich@uams.edu
The UAMS Institutional Review Board determined this study as not human subject research on October 2, 2019 (IRB # 260166).
Abstract
Many fetal diagnoses can result in fetal abdominal distention seen on prenatal ultrasound. Historically, abdominal decompression during the second stage of labor could allow for a vaginal delivery. Reports of abdominal dystocia are rare, leading to difficulty in predicting the success of a vaginal delivery. We present a 32-year-old Gravida 5 Para 3 at 36 2/7 weeks gestation who presented with preterm prelabor rupture of membranes (PPROM). The fetus had known bowel dilation and abdominal distention on prenatal ultrasonography. She was followed at our tertiary care center due to the abnormal fetal ultrasound. A multidisciplinary consult with pediatric surgery and maternal fetal medicine described no contraindications to a vaginal delivery. Once admitted for PPROM, induction of labor was recommended, but delivery was complicated by abdominal dystocia. This was relieved by emergent abdominal rescue using the Zavenelli maneuver and classical cesarean section. Clinicians should consider fetal abdominal distention as a possible source of labor dystocia; although anecdotally, this risk is small. We propose potential objective criteria for deciding route of delivery.
Keywords: Pregnancy; Abdominal dystocia; Labor dystocia; Fetal abdominal distention
Introduction
Labor dystocia is a known cause of maternal and fetal morbidity. Abdominal dystocia is a rare form of labor dystocia, likely caused by distention of the fetal abdomen. Fetal abdominal distention leading to dystocia may be caused by a multitude of fetal diagnoses including, but not limited to: intestinal obstruction, meconium peritonitis, colonic perforation, mega-cysts, polycystic kidneys, and ascites. With a limited amount of literature regarding abdominal labor dystocia specifically, providers may find themselves unprepared.
Case Report
We report a case of a 32-year-old Gravida 5 Para 3 pregnant patient, referred for collaborative care with Maternal Fetal Medicine, Neonatology, and Pediatric Surgery due to an abnormal prenatal ultrasound with echogenic and dilated fetal bowel. She had adequate prenatal care with an outside facility, including a normal glucose tolerance test. Workup included cystic fibrosis carrier testing and non-invasive prenatal genetic screening which were negative. At 34 weeks 3/7 days, prenatal ultrasound showed estimated fetal abdominal circumference at 37.2 cm (99th percentile) and largest bowel loop diameter dilated to 4.9 cm. [Figure 1] The fetal largest abdominal diameter, when measured retrospectively on prenatal images, was 13.4 cm. The amniotic fluid index was 20.2 cm. All teams agreed that, in this case, the abdomen should be considered compressible and not a contraindication to vaginal delivery.
At 36 weeks and 1/7 day, the patient presented to labor and delivery with preterm prelabor rupture of membranes (PPROM). The admission ultrasound was notable for fetal abdominal circumference of 46 cm and 14.0 cm at largest diameter, with stable bowel loops dilated to 4.8 cm. The patient had 3 prior vaginal deliveries, with the largest infant weighing 3.572 kg, the estimated fetal weight on admission was 3.8 kg. The patient was counseled on the fetus’ abdominal distention and the consulting services recommended labor, as the abdomen was considered compressible. The patient agreed to a vaginal delivery.
The patient’s labor progressed appropriately with oxytocin induction. She progressed to complete cervical dilation within 8 hours from admission. During the second stage of labor, the fetal head was delivered with a single maternal expulsive effort, but the remaining body did not deliver. Initially, a shoulder dystocia was presumed, but the fetal shoulders freely rotated without evidence of impacted shoulder. Episiotomy was performed to allow adequate room for examination. The posterior arm was delivered which allowed the anterior shoulder to deliver, but the delivering clinician was able to palpate in situ and confirmed that the abdominal girth remained above the pelvic inlet. Vaginal delivery efforts were halted. At this time, the posterior arm was replaced and the fetal head was elevated and supported as the patient was moved to the operating room.
Under general anesthesia, an abdominal rescue was performed via primary classical cesarean section. The fetal head could not be completely replaced into the vaginal canal to complete the Zavanelli maneuver until the hysterotomy was performed. Total time from vaginal delivery of the fetal head until abdominal birth was 12 minutes. A male infant weighing 3.17 kg was born with APGAR scores of 1, 4, and 7 at one, five, and ten minutes, respectively. The neonatal abdomen was distended, taut, and non-compressible upon neonatal examination. [Figure 2]. Cord blood gas pH studies were notable for an arterial pH of 7.0 and a base excess of -12.2 mmol/L. The neonate was intubated due to respiratory distress and transferred to the local children’s hospital for surgery. The neonate underwent exploratory laparotomy and had a large meconium cyst containing nearly 1 liter of fluid. There were several blind ending segments of the bowel. An end ileostomy was performed and later, two abdominal drains were placed. Newborn screening was initially abnormal for cystic fibrosis, but microarray was normal for genotypic male. Two months after delivery, he underwent a tapering jejunoplasty and was ultimately diagnosed with jejunal atresia. Most recently, the infant is in the care of his parents at home.
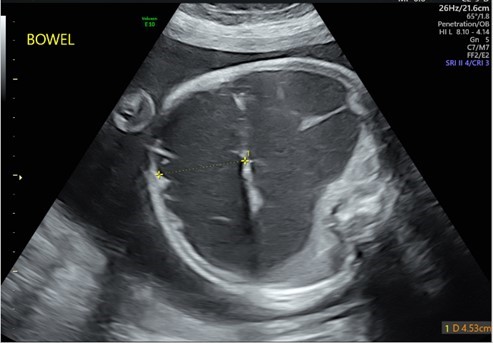
Figure 1: Prenatal ultrasound at 34 weeks gestation showing distention of bowel.
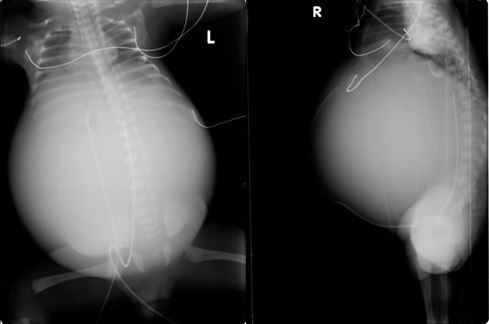
Figure 2: Rotund abdominal girth of neonate.
Discussion
In this case, the likelihood of abdominal dystocia was discussed during interdisciplinary delivery planning. It was felt to be unlikely given the patient’s multiparity with pelvis proven to 3.572 kg, the preterm gestational age, and the anticipated compressibility of the fetal abdomen. There is very little available literature in regards to abdominal dystocia, timing of delivery, and route of delivery. To our knowledge, five cases with abdominal dystocia have been reported in the literature [1- 4]. Four of these cases involved meconium peritonitis and were delivered abdominally. The first reported use of the Zavanelli maneuver for non-compressible abdominal dystocia was in 1994. The fetus had known gastroschisis, hydramnios, meconium peritonitis, and ascites [5]. The only vaginal delivery was a recent case report of abdominal dystocia due to fetal autosomal recessive renal polycystic kidney disease that was resolved with continued expulsive efforts and gentle fetal traction [4].
We propose the use of objective data to influence decisions about mode of delivery in patients at risk for abdominal dystocia. Abdominal dystocia is a known complication of fetal conditions with increased abdominal circumference, as the maternal bony pelvis has no laxity for fetal passage. Using available objective criteria, we recommend a cesarean delivery in cases of suspected meconium peritonitis on prenatal ultrasound accompanied by an accelerated abdominal circumference greater than the 99th percentile and an abdominal diameter larger than the fetal pelvic inlet diameter. According to a study of pelvic dimensions performed on CT/MRI scans of women with prior successful and uncomplicated vaginal births, the average maternal pelvic inlet transverse diameter measures 13.6cm +/- 0.7cm [6]. Extrapolating this information, fetuses with abdominal diameter greater than 14.3cm may be at greatest risk for abdominal dystocia, even if born to a woman with prior successful vaginal birth. Direct measurement of the pelvic inlet transverse diameter using imaging modalities prior to delivery may also be considered when considering a trial of labor in the patient with fetal abdominal distention. Clinical pelvimetry may also be useful, but lacks precision.
In conclusion, fetal abdominal dystocia is a rare event. In our case, the patient had a predictable, but unexpected outcome. We propose that objective data be used to decide mode of delivery in the setting of fetal abdominal distention, including clinical or imaging modalities to ascertain the maternal pelvis in conjunction with fetal biometry.
Authors’ Contributions
MH and TG involved in writing the original manuscript and literature search. ND provided edits and expert opinion. All authors approved the final draft. MH is the guarantor of this manuscript.
Competing Interests
The authors have nothing to disclose.
Grant Information
The authors received no specific funding for this work.
References
- Basu, D. and Thornton, J.G. Abdominal dystocia in a case of undetected intrauterine meconium peritonitis due to cystic fibrosis. Congenital Anomalies, 2007; 47: 72-73.
- Drips RC. Meconium peritonitis with massive abdominal distension resulting in dystocia. Report of a case. Obstet Gynecol 1966; 27: 335–337.
- Wall LA. Meconium peritonitis with ascites resulting in dystocia. Am J Obstet Gynecol 1959; 78: 1247–1249.
- Belin S, Delco C, Parvex P, et al. Management of delivery of a fetus with autosomal recessive polycystic kidney disease: a case report of abdominal dystocia and review of the literature. J Med Case Reports 2019; 13: 366.
- Hensleigh, P., Ray-Friele, E., et al. The Zavanelli Maneuver for Relief of Abdominal Dystocia Associated with Gastroschisis. International Journal of Gynecology & Obstetrics, 1995; 172(1): pp. 221–222.
- Salk, Ismail et al. “Pelvimetry by Three-Dimensional Computed Tomography in Non-Pregnant Multiparous Women Who Delivered Vaginally.” Polish journal of radiology 2016; 81: 219-27.

