Inhalation of a Dental Foreign Body in a Dentist's Office: An Exceptional Event!
Doaae El Ouaddane1,*, Badie Douqchi2, Akram Assadiki1, Ahmed Ahddadi1, Salima Hamraoui1 and Rachid Marouf1
1Department of Thoracic Surgery, Mohammed VI University Hospital, Faculty of Medicine and Pharmacy, Mohammed First University, Oujda, Morocco
2Department of Anesthesia and Reanimation, Mohammed VI University Hospital, Faculty of Medicine and Pharmacy, Mohammed First University, Oujda, Morocco
Received Date: 15/05/2025; Published Date: 20/06/2025
*Corresponding author: Doaae El Ouaddane, Department of Thoracic Surgery, Mohammed VI University Hospital , Faculty of Medicine and Pharmacy, Mohammed First University, Oujda, Morocco
Abstract
Foreign body aspiration is an uncommon complication of dental care, when it occurs directly, it generally involves a tool used by the practitioner.
We present a rather exceptional case of a dental foreign body (molar), it’s about a 7-year-old child was referred following the asymptomatic inhalation of a molar during dental surgery. Due to its sharp nature, the object required rapid extraction. It was located at the level of the left main bronchus and was removed with a rigid bronchoscope during short-term general anesthesia; we did not observe any lesions of the end bronchial mucosa.
Foreign body inhalation during dental care is uncommon and sometimes asymptomatic, good interrogation is necessary to react quickly.
Introduction
Aspiration of foreign material during dental treatment is a recognized and familiar phenomenon among orthodontists.
Dental treatment has a particularly risk for inhalation of foreign materials [1], although this is an uncommon complication in routine practice [2].
Case Report
A 7-year-old child was referred for the extraction of an end bronchial foreign body of dental origin, a molar, This is occurred during dental surgery, specifically the extraction of a severely decayed molar, which had accidentally been dropped by the dentist and subsequently lost sight of in the oropharynx, without causing any particular symptoms (Figure 1, 2). However, the nature of the object requires a rapid extraction and a visual inspection of the bronchial tree, the patient was therefore hospitalized at the hospital near his house, where the foreign body was located in the left lower lobe (Figure 3-6), unfortunately, as flexible bronchoscopy was not available, we received the patient in our hospital for an attempt to extract this foreign body, a procedure which seemes urgent given its relative proximity to the pulmonary vascular tree, leading to a risk of massive hemoptysis in the event of bronchial perforation .
We use for the procedure a 7.5 mm pediatric bronchoscope under short-term general anesthesia and laryngeal mask ventilation, we could visualize the foreign body in the left lower lobe bronchus, it was indeed a molar with a decayed area at the top, which could be easily extracted using forceps (Figure 7, 8), we did not observe any bronchial injury, the post-operative was uneventful and the patient the patient left the hospital less than 24 hours after the extraction.

Figures 1 and 2: Image showing the oral health of our patient; The arrow corresponds to the molar (foreign body).
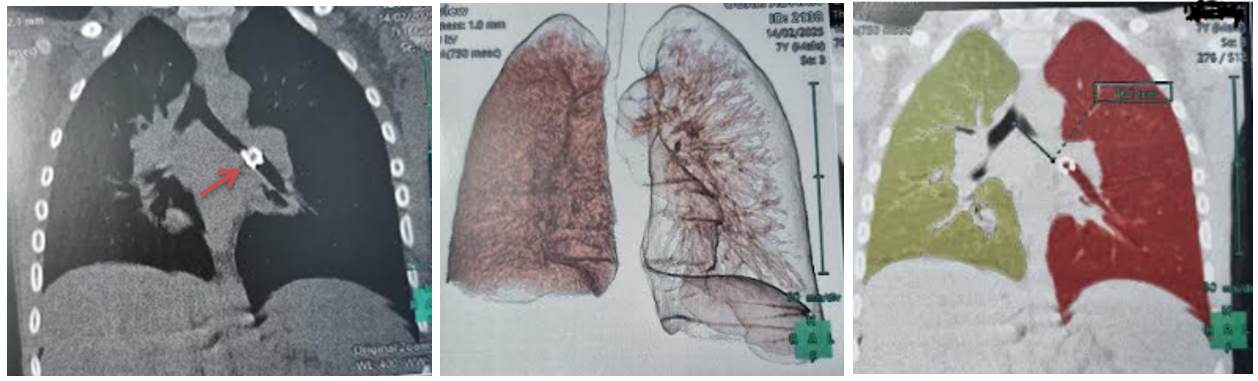
Figures 3 and 4: Image showing the CT image objectifying the opaque foreign body embedded in the left main bronchus.
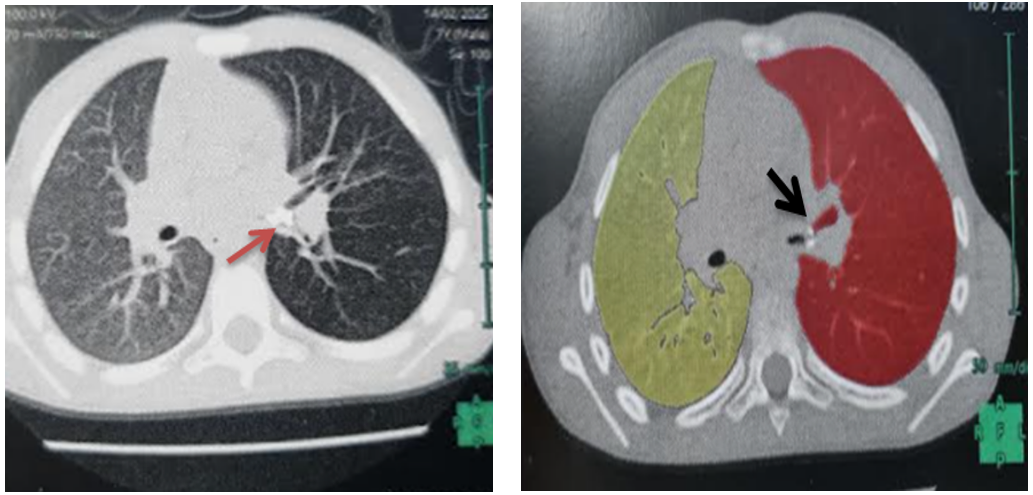
Figures 5 and 6: Axial CT scan showing the foreign body.
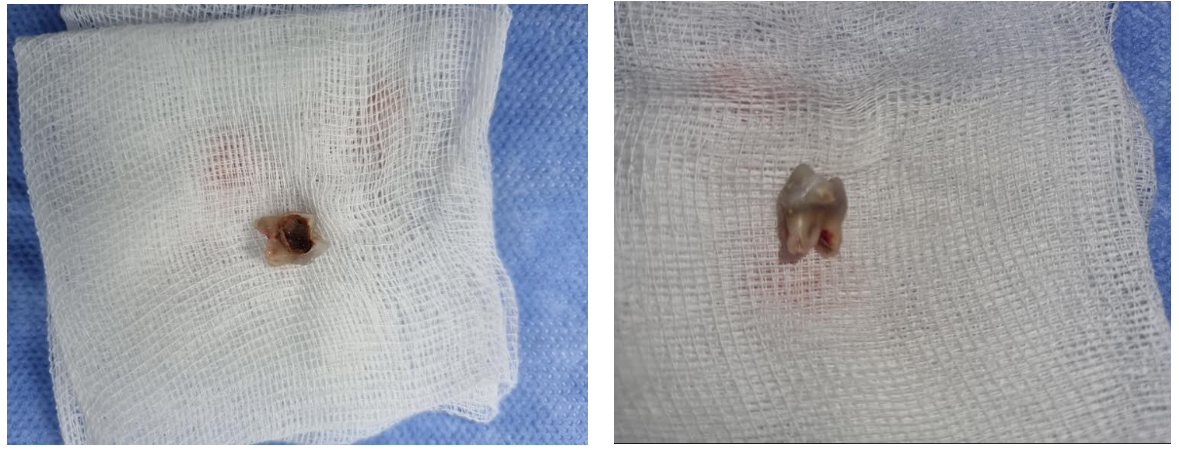
Figures 7 and 8: Foreign body (molar) after extraction.
Discussion
Aspiration of foreign material accounts for 13 to 20% of accidents in dental practice [3], leading to significant morbidity and even mortality related to obstruction of the upper airways, especially in childhood, It most often concerns procedures such as cementing or implanting dental crowns. However, the particular configuration of these objects can make their removal relatively difficult [4], the rate of 25% of aspiration accidents occur outside of dental’s office and then more frequently concern fixed dental equipment [3], however, as this observation shows, inhalation can also occur directly during treatment when the dentist handles small equipments or tries to remove baby teeth for children, even in the absence of local anesthesia of the mouth[2], many foreign bodies can therefore be inhaled [5]. The type and size of inhaled foreign bodies greatly influence the type of local tissue reaction and the symptomatology, thus, inert foreign bodies used in dental practice preferentially cause simple irritation of the mucosa with a low inflammatory component, the symptomatology is generally a dry cough which may be associated with dyspnea or stridor or even cardiorespiratory arrest if the foreign body causes an obstruction [5], in a quarter of cases, inhalation will remain completely asymptomatic [6]. On the other hand, certain objects may be sharp or pointed, leading to a risk of perforation of the bronchial mucosa with hemoptysis [7], distal migration is also possible, sometimes leading to surgical resection (lobectomy or wedge resection) [1], more rarely, the patient present a pneumothorax with subcutaneous emphysema, or even pneumomediastinum [8].
The radiological identification of non-radiopaque foreign bodies of dental origin can be complicated [2], that is gives the flexible endoscopy its place in the diagnostic assessment. On the other hand, thoracic CT scans are very sensitive for the detection of endobronchial foreign bodies, the risk observed of false positives, however, requires careful interpretation of the imaging [9], It can also be very useful for analyzing more precisely the reports of the foreign body with the surrounding structures, particularly the vascular axes, this makes it possible to assess the risk of hemoptysis and the degree of urgency of ablation.
Regarding therapeutic management, while asphyxiation is an urgent indication for clearing maneuvers and rigid bronchoscopy, flexible endoscopy is increasingly used for the resection of foreign bodies in the absence of signs of respiratory distress. These objects can then be collected using simple forceps or a trap designed for this purpose. This examination is more accessible and less expensive than rigid endoscopy. It also allows for the use of a shorter general anesthetic. CT reconstruction with virtual endoscopy (GPS) may also be useful in distal and peripheral locations [10] and may avoid rigid bronchoscopy or surgery. Although several cases of ablation under local anesthesia have been reported in dental practice, it seems preferable to perform a short general anesthesia and monitoring of vital parameters.
Conflict of Interest: The authors declared that they have no conflict of interest.
Grant Information: The author(s) received no specific funding for this work.
Acknowledgement: The authors have no acknowledgements to declare.
References
- Gregori D, Salerni L, Scarinzi C, Morra B, Berchialla P, Snidero S, et al. Foreign bodies in the upper airways causing complications and requiring in children aged 0-14 years: results from the ESFBI study. Eur Arch Otorhinolaryngol, 2008; 265(8): 971-978.
- Colchen A, Fischler M. Bronchoscopies interventionnelles en urgence. Rev Pneumol Clin, 2011; 67(4): 209-213.
- Huang HJ, Fang HY, Chen HC, Wu CY, Cheng CY, Chang CL. Three-dimensional computed tomography for detection of tracheobronchial foreign body aspiration in children. Pediatr Surg Int, 2008; 24(2): 157-160.
- Ouoba K, Iara CD, Dao MO, Ouegraogo I, Anou IS, Cissé R. Les corps étrangers laryngotrachéobronchiques chez l’enfant au CHU de Ouagadougou (une analyse de 96 observations). Med Trop, 2002; 62(6): 611-614.
- Bergermann M, Donald PJ, Wengen DF. Screwdriver aspiration. A complication of dental implant placement. Int J Oral Maxillofac Surg, 1992; 21: 339–341.
- Hodges ED, Durham TM, Stanley RT. Management of aspiration and swallowing incidents: a review of the literature and report of case. ASDC J Dent Child, 1992; 59(6): 413–419.
- Heimlich HJ. The Heimlich maneuver: prevention of death from choking on foreign bodies. J Occup Med, 1977; 19: 208–210.
- Vincent M, Vergnon J-M. Corps étrangers d’origine dentaire : comment ramener la fraise du dentiste ? Revue des Maladies Respiratoires, 2015.
- Chen LH, Zhang X, Li SQ, Liu YQ, Zhang TY, Wu JZ. The risk factors for hypoxemia in children younger than 5 years old undergoing rigid bronchoscopy for foreign body removal. Anesth Analg, 2009; 109(4): 1079-1088.
- Fidkowski CW, Zheng H, Firth PG. The anesthetic considerations of tracheobronchial foreign bodies in children: a literature review of 12,979 cases. Anesth Analg, 2010; 111(4): 1016-1025.

