A Mini Review on Neuroprotective Effect of Antioxidant in The Brain
Aimi Syamima Abdul Manap1,* and Rubaiyat Siddique Diba2
1Department of Biomedical Science, College of Veterinary Medicine, King Faisal University, Al-Hofuf, Saudi Arabia
2Independent researcher
Received Date: 06/04/2025; Published Date: 14/05/2025
*Corresponding author: Aimi Syamima Abdul Manap, Department of Biomedical Science, College of Veterinary Medicine, King Faisal University, Al-Hofuf, Saudi Arabia
Abstract
The brain's high energy needs, ample lipid content, and poor antioxidant capability make it susceptible to severe oxidative damage. In neurodegenerative illnesses, Reactive Oxygen Species (ROS) cause oxidative alterations in the brain that increase vulnerability to neuronal damage and functional impairments. The physiological roles of antioxidants in the brain, intracellular signaling, and cellular defense mechanisms all control excessive and aberrant amounts of ROS and/or metal overload. Numerous preclinical and clinical studies have assessed single and/or complex antioxidant chemicals that target oxidative stress, redox metals, and neuronal cell death as an additional therapeutic approach to address oxidative stress linked to neurodegenerative processes. In this mini review, we provide a latest overview and analysis of different antioxidants and offer possible antioxidant therapy plans for the brain's neuroprotection against oxidative damage. The relative benefits and methodological issues for evaluating antioxidant chemicals for the treatment of neurodegenerative diseases are examined in this review, which focuses on enzymatic and non-enzymatic antioxidant systems in the brain.
Introduction
The brain's high energy demands make it especially vulnerable to oxidative stress, which arises when Reactive Oxygen Species (ROS) accumulate beyond the body's ability to neutralize them with antioxidants [1]. Much like a finely calibrated engine that requires precise fuel and upkeep, maintaining a delicate balance is crucial for sustaining cellular function and overall neurological health. When this equilibrium is disrupted, excessive ROS trigger oxidative damage, compromising neuronal integrity and impairing cognitive processes [2].
Under normal physiological conditions, cells regulate Reactive Oxygen Species (ROS) to prevent potential harm. However, when ROS levels surpass the body’s antioxidant defences, oxidative stress ensues, leading to cellular damage. The brain, despite comprising only 2% of total body mass, requires nearly 20% of the body's oxygen supply, making it particularly susceptible to oxidative stress [3]. Its high concentration of Polyunsaturated Fatty Acids (PUFAs) in neuronal membranes further increases the risk of lipid peroxidation, a process that weakens cell structure and disrupts neural signalling [4]. Compounding this vulnerability, the brain has relatively low antioxidant reserves, leaving neurons highly exposed to oxidative injury. Once oxidative stress sets in, it can compromise key biomolecules damaging lipids, proteins, and nucleic acids. Lipid peroxidation deteriorates cell membranes, protein oxidation disrupts enzymatic functions, and oxidative DNA damage impairs gene expression, collectively endangering neuronal survival [5]. Chronic oxidative damage has been strongly associated with neurodegenerative diseases such as Alzheimer’s, Parkinson’s, and ALS, contributing to protein misfolding, mitochondrial dysfunction, and progressive neuron loss [6]. Beyond these conditions, oxidative stress is also implicated in cognitive decline and psychiatric disorders, where imbalances in neurotransmitters and heightened neuroinflammation impact overall mental health [7].
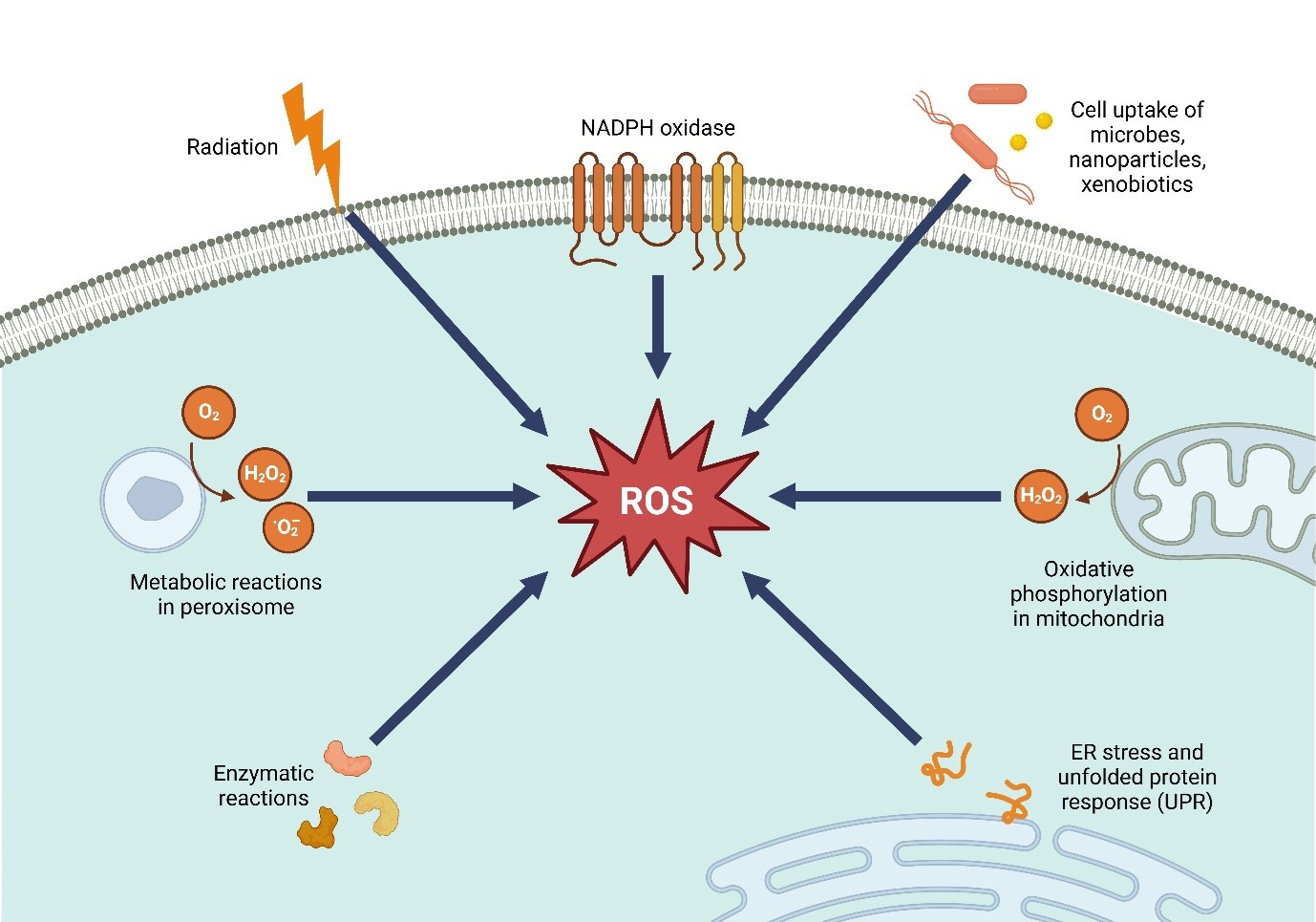
Figure 1: Sources of Reactive Oxygen Species (ROS).
Given the recognized role of oxidative stress in neurological diseases, scientists continue to investigate the potential of antioxidants in mitigating its effects. Understanding how antioxidants interact with ROS and support neuronal resilience has become a critical area of neuroprotective research. While studies highlight promising benefits, challenges remain in determining the clinical efficacy of antioxidant-based interventions due to variations in dosage, bioavailability, and the complex interplay of oxidative pathways. Ongoing research seeks to optimize these strategies, offering new possibilities for slowing neurodegeneration and preserving cognitive health.
Factors that contribute to the brain’s vulnerability to oxidative stress
The brain’s vulnerability to oxidative damage arises from a combination of metabolic inefficiencies, structural sensitivities, and environmental stressors that accelerate cellular deterioration over time , a key driver of this damage is mitochondrial dysfunction [5]. As the primary energy source for neurons, mitochondria generate ATP to sustain brain function. However, aging, genetic mutations, and metabolic stress can compromise mitochondrial efficiency, leading to excessive Reactive Oxygen Species (ROS) production. Once damaged, mitochondria struggle to regulate oxidative balance, triggering a self-perpetuating cycle of energy depletion, oxidative stress, and neuronal degeneration. This decline is particularly evident in neurodegenerative diseases like Alzheimer’s and Parkinson’s, where mitochondrial damage both drives and results from disease progression [8].
Beyond mitochondrial instability, the brain’s biochemical environment intensifies oxidative stress. Redox-active metals such as iron and copper contribute to ROS generation through Fenton reactions, making neurons highly susceptible to oxidative injury. While these metals are vital for neurotransmitter synthesis and enzymatic activity, their dysregulation promotes the formation of hydroxyl radicals, which aggressively degrade cellular structures [9]. This imbalance is a hallmark of neurodegeneration, with iron accumulation commonly observed in affected brain regions, such as the substantia nigra in Parkinson’s disease [10]. Additionally, disruptions in calcium regulation overstimulate neuronal activity, increasing ROS production and impairing mitochondrial resilience. External influences further compound oxidative stress. As the brain ages, its ability to neutralize ROS declines, with antioxidant enzyme levels decreasing while oxidative damage accumulates in cellular components [11]. Environmental toxins such as heavy metals, pesticides, and airborne pollutants cross the blood-brain barrier, triggering inflammatory responses and further elevating ROS production. Long-term exposure to polluted environments has been linked to accelerated cognitive decline and a heightened risk of neurodegenerative disorders (Dhapola et al., 2023).
Diet and metabolic health also play a crucial role. Deficiencies in antioxidants like vitamins C and E, selenium, and polyphenols weaken neuronal defences, while diets high in processed sugars and unhealthy fats contribute to metabolic stress, insulin resistance, and chronic inflammation all of which amplify oxidative damage [12]. Obesity and diabetes, both associated with systemic inflammation, further impair mitochondrial function and glucose metabolism, increasing susceptibility to cognitive impairment and neurodegenerative diseases such as Alzheimer’s [13].
Lastly, chronic psychological stress significantly impacts oxidative balance. Persistent elevation of cortisol can impair mitochondrial function, suppress antioxidant defences, and promote neuroinflammation, accelerating brain aging [14]. Research links prolonged stress with oxidative damage in key cognitive regions like the hippocampus, which is essential for memory and emotional regulation [7]. This explains why individuals experiencing chronic stress or depression often exhibit higher oxidative stress markers, predisposing them to neurodegenerative conditions. Together, these interconnected factors create a highly oxidative environment in the brain, increasing neuronal vulnerability to long-term damage. As research advances, targeting both biological vulnerabilities and modifiable risk factors remains essential in preserving cognitive health and reducing the onset of neurodegenerative diseases.
Neuroprotective activity from antioxidants
Antioxidants serve as vital defenders against oxidative damage, a key driver of neurodegeneration. Their primary role is to neutralize reactive oxygen and nitrogen species (ROS/RNS) before these unstable molecules can inflict harm on neuronal membranes, proteins, and DNA. By safeguarding mitochondrial function, antioxidants ensure efficient energy production, preventing the cellular dysfunction that leads to neuronal death. Additionally, they curb the activation of inflammatory pathways triggered by excessive ROS, reducing neuroinflammation and preserving overall brain health.Neurons rely on a sophisticated antioxidant defense system consisting of enzymatic and non-enzymatic components, which work in unison to counteract oxidative stress. Beyond merely scavenging free radicals, antioxidants also contribute to the repair of oxidized biomolecules, helping maintain cellular integrity. Their protective effect is particularly crucial in preventing lipid peroxidation within neuronal membranes, intervening at key stages such as initiation, propagation, and chain termination. This function plays a significant role in halting ferroptosis an iron-dependent form of cell death associated with neurodegenerative diseases.
As research continues to unravel the intricate ways antioxidants support brain function, they are becoming central to the development of strategies aimed at slowing cognitive decline and mitigating the progression of neurodegenerative disorders. This section delves into the latest findings on the neuroprotective potential of various antioxidants and their impact on brain health.
Table 1: Summary on Neuroprotective activity of various antioxidants in the brain.
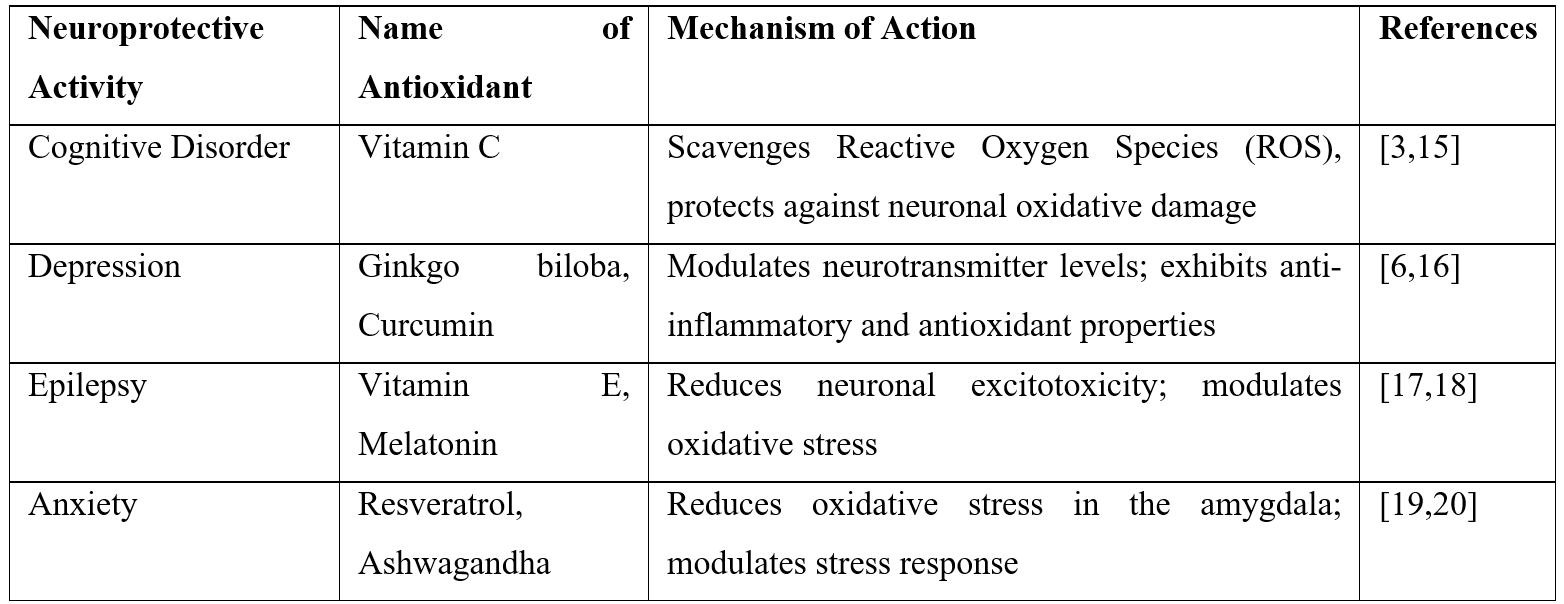
Cognitive Disorder
Oxidative stress is a key contributor to cognitive decline, accelerating neuronal damage and memory impairment. In conditions such as Mild Cognitive Impairment (MCI) and dementia, an excess of Reactive Oxygen Species (ROS) overwhelms the brain’s natural antioxidant defenses, leading to synaptic dysfunction and neuronal loss [6] This persistent oxidative burden fuels neurodegenerative processes, gradually worsening cognitive function over time.
Enhancing antioxidant defenses has demonstrated neuroprotective effects in these conditions [21]. Long-term consumption of antioxidant-rich nutrients, including vitamins and polyphenols, has been linked to a slower progression of Alzheimer’s disease, suggesting that strengthening the brain’s redox balance can help maintain cognitive function [22]. Notably, the carotenoid astaxanthin has been shown to mitigate memory deficits and even reverse Alzheimer-like pathology in experimental models by reducing amyloid and tau accumulation while restoring glutathione levels [23]. By neutralizing free radicals and preventing lipid peroxidation, antioxidants play a crucial role in preserving neuronal integrity and delaying age-related cognitive decline [4].
Depression
Major depressive disorder has been closely associated with increased oxidative stress in the brain. Individuals with depression often display higher levels of oxidative damage markers, such as malondialdehyde and 8-OHdG, along with a decline in key antioxidant defenses like Superoxide Dismutase (SOD) and glutathione [24,25]. This imbalance suggests that an excess of Reactive Oxygen Species (ROS) and a weakened antioxidant system contribute to neuroinflammation and neuronal dysfunction, both of which are implicated in depressive symptoms.
Strengthening antioxidant defenses has shown promise in alleviating depression [26]. Many conventional antidepressants naturally enhance antioxidant enzyme activity while reducing oxidative stress markers. Likewise, certain antioxidants have demonstrated antidepressant-like effects. For example, research has found that diallyl disulfide, an antioxidant derived from garlic, reversed inflammation-induced depressive behaviours in animal models [27]. By mitigating oxidative damage, antioxidants help regulate neurotransmitter levels and support neurotrophic factors, ultimately improving mood and cognitive function in individuals with depression.
Epilepsy
In epilepsy, recurrent seizures and oxidative stress create a self-perpetuating cycle that worsens neuronal damage [28]. Seizure activity triggers a surge in Reactive Oxygen Species (ROS), leading to lipid peroxidation and cellular injury, which further increases the brain’s vulnerability to future seizures [29]. As a result, many epilepsy patients exhibit elevated oxidative damage in neural tissues, with oxidative stress acting both as a trigger and a consequence of epileptic activity.
Breaking this cycle with antioxidant interventions offers a promising neuroprotective approach. Various antioxidants, including vitamin E, resveratrol, and curcumin, have shown anticonvulsant properties, reducing both seizure frequency and neuronal damage [30]. Notably, curcumin, when used as an adjunct therapy, has improved outcomes in treatment-resistant epilepsy, while melatonin, a powerful endogenous antioxidant, has demonstrated the ability to reduce seizures and oxidative damage in both experimental and clinical studies [31]. By neutralizing free radicals and preserving mitochondrial function, these antioxidants help sustain neuronal integrity and mitigate the neurotoxic cascade associated with epilepsy.
Anxiety
Anxiety disorders have been closely associated with oxidative stress and an imbalanced redox state in the brain. Chronic stress and heightened anxiety levels contribute to excessive production of Reactive Oxygen Species (ROS), overwhelming the brain’s natural antioxidant defenses and leading to neuronal damage [32]. This oxidative burden disrupts neurotransmission altering monoamine function and promoting neuroinflammation which may further reinforce the neural circuitry changes underlying pathological anxiety.
Strengthening the brain’s antioxidant system has shown promising anxiolytic effects. Both preclinical and clinical studies indicate that compounds such as N-acetylcysteine (a precursor to glutathione), sulforaphane, and certain flavonoids can alleviate anxiety by reducing oxidative damage and inflammation [33]. For instance, resveratrol, a polyphenol, significantly improved anxiety-like behaviours in stressed rodents by restoring oxidative balance, enhancing neuroplasticity, and stabilizing neurotransmitter levels [34]. By counteracting oxidative stress, antioxidants help protect against stress-induced neuronal dysfunction and support the biological pathways that regulate anxiety, ultimately promoting a neuroprotective and calming effect [19].
Conclusion
In conclusion, the antioxidants discussed in this article highlight the significant potential of natural compounds in providing neuroprotection for various brain-related conditions such as cognitive disorders, depression, epilepsy, and anxiety. These antioxidants work by combating oxidative stress, reducing inflammation, and promoting cellular repair, all of which are essential in maintaining brain health and mitigating damage from neurodegenerative diseases. While more research is needed to fully understand their therapeutic efficacy and optimal use, these antioxidants offer promising avenues for future treatments. Incorporating them into clinical strategies could potentially improve patient outcomes and provide safer, more effective alternatives or adjuncts to current therapies for brain illnesses.
Conflicts of interest: The authors declare no conflict of interest.
Funding: The authors declared that there is no funding received for this article.
References
- Singh A, et al. ‘Oxidative stress: a key modulator in neurodegenerative diseases’, Molecules, 2019; 24(8): p. 1583.
- Jaganjac M, et al. ‘Oxidative stress and regeneration’, Free Radical Biology and Medicine, 2022; 181: pp. 154–165.
- Franzoni F, et al. ‘Oxidative stress and cognitive decline: the neuroprotective role of natural antioxidants’, Frontiers in neuroscience, 2021; 15: p. 729757.
- Petrovic S, et al. ‘Lipid peroxidation and antioxidant supplementation in neurodegenerative diseases: a review of human studies’, Antioxidants, 2020; 9(11): p. 1128.
- Hajam YA, et al. ‘Oxidative stress in human pathology and aging: molecular mechanisms and perspectives’, Cells, 2022; 11(3): p. 552.
- Olufunmilayo EO, Gerke-Duncan MB, Holsinger RD. ‘Oxidative stress and antioxidants in neurodegenerative disorders’, Antioxidants, 2023; 12(2): p. 517.
- Balmus IM, et al. ‘Oxidative stress implications in the affective disorders: main biomarkers, animal models relevance, genetic perspectives, and antioxidant approaches’, Oxidative medicine and cellular longevity, 2016; 2016(1): p. 3975101.
- Ng SC, et al. ‘Free radical chain reactions and polyunsaturated fatty acids in brain lipids’, ACS omega, 2022; 7(29): pp. 25337–25345.
- Huat TJ, et al. ‘Metal toxicity links to Alzheimer’s disease and neuroinflammation’, Journal of molecular biology, 2019; 431(9): pp. 1843–1868.
- Levi S, et al. ‘Iron imbalance in neurodegeneration’, Molecular psychiatry, 2024; 29(4): pp. 1139–1152.
- Asatiani N, et al. ‘Blood Catalase, Superoxide Dismutase, and Glutathione Peroxidase Activities in Alcohol-and Opioid-Addicted Patients’, Medicina, 2025; 61(2): p. 204.
- Pérez-Torres I, et al. ‘Oxidative stress, plant natural antioxidants, and obesity’, International journal of molecular sciences, 2021; 22(4): p. 1786.
- Pugazhenthi S, Qin L, Reddy PH. ‘Common neurodegenerative pathways in obesity, diabetes, and Alzheimer’s disease’, Biochimica et biophysica acta (BBA)-molecular basis of disease, 2017; 1863(5): pp. 1037–1045.
- Sayre LM, Perry G, Smith MA. ‘Oxidative stress and neurotoxicity’, Chemical research in toxicology, 2008; 21(1): pp. 172–188.
- Sharma S, Opyrchal M, Lu X. ‘Harnessing tumorous flaws for immune supremacy: is miRNA-155 the weak link in breast cancer progression?’, Journal of Clinical Investigation, 2022; 132(19): p. e163010.
- Lin J, Sun X, Yang L. ‘Effects and safety of Ginkgo biloba on depression: a systematic review and meta-analysis’, Frontiers in Pharmacology, 2024; 15: p. 1364030.
- Madireddy Sahithi, Madireddy Samskruthi. ‘Therapeutic strategies to ameliorate neuronal damage in epilepsy by regulating oxidative stress, mitochondrial dysfunction, and neuroinflammation’, Brain sciences, 2023; 13(5): p. 784.
- de Melo AD, et al. ‘Antioxidant Therapy Reduces Oxidative Stress, Restores Na, K-ATPase function and induces neuroprotection in rodent models of seizure and epilepsy: a systematic review and meta-analysis’, Antioxidants, 2023; 12(7): p. 1397.
- Tseilikman VE, et al. ‘Unraveling the Liver–Brain Axis: Resveratrol’s Modulation of Key Enzymes in Stress-Related Anxiety’, Biomedicines, 2024; 12(9): p. 2063.
- Mikulska P, et al. ‘Ashwagandha (Withania somnifera)—current research on the health-promoting activities: a narrative review’, Pharmaceutics, 2023; 15(4): p. 1057.
- Lee KH, Cha M, Lee BH. ‘Neuroprotective effect of antioxidants in the brain’, International journal of molecular sciences, 2020; 21(19): p. 7152.
- Pritam P, et al. ‘Antioxidants in Alzheimer’s disease: Current therapeutic significance and future prospects’, Biology, 2022; 11(2): p. 212.
- Rahman SO, et al. ‘Neuroprotective role of astaxanthin in hippocampal insulin resistance induced by Aβ peptides in animal model of Alzheimer’s disease’, Biomedicine & Pharmacotherapy, 2019; 110: pp. 47–58.
- Liu T, et al. ‘A meta-analysis of oxidative stress markers in depression’, PloS one, 2015; 10(10): p.e0138904.
- Lindqvist D, et al. ‘Oxidative stress, inflammation and treatment response in major depression’, Psychoneuroendocrinology, 2017; 76: pp. 197–205.
- Visentin APV, et al. ‘Targeting inflammatory‐mitochondrial response in major depression: current evidence and further challenges’, Oxidative medicine and cellular longevity, 2020; 2020(1): p. 2972968.
- Wei X, et al. ‘Acute diallyl disulfide administration prevents and reveres lipopolysaccharide-induced depression-like behaviors in mice via regulating neuroinflammation and oxido-nitrosative stress’, Inflammation, 2021; 44: pp. 1381–1395.
- Khurana DS, et al. ‘Mitochondrial dysfunction in epilepsy’, in. Seminars in pediatric neurology, Elsevier, 2013; pp. 176–187.
- Firdous SM, Mallik S, Paria B. ‘Antioxidant Effects of Medicinal Plants for the Treatment of Epilepsy’, Antioxidants: Nature’s Defense Against Disease, 2025; pp. 441–489.
- Grabarczyk M, et al. ‘Role of plant phytochemicals: resveratrol, curcumin, luteolin and quercetin in demyelination, neurodegeneration, and epilepsy’, Antioxidants, 2024; 13(11): p. 1364.
- Kamieniak M, et al. ‘The Oxidative Stress in Epilepsy—Focus on Melatonin’, International journal of molecular sciences, 2024; 25(23): p. 12943.
- Liu F, et al. ‘Antioxidants in neuropsychiatric disorder prevention: neuroprotection, synaptic regulation, microglia modulation, and neurotrophic effects’, Frontiers in Neuroscience, 2024; 18: p. 1505153.
- Rossetti AC, et al. ‘Oxidation-reduction mechanisms in psychiatric disorders: A novel target for pharmacological intervention’, Pharmacology & Therapeutics, 2020; 210: p. 107520.
- Socała K, et al. ‘Therapeutic potential of stilbenes in neuropsychiatric and neurological disorders: A comprehensive review of preclinical and clinical evidence’, Phytotherapy Research, 2024; 38(3): pp. 1400–1461.

