Fournier's Gangrene on Urethral Stenosis
Nachid A*, Safwate R, Ouzidane Y, Kbirou A, Moataz A, Dakir M, Debbagh A and Aboutaieb R
Department of Urology, CHU IBN Rochd Casablanca, Morocco
Received Date: 27/02/2025; Published Date: 08/05/2025
*Corresponding author: Nachid A, Department of Urology, CHU IBN Rochd Casablanca, Morocco
Abstract
Fournier's Gangrene (FG) and penile gangrene are life-threatening conditions characterized by rapid tissue necrosis due to bacterial infection, typically involving the perineum and genitalia. We present two cases that highlight the challenges in diagnosis and management, emphasizing the importance of early surgical intervention, broad-spectrum antibiotics, and supportive care for improving patient outcomes.
We report the case of two patients treated in our facility, with favorable postoperative outcomes.
Keywords: Penil gangrene; Frounier’s gangrene; Urethral stenosis; Recurrence
Introduction
Penil and Fournier’s gangrene, is a rapidly progressive, necrotizing infection of the perineal, genital, or perianal regions. It typically arises from polymicrobial infections and is most commonly seen in individuals with underlying risk factors such as diabetes, obesity,renal failure or immunosuppression. The condition is characterized by severe pain, swelling, erythema, and necrosis, which can progress to systemic sepsis if untreated. Early diagnosis and aggressive management, including surgical debridement and broad-spectrum antibiotics, are critical for patient survival.
Imaging, without delaying surgical intervention, primarily relies on computed tomography and scrotal ultrasound. During management, it is essential to consider a proctological examination, retrograde urography, and the potential need for stool and urine diversion.
Case Report
Case 1: A 58-year-old patient with no comorbidities, hospitalized two years ago for fournier's gangrene secondary to ureteral stenosis for which he undergone necrosectomy and derivation of the bladder, which was removed after skin recovery.
He presented to the emergency department for a recurrence of the symptomatology with appearance of necrotic areas on the penis and bursae (Figure 1) preceded by dysuria and increased bursal size, which had been evolving for 10 days.
On clinical examination, we find a conscious patient, HD stable and respiratory, a 39,3 fever. On examination of the external genitalia, necrosis of the glans and scrotal sacs was containing a collection (Figure…). The biological assessment showed a leukocytosis at 23 540/mm, elevated CRP at 446 mg/L, a renal failure at 68,2mg/L of creat, urea at 1,43g/L with no renal dilatation.
Patient received intravenous antibiotic: ceftriaxone, gentamycin and metronidazole and was rushed to the operating room where he underwent a urethroscopy objectifying several ureteral strictures (Figure 2) and a necrosectomy revealing a 1cm defect in the bulbo membranous ureter (Figure 3).
The postoperative follow-ups were normal, with normalization of the biological balance, the patient was declared outgoing on day 5.

Figure 1: Clinical appearance of necrosis in the genital region.

Figure 2: Endoscopic appearance of urethral stricture.

Figure 3: Intraoperative appearance of urethral tissue loss.
Case 2:
An 82-year-old with no comorbidities presented with symptoms of lower urinary tract obstruction for a year, which progressed to necrosis of the glans and part of the penis 15 days before admission.
Clinical examination revealed necrosis of the glans with an abscessed penile skin containing greenish fluid, while the scrotum and perineum were intact (Figure 4). Laboratory tests showed leukocytosis (12,000/mm³), elevated CRP (215 mg/L), and normal renal function.
The patient was hospitalized urgently, started on broad-spectrum antibiotics, and underwent emergency necrosectomy to remove necrotic tissue.
Further investigation revealed urethral strictures (Figure 5) managed by cold-blade urethrotomy. A definitive perineostomy was performed for urinary diversion (Figure 6), and the patient recovered well, being discharged on day 7 with normalized lab results.

Figure 4: Penile gangrene.
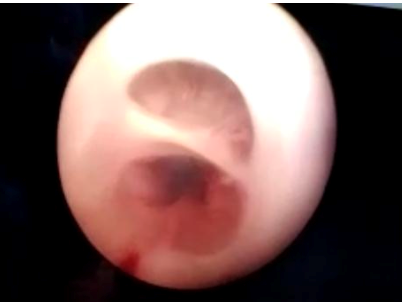
Figure 5: Urethral structure.

Figure 6: Perineostomy.
Discussion
Fournier’s gangrene is a fast-progressing necrotizing infection that affects the external genitalia and frequently extends to the perineum [1].
Ischemic gangrene of the penis is extremely rare due to its rich blood supply but carries high morbidity and mortality due to the substantial risk of sepsis [2].
Identifying the exact portal of entry is often difficult. Fournier’s gangrene has been linked to several risk factors, including advanced age, diabetes, alcoholism, immunosuppression (e.g., HIV), and obesity. Early symptoms are often nonspecific, resembling cellulitis with erythema and induration. As the condition progresses, necrosis and the characteristic signs of Fournier’s gangrene develop, with patients frequently presenting to the hospital in severe or septic states [1]. The infection typically has a polymicrobial origin, with Group A streptococcus being the most commonly detected organism, though the underlying cause remains poorly understood [3].
Various imaging techniques help assess the presence of air and the extent of infection in Fournier’s Gangrene (FG). Standard radiography is a quick, effective tool as 90% of FG cases show subcutaneous emphysema, while ultrasonography can detect subcutaneous gas as “dirty” acoustic shadowing. Computed Tomography (CT) is the most specific imaging modality for infection extent, aiding surgical planning, while Magnetic Resonance Imaging (MRI) is reserved for unclear cases but should not delay surgery due to FG’s rapid progression [4]. Neither patient underwent imaging, given the advanced stage of the disease.
Managing Fournier’s Gangrene (FG) is challenging due to its nonspecific symptoms and rapid necrotic progression. Treatment involves hemodynamic stabilization, broad-spectrum antibiotics, and urgent surgical debridement to remove all necrotic tissue until viable tissue is reached. Prompt removal of necrotic tissue is essential to prevent infection spread, though debridement often results in significant tissue deficits. A retrospective study of 72 FG patients linked delayed debridement to significantly higher mortality, emphasizing the importance of timely and extensive intervention for improved outcomes [4].
Gangrene can be classified into two types: dry gangrene and wet gangrene, the latter characterized by secondary infection. Dry gangrene is typically managed conservatively, whereas partial or total penectomy is indicated for wet gangrene with tissue infection. The use of a tourniquet during surgery is contraindicated to avoid increasing ischemic areas, a precaution that was observed during our procedure [5,6].
Following surgical debridement, effective local wound care is essential and often involves techniques such as vacuum-assisted closure (VAC) devices or wet-to-dry dressings. Once granulation tissue forms, patients typically require reconstructive surgery to provide adequate tissue coverage for the affected area.
Conclusion
Fournier’s gangrene is a rapidly progressing necrotizing infection with high morbidity and mortality, especially in severe or septic cases. Early diagnosis is challenging due to nonspecific symptoms, making prompt surgical debridement and broad-spectrum antibiotics essential for survival. Imaging techniques like CT scans help assess the infection’s extent, but surgical intervention should not be delayed. Postoperative wound care, including vacuum-assisted closure or wet-to-dry dressings, is crucial for recovery and tissue regeneration. A multidisciplinary approach is necessary to improve patient outcomes and reduce complications.
Conflicts of interest: None
Funding: None
References
- Duong A, Slader M, Florian J, Smart J. A Case Report of Fournier’s Gangrene, 2022.
- Hernández Martínez JO, Bertrand Noriega F, Ramírez Pedraza JM, Cosío Álvarez RA. Ischemic gangrene of the penis due to Fournier’s gangrene following traumatic transurethral catheterization: A case report. Urology Case Reports, 2024; 56: 102820.
- Chhetri ST, Sah SK, Pathak ID, Pokhrel N, Thyayat PK, Shah NK. Fournier’s gangrene in elderly men: A report of two cases. International Journal of Surgery Case Reports, 2025; 126: 110734.
- Lewis GD, Majeed M, Olang CA, Patel A, Gorantla VR, Davis N, et al. Fournier’s Gangrene Diagnosis and Treatment: A Systematic Review. Cureus, 2021.
- Complete gangrene of penis in patient with arterial vascular disease. Urology, 2004; 64: 1231.e4–1231.
- Weiner DM, Lowe FC. Surgical management of ischemic penile gangrene in diabetics with end stage atherosclerosis. J Urol, 1996; 155: 926–929.

