Hematemesis Revealing a Primary Aortodigestive Fistula
Meryem Sassi, Hamid Jiber, Samir El Youbi, Hamza Naouli and Abdellatif Bouarhroum
Faculty of Medicine and Pharmacy of Fez, Sidi Mohamed Ben Abdellah University, Morocco
Received Date: 03/04/2025; Published Date: 05/05/2025
*Corresponding author: Meryem Sassi, Faculty of Medicine and Pharmacy of Fez, Sidi Mohamed Ben Abdellah University, Morocco
Abstract
Primary aortodigestive fistulas are most often caused by erosion of the intestinal wall by an abdominal aortic aneurysm. Infectious aortitis, with formation of a false aneurysm and eventual erosion into the duodenum, is a rare cause and has been described in very few patients in the literature.
We report a case of a female patient who was admitted to the emergency unit for hematemesis.
CT-scan in favour of inflammatory aortitis complicated by two partially thrombosed false aneurysms of the subrenal abdominal aorta fistulized in the lumen of the 3rd portion of the duodenum.
The procedure involved resection of the aorta on both sides of the aneurysm, with insertion of a reinforced PTFE prosthesis and suture of the duodenal breach.
Keywords: Gastrointestinal bleeding; Abdominal aortic aneurysm; Primary aortoduodenal fistula; Surgery
Introduction
Aortoenteric fistulas are infrequent malignant complications of abdominal aortic aneurysms.
The first case report of PADF (primary aorto duodenal fistula), was described by Salmon in 1843.Since then approximately 250 new cases have been reported in the literature [1].
We present a rare case of a primary aorto-duodenal fistula (PADF) associated with abdominal aortic aneurysm (AAA), reveald by an upper digestive hemorrhage
Case Report
A female patient, aged 39 years, was admitted as an Emergency; she had sudden epigastric pain while eating her meal six days previously. The pain radiated through to the back and persisted throughout the night.
The following day she vomited a small clot of Blood.
On the morning of admission, she passed a bulky black Stool. her hemoglobin (Hgb) was 8 g/dL.
the Esophagogastroduodenoscopy (EGd) showed clotted blood in the stomach and proximal duodenum with unsuccessful clots removal. Scannographic appearance in favour of inflammatory aortitis complicated by two partially thrombosed false aneurysms of the subrenal abdominal aorta, located respectively at the level of the emergence of the right renal artery for the first and 18 mm from it for the second; fistulized with the lumen of the 3rd portion of the duodenum.
The patient was admitted to operating room; under general anesthesia, we perform a median laparotomy.
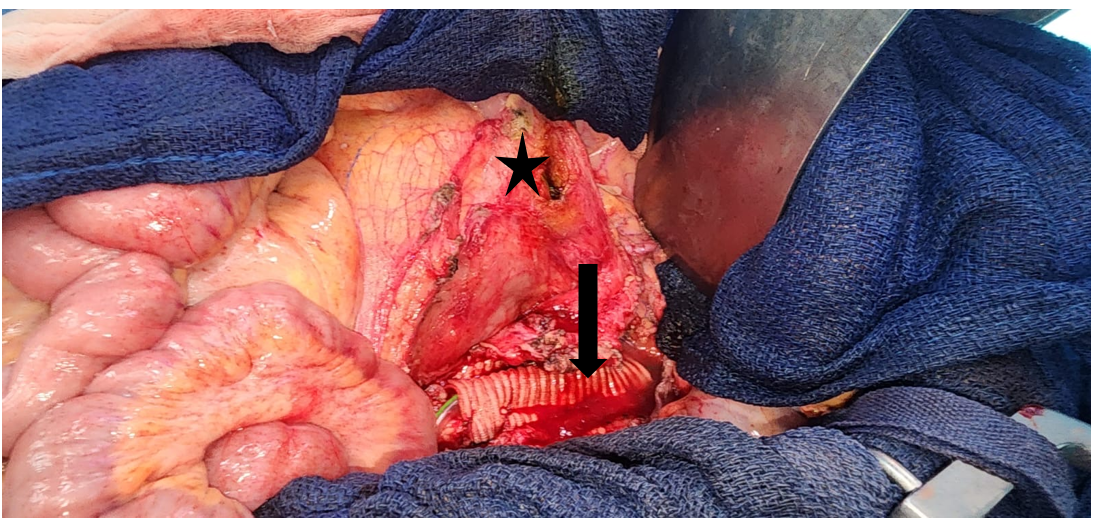
surgical exploration found two thrombosed false aneurysms, the first of which is fistulized with the third duodenal portion.
The procedure involved resection of the aorta on both sides of the aneurysm, with insertion of a reinforced PTFE prosthesis and suture of the duodenal breach.
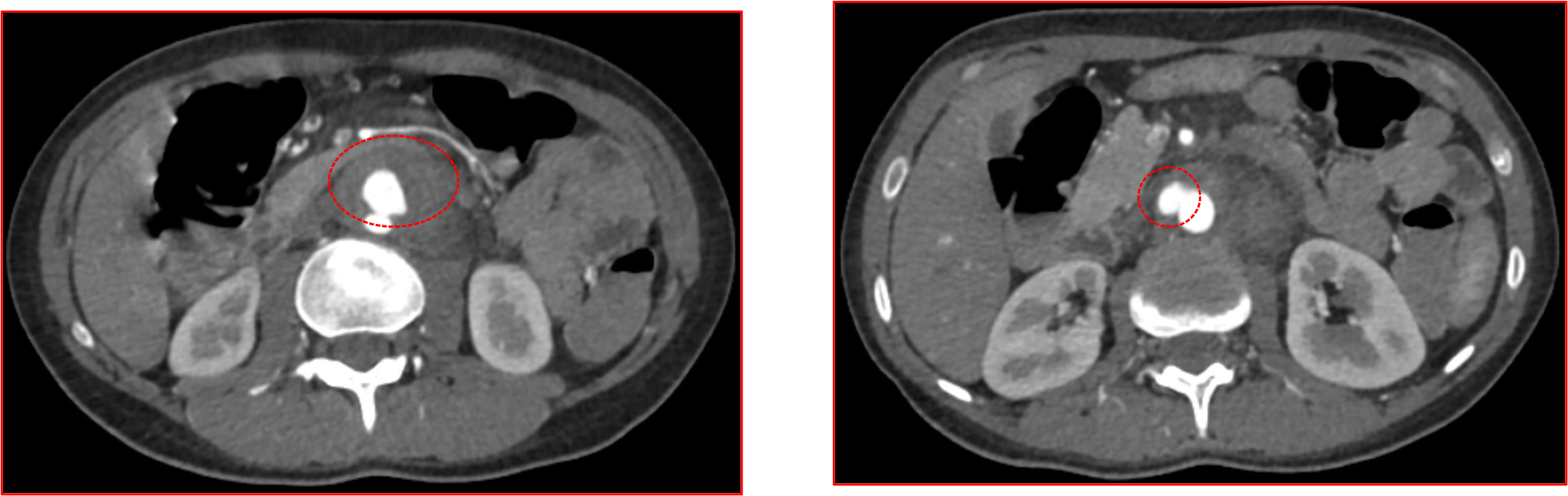
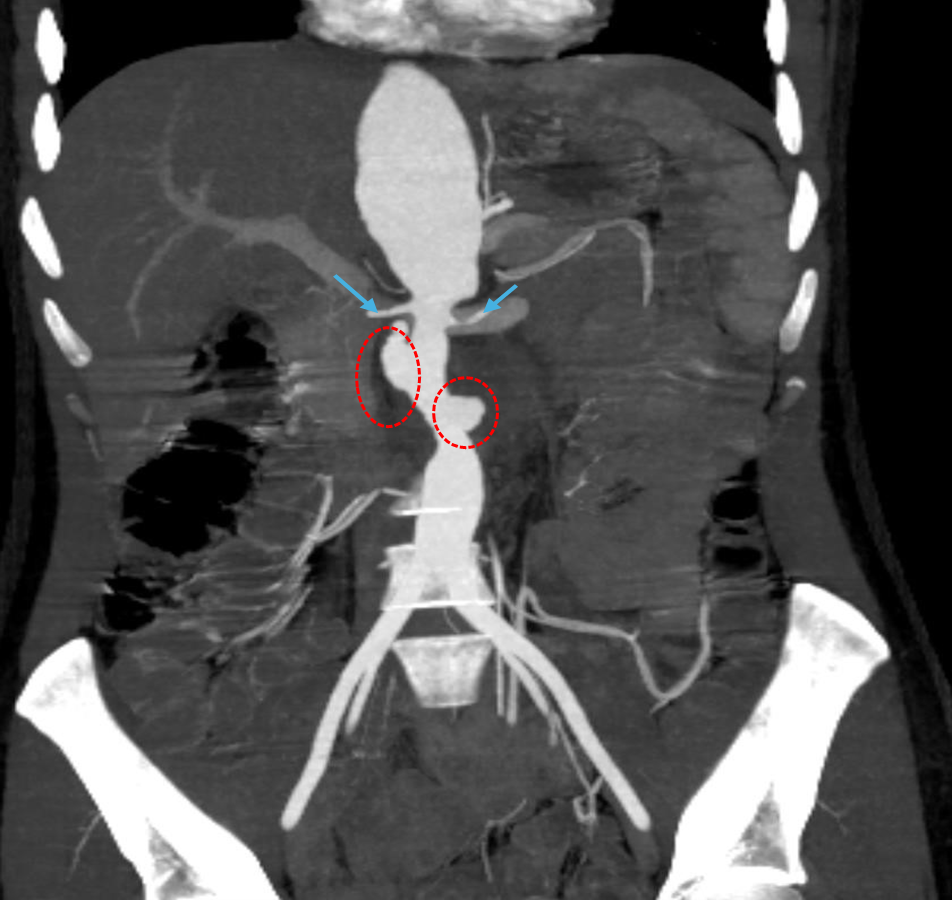
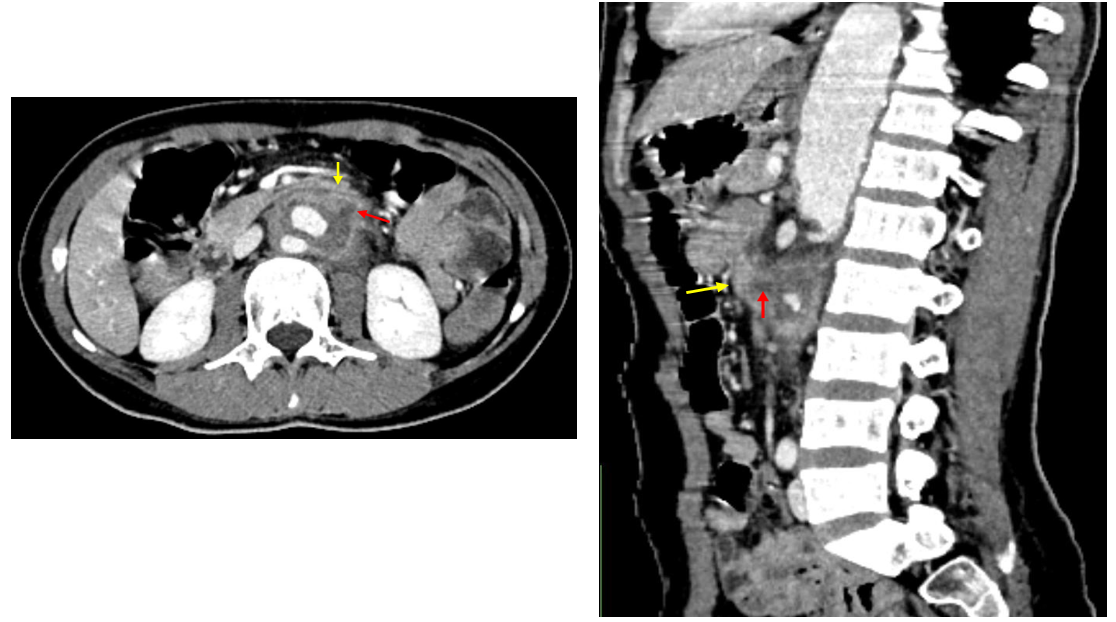
Figure 3: fistula (red arrow) and duodenum (yellow arrow).
Discussion
A primary aorto-enteric fistula is a communication between the native aorta and an adjacent intestinal segment in a patient who has never undergone surgery or suffered prior trauma. It is usually a complication developing from an atheromatous aneurysm of the abdominal aorta. Much more rarely, it may be related to an infectious (‘mycotic’ [2]) aneurysm, vasculitis, tuberculosis or lastly, and historically, syphilitic aortitis [3-6].
The clinical manifestation of PAEF is characterized by GI bleeding followed by massive hemorrhage [7]
CTA of the aorta has 40-90% sensitivity and 33-100% specificity in detecting AEF [8].
The fact that the endoscopic detection rate for PADF is only 25% makes it particularly useful for ruling out other causes of upper GI bleeding [9,10]. This low detection rate may be due to EGD's limited visualization of the distal third of the duodenum.
Treatment of PAEF includes reconstruction of the aorta and repair of the duodenum with an exploratory laparotomy [11]. Endovascular Aortic Repair (EVAR) can be used as a bridge approach in hemodynamically unstable patients [12]. The mortality rate in untreated cases is around 80-100%, while ranges from 30% to 56% in treated cases [13-15].
Conclusion
The diagnosis of aortoenteric fistulas is difficult because of its nonspecific and subtle clinical presentation. In cases where the main vascular vessels and the upper gastrointestinal tract are lesioned the simplest possible reconstructions come of use.
References
- Sokol Xhepa, Ervin Bejko, et al. A very Rare Complication of an Abdominal Aortic Aneurysm. Primary Aortoduodenal Fistula without Gastrointestinal Bleeding. Albanian Journal of Trauma and Emergency Surgery, 2020; 4(1).
- Raymond A, Fairise A, Ropion-Michaux H, Mathias J, Laurent V, Régent D. Imagerie des anévrismes infectieux (mycotiques) de l’aorte Feuillets de radiologie, 2011; 51: pp. 245-253.
- Thomson VS, Gopinath KG, Joseph E, Joseph G. Primary aorto-enteric fistula: a rare complication of abdominal aortic aneurysm J Postgrad Med, 2009; 55(4): pp. 267-269.
- Song Y, Liu Q, Shen H, Jia X, Zhang H, Qiao L. Diagnosis and management of primary aortœnteric fistulas-experience learned from eighteen patients. Surgery, 2008; 143(1): pp. 43-50.
- Roche-Nagle G, O’Donnell DH, Brophy DP, Barry MC. Primary aortœnteric fistula. Am J Surg, 2008; 195(4): pp. 506-507.
- Jarboui S, Jarraya H, Mahjoub W, Baccar M, Kacem C, Abdesselem MM, et al. Primary aorto-enteric fistula in a 52-year-old man. Tunis Med, 2008; 86(9): pp. 830-832.
- Lin TC, Tsai CL, Chang YT, Hu SY. Primary aortoduodenal fistula associated with abdominal aortic aneurysm with presentation of gastrointestinal bleeding: a case report. BMC Cardiovasc Disord, 2018; 18. doi: 10.1186/s12872-018-0852-y.
- dos Santos CR, Casaca R, de Almeida JC, Mendes-Pedro L. Enteric repair in aortoduodenal fistulas: a forgotten but often lethal player. Ann Vasc Surg, 2014; 28: 756-762. doi: 10.1016/j.avsg.2013.09.004.
- Song Y, Liu Q, Shen H, Jia X, Zhang H, Qiao L. Diagnosis and management of primary aortoenteric fistulas-- experience learned from eighteen patients. Surgery, 2008; 143: 43-50. 10.1016/j.surg.2007.06.036.
- Bissacco D, Freni L, Attisani L, Barbetta I, Dallatana R, Settembrini P. Unusual clinical presentation of primary aortoduodenal fistula. Gastroenterol Rep (Oxf), 2015; 3: 170-174. doi: 10.1093/gastro/gou040.
- Ishimine T, Tengan T, Yasumoto H, et al. Primary aortoduodenal fistula: a case report and review of literature. Int J Surg Case Rep, 2018; 50: 80-83. doi: 10.1016/j.ijscr.2018.07.019.
- Sarac M, Marjanovic I, Bezmarevic M, Zoranovic U, Petrovic S, Mihajlovic M. An aortoduodenal fistula as a complication of immunoglobulin G4-related disease. World J Gastroenterol, 2012; 18: 6164-6167. doi: 10.3748/wjg.v18.i42.6164.
- Šumskienė J, Šveikauskaitė E, Kondrackienė J, Kupčinskas L. Aorto-duodenal fistula: a rare but serious complication of gastrointestinal hemorrhage. A case report. Acta Med Litu, 2016; 23: 165-168. doi: 10.6001/actamedica.v23i3.3380.
- Peck JJ, Eidemiller LR. Aortoenteric fistulas. Arch Surg, 1992; 127: 1191-1194. doi: 10.1001/archsurg.1992.01420100049008.
- Fontana M, Tonelli R, Gozzi F, et al. An uncommon cause of hemoptysis: aortobronchial fistula . Multidiscip Respir Med, 2018; 13. doi: 10.1186/s40248-018-0146-3.

