Umbilical Endometriosis: Differential Diagnosis of Incisional Umbilical Hernia
Amine Bachar, Soukaina Khafif, Zakaria Essaidi, Taoufik El Abbassi and Fatima Zahra Bensardi
Departement of General Surgery, Ibn Rochd University Hospital Center, Morocco
Received Date: 13/01/2025; Published Date: 19/03/2025
*Corresponding author: Soukaina Khafif, Departement of General Surgery, Ibn Rochd University Hospital Center, Morocco
Abstract
Endometriosis is an extra-uterine localization of functional endometrial tissue consisting of glands and stroma. The most common site is the internal genitalia, however, there are other locations. Umbilical endometioma represents a differential diagnosis with several pathologies. Treatment is based on surgical removal of the lesion. We report the case of a patient with umbilical endometriosis who was taken for engorged umbilical hernia, because the patient was ashamed to report catamenial bleeding on examination. The diagnosis was evoked during hospitalization, which coincided with her menstrual period. The MRI was also in favor of endometriosis. This was confirmed at anapath after resection of the lesion.
Keywords: Endometriomas; Ombilical endometriosis; Magnetic resonance imaging; Catamenial bleeding
Introduction
Endometriosis is an extra-uterine localization of functional endometrial tissue consisting of glands and stroma [1]. The most common site is the internal genitalia. Other extra-genital locations are less frequent (0.03-0.4%) [2].
Umbilical endometriosis is rare, representing 0.5 to 1% of all extragenital endometrioses [3]. t may be primary or secondary to surgery. Differential diagnoses are essentially primary or incisional umbilical hernia, nodular melanoma, primary or metastatic cancers, granulomas and keloids.
We report the case of a patient with umbilical endometriosis who was treated for engorged umbilical hernia.
Case Report
The patient was 44 years old, had undergone 3 midline caesarean operations, the last one 3 years ago, and had no other particular pathological history. The history of her illness dates back 2 years, with the appearance of an initially painless umbilical tumefaction, appearing cyclically, whose evolution was marked 1 year later by its painful persistence. Clinical examination revealed a median subumbilical laparotomy scar with an umbilical mass that was firm, painless, irreducible and indurated at its base, with no inflammatory signs. The rest of the somatic examination revealed no other abnormalities.

Figure 1: Physical examination showing umbilical mass bleeding during menstrual period.
Abdominal CT suggested an incisional hernia with a spontaneously dense formation at the level of the median scar, with irregular contours probably related to a keloid scar.
Figure 2: CT images suggestive of ombilical hernia.
During her hospitalization, the patient presented bleeding through the umbilicus, coinciding with her menstrual period and that she was ashamed to report. We therefore carried out an abdominal MRI, which revealed a roughly rounded, well-limited formation with regular contours, in discrete T1 and T2 hyposignal, diffusion hypersignal and without ADC diffusion restriction, enhanced after injection of gadolinium. There are also a few T1 hypersignal spots, measuring 34 x 22 mm and extending over 31 mm. A second lesion of the same characteristics was found subumbilically in the subcutaneous fat on the median scar lateralized to the right. Measuring 38 x 31 mm and extending over 39 mm, raising the possibility of parietal endometriosis.
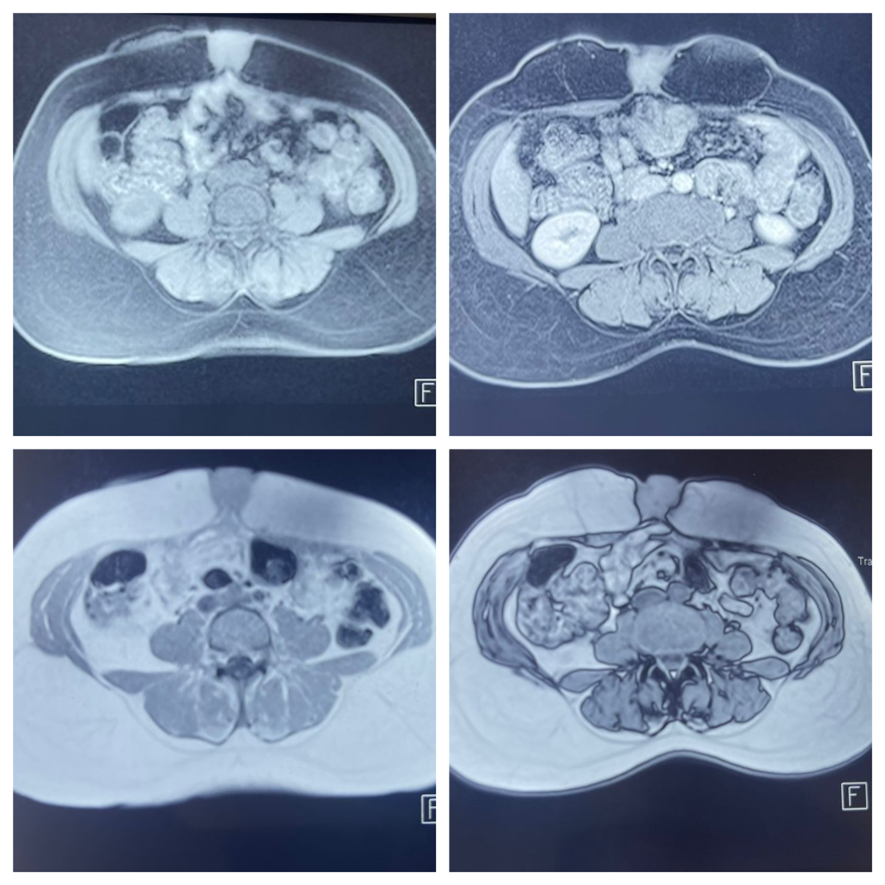
Figure 3: MRI images showing the lesion evoking umbilical endometrioma.
Surgical exploration revealed a 4 cm umbilical mass with no parietal defect, a second 3 cm subcutaneous mass and a 1 cm nodule in the anterior parietal peritoneum. All three masses were resected. The abdominal wall was then closed in anatomical planes. Pathology confirmed endometriosis in all three masses.
Discussion
Endometriosis is the ectopic implantation of functional endometrial epithelium outside the uterine cavity [4]. It is most often found in the pelvis (ovaries, fallopian tubes, broad ligaments, recto-vaginal septum, round and bladder ligaments), extra-pelvic, notably abdominal (appendicular, ureteral, etc.) or extra-abomino-pelvic (cardiac, pulmonary, pleural, diaphragmatic, cerebral, parietal). Of these, parietal endometriosis is the most common1. Endometriosis is parietal when the ectopic location is superficial to the peritoneum5. It may be superficial (subcutaneous tissue), intermediate (attached to the fascia) or deep (in the parietal muscle). Umbilical endometriosis is one of the most common parietal endometrioses.
Several theories have been put forward to explain this ectopic implantation, including reflux migration via the tubes, lympho-vascular migration theory and cellular metaplasia [5,6].
It is a chronic pathology that mainly affects women of childbearing age, with a peak around the age of 40. Diagnosis is often made later than the onset of symptoms, due to a lack of awareness of the pathology [3,4].
Umbilical endometriosis essentially manifests as a painful mass with a catamenial character. The cyclical nature of the pain is an important element of orientation, but its absence does not eliminate the diagnosis. It may be absent in 13% of cases [7]. Clinical signs may appear in the weeks or even years following surgery [4]. In our patient, the interval between the operation and the onset of symptoms was 12 months. The nodule may be located higher than the scar, which may be offset from the deep scar [1]. The classic presentation includes the triad of cyclical abdominal pain at the time of menstruation, a palpable mass and a history of caesarean section or other gynaecological surgery [7].
Ultrasound and CT images of scar endometriosis are not very specific. They may appear as fluid collections or as tissue. In fact, the appearance of lesions depends on hormonal impregnation, depending on the cycle. They may be solid, cystic or mixed [4,8].
MRI is the examination of choice in the search for deep endometriotic lesions indicating medical treatment associated with excision surgery [4]. It provides a better definition of the size of the mass, its relationship with neighbouring structures, particularly the deep plane, and infiltration into surrounding tissues, useful information for choosing the best method of closure of the fascial defect during surgery [5,11]. However, signal characteristics and contrast enhancement patterns are not specific, and it is not always possible to determine the true histological nature of soft tissue masses, with a few exceptions [6].
Different imaging modalities (ultrasound, MRI, CT scan) are not specific but are useful for determining the extent of disease and aiding surgical resection planning, particularly for large, recurrent lesions [6].
Once identified, the endometrioma must be completely excised and sent to pathology [9]. Treatment is based primarily on excision of the mass with safety margins of at least 1cm to reduce the risk of recurrence10. Hysterectomy is a last-line treatment suitable for patients who do not wish future fertility and who have not responded to more conservative management [11].
Even though ultrasound-guided fine needle aspiration can provide diagnosis, surgical excision is recommended for both diagnosis and treatment of an abdominal wall mass [12].
Finally, it should be noted that endometriosis has been shown to undergo a rare malignant transformation in 0.7-1.5% of all cases of endometrioma. It is therefore important to be proactive in the treatment of symptomatic endometriosis, particularly in atypical locations such as those adjacent to the abdominal wall. Some studies report that malignant transformations have a significant mortality rate, of up to 43% in the absence of treatment [11].
References
- Elhabachi B, Brix M. Endométriose pariétale: L’IRM est-elle suffisante pour opérer? PAMJ Clin Med, 2020; 4. doi: 10.11604/pamj-cm.2020.4.2.24198.
- Fahssi ME, Lomdo M, Bounaim A, Ali AA, Sair K. L’endométriose pariétale cicatricielle après césarienne: une entité rare. Pan Afr Med J, 2016; 24(79). doi: 10.11604/pamj.2016.24.79.8680.
- Massaoudi C, Gara S, Chabchoub I, Jones M, Noureddine L, Faten Z. Nodule ombilical avec saignement cyclique : pensez à l’endométriose ombilicale, à propos de 3 cas. Rev Médecine Interne, 2023; 44: A525. doi: 10.1016/j.revmed.2023.10.294.
- Hedfi M, Essid N, Trabelsi F, Znaidi H. Endométriose de la paroi abdominale: à propos de deux cas. Pan Afr Med J, 2022; 42: 54. doi: 10.11604/pamj.2022.42.54.32449.
- Horton JD, Dezee KJ, Ahnfeldt EP, Wagner M. Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg, 2008; 196(2): 207-212. doi: 10.1016/j.amjsurg.2007.07.035.
- Grigore M, Socolov D, Pavaleanu I, Scripcariu I, Grigore AM, Micu R. Abdominal wall endometriosis: an update in clinical, imagistic features, and management options. Med Ultrason, 2017; 19(4): 430-437. doi: 10.11152/mu-1248.
- Ramos-Mayo AE, Gil-Galindo G. Experiencia del departamento de hernias y pared en el manejo de endometriosis de pared abdominal durante 9 años. Cir Cir, 2019; 87(4): 1859. doi: 10.24875/CIRU.19000622.
- Paramythiotis D, Karlafti E, Tsomidis I, et al. Abdominal wall endometriosis: a case report. Pan Afr Med J, 2022; 41: 193. doi: 10.11604/pamj.2022.41.193.33536.
- Payton JI, Chiodo MV, Webster N. Incidental Abdominal Wall Endometriosis in Plastic Surgery: Two Cases and Review of the Literature. Plast Reconstr Surg Glob Open, 2024; 12(6): e5871. doi: 10.1097/GOX.0000000000005871.
- Sow O, Valentin W, Cheikh D, et al. Endométriome ombilical: à propos d’un cas et revue de la littérature: Umbilical endometrioma: a case report and literature review. Pan Afr Med J, 2018; 29: 22. doi: 10.11604/pamj.2018.29.22.14520.
- Zhang N, Robrahn S, Thornburgh KR, et al. Abdominal Wall Endometriosis: A Case Report and Literature Review of Pfannenstiel Incision Endometrioma. Cureus, 2024. doi: 10.7759/cureus.66223.
- Symptomatic Primary Umbilical Endometriosis: A Case Report and A Review of the Literature – International Journal of Health & Medical Research, 2024.

