Spiegel Hernia - A Case Report and Literature Review
Abdelhak Ettaoussi, Kamal Benzidane*, Nassima Fakhiri, Khalid El Hattabi, Abdellillah El Bakouri, Mounir Bouali, Kamal khadija and Majd abdessamad
Hassan II University of Casablanca, Morocco Institution: Department of Visceral Surgical Emergency, Ibn Rochd University Hospital, Casablanca, Morocco
Received Date: 08/02/2025; Published Date: 17/03/2025
*Corresponding author: Kamal Benzidane, Hassan II University of Casablanca, Morocco, Institution: Department of Visceral Surgical, Ibn Rochd University Hospital, Casablanca, Morocco
Abstract
Spigelian hernias (SgH) are a rare type of ventral hernia, accounting for 1–2% of all ventral hernias. They are located along the semilunar line, most commonly within the Spigelian belt. Although rare, the incidence of SgH is increasing due to advancements in modern imaging techniques. These hernias can occur at any age, with a female predominance, often attributed to risk factors such as pregnancy. Clinical diagnosis is challenging because, leading to subtle symptoms such as pain and a swelling sensation despite normal clinical examinations. Imaging techniques, particularly ultrasonography (US) and computed tomography (CT), play a critical role in diagnosis in difficult cases. Surgical treatment can be performed via laparotomy or laparoscopy, with no definitive preference in recent guidelines. A mesh repair is typically recommended and direct suture repair is an option for smaller defects, with both techniques showing low recurrence rates. Laparoscopic techniques such as IPOM, TEP, and TAPP are employed, with the choice depending on the surgeon’s experience. Complications are rare and comparable to those of other abdominal wall hernias, with laparoscopic approaches associated with particularly low complication rates.
Keywords: Spigelian hernia; Abdominal wall hernia; Laparoscopic repair; Mesh repair
Introduction
The Spigelian hernia is a protrusion of intra-abdominal viscera through the anterolateral abdominal wall, specifically at the level of the semilunar line, located between the sheath of the wide abdominal muscles and the lateral edge of the rectus muscle. It was first described by Josef Klinkosh and named after the anatomist and physician Adrian van den Spieghel, who identified this line, *linea semilunaris spigelii* [1,2]. It is a rare type of hernia, accounting for 1–2% of all abdominal wall hernias. Its rarity and location make significant diagnostic challenges as well as therapeutic difficulties.
We present the case of a spiglian hernia in a years old female and discuss its epidemiological features, diagnostic approach and therapeutic management in the light of the existing literature.
Patient and Observation
A 53-year-old female patient, who delivered three children via vaginal delivery and has no significant medical history, presented with a painless, reducible, and cough-impulsive swelling in the left flank for one month, with no associated symptoms. Clinical examination revealed a patient in good general condition. Abdominal examination showed a Spigelian hernia (along the left semilunar line), which was painless, reducible, and cough-impulsive, with no signs of local inflammation. The hernia defect measured 3 cm. The remainder of the somatic examination was unremarkable.
The patient underwent an abdominal wall CT scan, which confirmed a left Spigelian hernia containing small bowel loops and omentum, with no signs of complications. The hernia defect measured 33 mm.
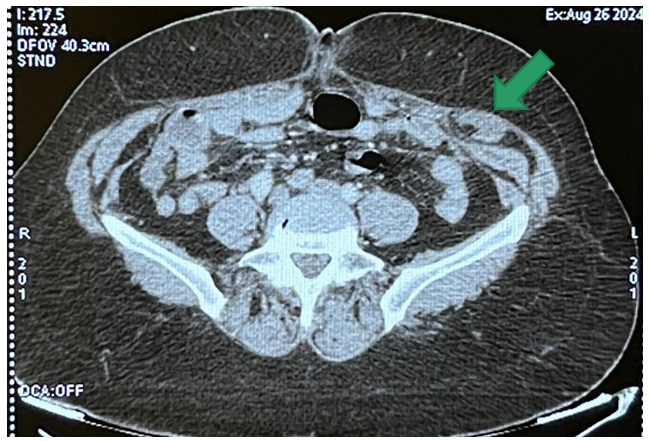
Figure 1: CT scan image showing a left Spigelian hernia with small bowel and epiploic continent.
Laparoscopic approach was performed to treat the condition. Pneumoperitoneum was created using a Veress needle inserted into the left hypochondrium. A 12 mm trocar was placed for the laparoscope in the right flank, followed by two 5 mm trocars: one in the right iliac fossa and the other in the right hypochondrium. Intraoperative exploration confirmed the presence of a left Spigelian hernia with properitoneal fat contents and a 3 cm defect.
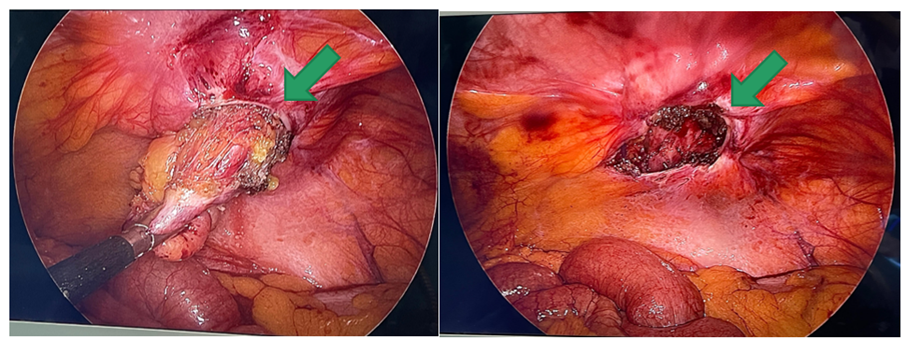
Figure 2: Per operative image showing the left Spigelian hernia containing properitoneal fat (left image) and the 2 cm defect after dissection (right image).
The hernia was repaired using a dual-sided mesh measuring 15 x 15 cm, without closing the hernia defect, and fixing it by using absorbable tackers.
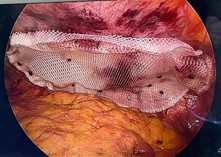
Figure 3: Per operative image of the dual-sided mesh placement.
Postoperative recovery was uneventful, and the patient was discharged the following day.
Discussion
Spigelian hernias (SgH) have several characteristics. Their location is situated at the semilunar line that represents the border between the aponeurosis and the transverse abdominal muscle. The most common localisation is in the Spigelian belt, a wide band situated 6 cm superior to the interspinous [3]. The second characteristic is the incidence of this type of hernia, accounting 1 - 2% of all ventral hernias, but is significantly increasing due to advancements in modern imaging techniques. SgH can occur at any age, with a peak incidence between 40 and 70 years and a female predominance, which can be explained by risk factors, particularly pregnancy [4,5].
The clinical diagnosis remains difficult due to severe points. The hernia sac tends to spread laterally to the interstitial zone between internal and external oblique muscles without penetrating the intact External oblique aponeurosis making two-thirds of the patients describe clinical symptoms of pain, and swelling sensation in the lower abdomen with a normal clinical examination [6,7]. The “Low Spigelian hernia”, a subtype of SpH located caudally to the inferior epigastric artery Low SpH can be mistaken with inguinal hernia or co-existe a direct inguinal hernia most likely due to concomitant wall weakness [3,8,9]. The complicated form seem to be higher compered to others abdominal wall hernia occuring on 17 - 24% of all SgH cases and can be explained by the small defect rarely exceeding 2 cm [3,6,8].
Imagering techniques such as ultrasonography (US) and CT scan made the diagnosis in asymptomatic or difficult case. US is considered the most effective, accessible, and reliable diagnostic tool for identifying Spigelian hernias, with a diagnostic accuracy rate of 86% except in cases of reducible hernias, where it can show an echogenic area in the region of the semilunar line corresponding to the fascial defect. In this case the CT scan can be used as an alternative offering a sensitivity nearing the 100% [10,11,12].
Surgical approach for SgH can be performed via laparotomy or laparoscopy, with no specific preference indicated on the recent EHS guidelines [13]. A mesh repair is recommended, with a 5 cm overlap of the hernia defect. However, Whether the defect should be closed before placing the mesh remains a topic of debated. For small defects, direct suture repair is an option, and both techniques show very low recurrence rate [14-16]. the laparoscopic approach includes different techniques, such as IPOM (IntraPeritoneal Onlay Mesh), TEP (Totally ExtraPeritoneal) and TAPP (TransAbdominal PrePeritoneal). The choice of technique depends on the surgeon's preference and experience [16]. On the other hand, the laparotomy approach may be preferred for large SgH or when a loco-regional anesthesia is required [4,8].
The complication remaing similar to those observed with others hernia with a low rate for the laparoscopic approach [15,17].
Conclusion
Spigelian hernias (SgH) are a rare type of ventral hernia with unique characteristics, including their specific anatomical location along the semilunar line. While advancements in imaging techniques, such as ultrasonography and CT scans, have significantly improved diagnostic accuracy, clinical diagnosis remains challenging due to the hernia's subtle and atypical presentation. The surgical management of SgH, whether through laparotomy or laparoscopy, has demonstrated excellent outcomes with low recurrence and complication rates. The choice of surgical technique and repair method, including mesh placement or direct suturing, largely depends on the hernia's size, complexity, and the surgeon's expertise. Continued advancements in diagnostic tools and surgical approaches are essential to further improving outcomes for this challenging and increasingly recognized condition.
Conflicts of interest: The authors declare no conflict of interest.
Consent for publication: All patients consented to the publication of the presented results.
Author contributions: All authors have contributed to the conduct of this work. All authors also declare that they have read and approved the final version of the manuscript.
References
- van den Spiegel A. De humani corporis fabrica libri decem, 1624.
- Evangelista Deuchinus, Venice Klinkosh JT. Divisionem herniarum novamgue hernias ventralis specimen proponit. Dissertationum Medicorum, 1764; p 184.
- Spangen L. Spigelian hernia. World J Surg, 1989; 13: 573–580. https://doi.org/10.1007/BF01658873.
- Malazgirt Z, Topgul K, Sokmen S, et al. Spigelian hernias: a prospective analysis of baseline parameters and surgical outcome of 34 consecutive patients. Hernia, 2006. https://doi.org/10.1007/s10029-006-0103-5.
- Patle NM, Tantia O, Sasmal PK, et al. Laparoscopic repair of spigelian hernia: our experience. J Laparoendosc Adv Surg Tech. https://doi.org/10.1089/lap.2009.0314
- Larson DW, Farley DR (2002) Spigelian hernias: Repair and outcome for 81 patients. World J Surg, 2010; 26(10): 1277–1281. https://doi.org/10.1007/s00268-002-6605-0.
- Barnes TG, McWhinnie DL. Laparoscopic spigelian hernia repair: a systematic review. Surg Laparosc Endosc Percutan Tech, 2016; 26: 265–270. https://doi.org/10.1097/SLE.0000000000000286.
- Webber V, Low C, Skipworth RJE, et al. Contemporary thoughts on the management of Spigelian hernia. Hernia, 2017. https://doi.org/10.1007/s10029-017-1579-x.
- S Tran H, Tran K, Zajkowska M, et al. Single-incision laparoscopic repair of spigelian hernia. JSLS J Soc Laparoendosc Surg, 2015; 19(e2015): 001644. https://doi.org/10.4293/JSLS.2015.001644.
- S Salemis NS, Kontoravdis N, Gourgiotis S, Panagiotopoulos N, Gakis C, Dimitrakopoulos G. Colonic obstruction secondary to incarcerated Spigelian hernia in a severely obese patient. Int J Surg Case Rep, 2010; 1: 27–29.
- Cruz A, Lerma R, Sánchez-Ganfornina F, Báez F, Muntané J, Padillo FJ. Incarcerated Spigelian hernia: diagnosis by computed tomography. Rev Esp Enferm Dig, 2012; 104: 612–613.
- Fernández-Moreno MC, Martí-Cuñat E, Pou G, Ortega J. Intraperitoneal Onlay Mesh Technique for Spigelian Hernia in an Outpatient and Short-Stay Surgery Unit: What’s New in Intraperitoneal Meshes? J Laparoendosc Adv Surg Tech A, 2018; 28: 700–704.
- Henriksen NA, Kaufmann R, Simons MP, et al. EHS and AHS guidelines for treatment of primary ventral hernias in rare locations or special circumstances. BJS Open, 2020; 4: 342–353. https://doi.org/10.1002/bjs5.50252.
- Moreno-Egea A, Carrasco L, Girela E, et al. Open vs laparoscopic repair of spigelian hernia: a prospective randomized trial. Arch Surg, 2002. https://doi.org/10.1001/archsurg.137.11.1266.
- Skouras C, Purkayastha S, Jiao L, Tekkis P, Darzi A, Zacharakis E. Laparoscopic management of spigelian hernias. In Surgical Laparoscopy, Endoscopy and Percutaneous Techniques, 2011; 21(2): 76–81. https://doi.org/10.1097/SLE.0b013e31820d66df.
- Moreno-Egea A, Campillo-Soto Á, Morales-Cuenca G. Which should be the gold standard laparoscopic technique for handling Spigelian hernias? Surg Endosc, 2015. https://doi.org/10.1007/s00464-014-3738-9.
- Perrakis A, Velimezis G, Kapogiannatos G, et al. Spigel hernia: a single center experience in a rare hernia entity. Hernia, 2012. https://doi.org/10.1007/s10029-012-0925-2.

