Closed Irreducible Traumatic Dislocation of Third, Fourth and Fifth Metatarsophalangeal Joint: A Case Report and Review of Literature
Devendra Pathrot1,*, Anmol Kshirsagar1, Sunil Manual2, Srinath KM2 and Chidendra M Shettar2
1Assistant Professor, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad, India
2Professor, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad, India
Received Date: 30/01/2025; Published Date: 06/03/2025
*Corresponding author: Devendra Pathrot, MS, DNB (Ortho), Assistant Professor, Department of Orthopaedics, SDM College of Medical Sciences and Hospital, Shri Dharmasthala Manjunatheshwara University, Dharwad, India
Abstract
Traumatic closed dislocation of multiple metatarsophalangeal (MTP) joints of lesser toes are uncommon injuries. These dislocations cause severe pain, deformity and difficulty to wear footwear if left untreated. Early diagnosis and proper treatment help the patient for better functional out-come. The complex anatomy of the MTP joint hinders for closed reduction in most of the cases. We are reporting a case of closed irreducible traumatic dislocation of third, fourth and fifth MTP joint following a road traffic accident. Closed attempt was done under local anesthesia in the casualty but failed to reduce. Open reduction was done through dorsal longitudinal incision and reduction was secured with k-wires. There was a button holing of the metatarsal head in the medial part of the plantar plate and were able to reduce all three dislocations through a single incision, without damaging the extensor tendons and the neurovascular bundle. Surgical outcomes after open reduction, followed by effective immobilization and early rehabilitation results in good functional outcome in all cases with nil or minimal complications.
Keywords: Lesser MTP joint dislocation; Plantar plate; Irreducible MTP joint; Open reduction; Surgical approach
Abbreviations: MTP- Metatarsophalangeal Joint; OR- Open reduction; MVA- Motor vehicle accident; NA- Not available; MT- Metatarsal; K- wire- Kirschner wire
Introduction
Closed traumatic dislocation of multiple MTP joints of lesser toes is a rare injury [1]. The MTP joint is a complex synovial joint with strong plantar plate, capsule, deep transverse metatarsal ligament, long and short flexor tendons and lumbrical muscles [2,3]. They play an important role in flexion and extension of the toes especially during the terminal stance and pre-swing phase of the gait cycle [4]. The dislocation of these joint becomes irreducible due to the button holing of the metatarsal (MT) head in the complex plantar structures [5]. These are the unique injuries sometimes we cannot reduce the dislocation by closed manner. Dislocation in this area will have a chronic pain and deformity for the patient to bear weight or walking, if left untreated [6]. There are only few cases in the literature of irreducible dislocation of multiple MTP joints of lesser toes.
We are reporting a case of closed traumatic dislocation of third, fourth and fifth MTP joint following a road traffic accident. Subsequently discussed relevant anatomical structures to understand the injury’s intricacies, the various approaches to make a good clinical decision.
Case Presentation
A 26-year gentleman male patient presented to the casualty with a history of fall from two-wheeler with pain, swelling, and deformity in the left foot. Clinical examination revealed shortening of lateral three toes and fullness on the dorsum of distal foot. An initial radiograph where taken which showed dorsal dislocation of third, fourth and fifth MTP joint as shown in Figure 1. Closed reduction was tried under regional block, but the reduction was unsuccessful. Patient was taken to the operating theatre under regional anaesthesia for open reduction.
Surgical steps
A 5-cm long dorsal longitudinal incision was taken over medial aspect of 4th MT, skin and subcutaneous dissection was done. The extensor tendons of the third toe were identified and a capsule was incised longitudinally medial the extensor tendons. The tendons were retracted medially. Now we can see distally the base of the proximal phalanx, planter plate at the base and the head of MT is dislocated in the medial part of the plantar plate. A small longitudinal incision was given to the plantar plate to enlarge the buttonhole. The head was delivered with the small bone liver and the joint was reduced later secured with k-wire under fluoroscopic guidance as shown in Figure 2a & 2b. Similarly, the other two dislocation of fourth and fifth MTP joint were reduced through the same incision as shown in Figure 2c & 2d.
Postoperative X- rays were taken, showed good reduction. Sutures were removed at 14th day of surgery. Patient was made to walk with help of walker support with non- weight bearing along with below knee plaster support was given for one month. K-wire were removed after one-month, patient was made to walk with full weight bearing as tolerable to pain and active/passive ankle movements were started. At two-month patient was able to walk full weight without any pain with good ankle movements. Postoperative radiographs and clinical picture are shown in Figure 3. At three-month follow-up patient was able to resume his daily activity wearing a regular footwear without any pain. At one year follow-up patient was able to do all his activities like jogging, running, squatting and sitting cross legged without any difficulties.

Figure 1: Radiographs of foot. (a) Anterior-posterior view, (b) Oblique view, (c) Clinical picture of patient.

Figure 2: Intra-operative picture showing (a) White structure shown by black arrow is plantar plate, (b) Yellow arrow shows the 3rd metatarsal head after reduction, (c) Blue arrow shows 2nd metatarsal head after reduction, (d) After reduction all the MTP joints.
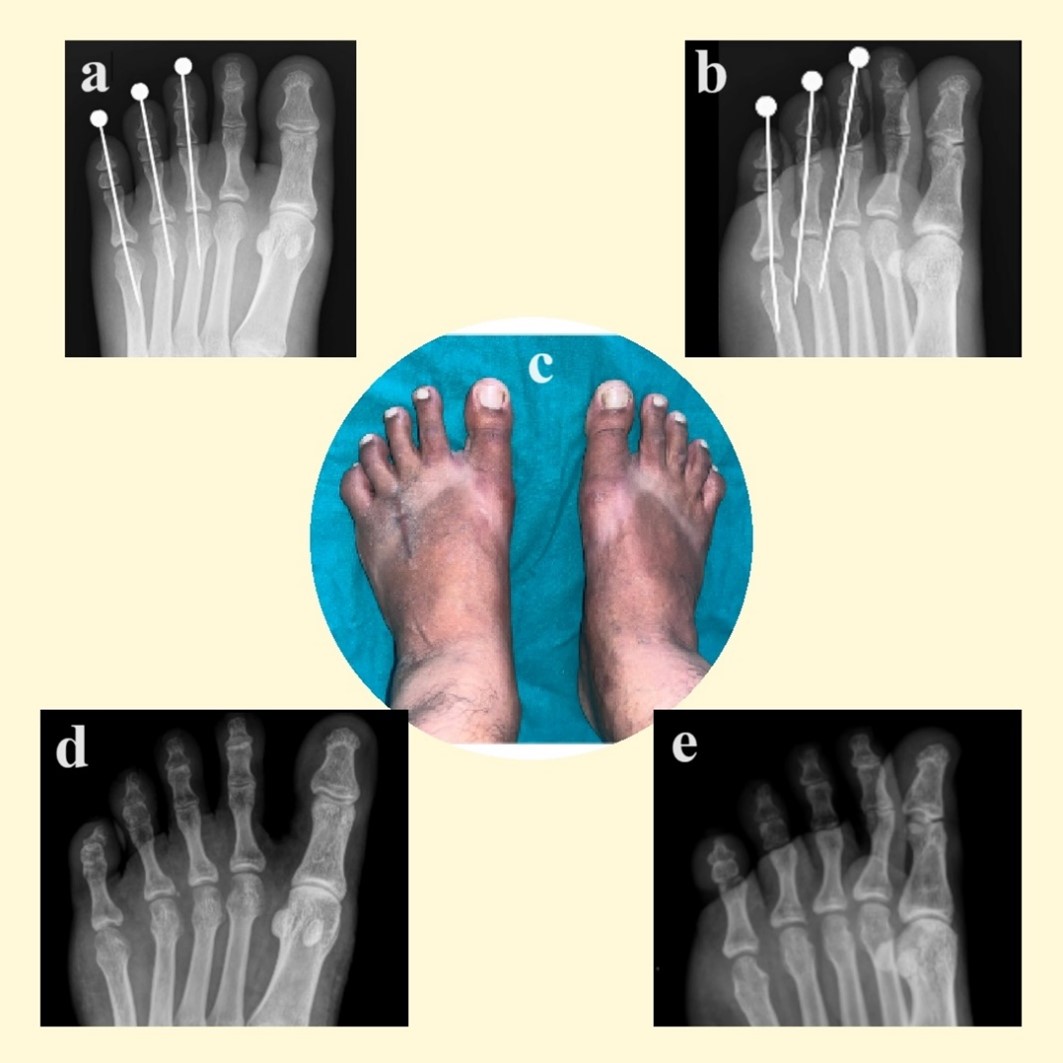
Figure 3: Post-operative radiographs (a) Anterior-posterior, (b) Oblique view, (c) Clinical picture after 1 year follow-up, (d) and (e) Radiographs after 1 year follow-up anterior-posterior and oblique views respectively.
Discussion
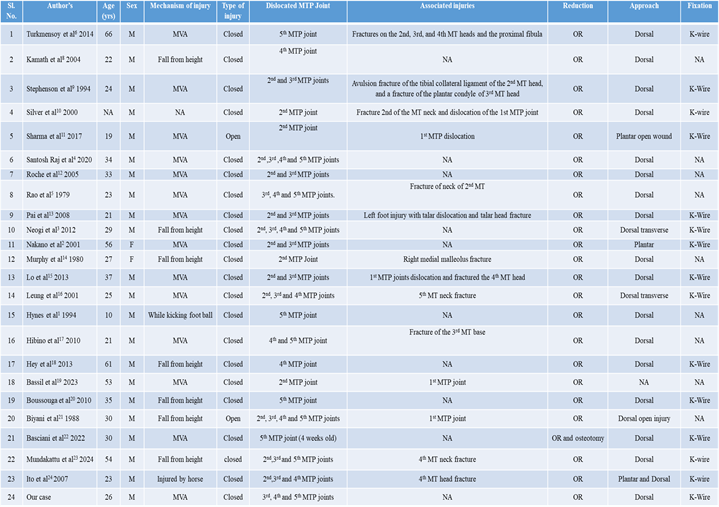
Dorsal dislocation of the MTP joint of lesser toes is a rare but potentially debilitating injury that requires timely and appropriate management. Traumatic dislocations of the first MTP joint are more common compared the lesser toe. Jahss et al in 1980 has classified first MTP joint dislocation on the basis of their anatomy into two types [7]. The lesser MTP joint dislocation can occur isolated signally or two-three MTP joints, or all four of them have been reported. We searched the PubMed, Embase, and Web-of-Science databases and found 21 case reports of lesser toes MTP joint dislocation which were not reducible by closed reduction. The characteristics of all reported cases are listed in the Table 1.
Mechanism of injury
MTP joint dislocation of lesser toe occurs due to fall from height that lands the foot on ground with forceful hyperextension of the MTP joints with foot in equinus position [2,5]. Most common cause for the dislocation is by motor vehicle accident, followed by fall form height. Males are more prone for such injuries than females, and can occur in all age groups.
The MTP joint dislocates dorso-laterally with respect to the MT head. The MT head dislocates towards the plantar surface through the weak medial part of plantar plate and deep transverse metatarsal ligament as shown in Figure 4a. The strong plantar joint capsule consisting of the deep transverse metatarsal ligament, plantar plate, long and short flexor tendons, and lumbrical muscles have been reported to become an obstruction that interferes with the reduction of the dorsal dislocation, independently or in combination with each other [2,12]. The deep transverse metatarsal ligament and plantar plate are strong and caught by the dorsal side of the MT neck, or because the flexor tendons and lumbrical tendons strangulate the MT neck during the closed reduction as shown in Figure 4b.
Johnston et al in 1994, performed an anatomical study using cadavers and reported on the anatomical structure of the MTP joint in lesser toes. The proximal region of the joint capsule ruptures, resulting in dorsal dislocation of the deep transverse metatarsal ligament and the plantar plate. Simultaneously, the flexor tendon strangulates the MT neck laterally and lumbrical tendons medially [25]. In our patient the MT was dislocated medially through the medial part of the plantar plate and the deep transverse metatarsal ligament. The neck of MT head was button holed between deep transverse metatarsal ligament and strong plantar plate (Figure 4b). Irreducible dorsal dislocations of MTP joint of lesser toes requires open reduction and with or without fixation. There are various approaches have been described by different authors for open reduction of lesser MTP joints as shown in Figure 5.
Dorsal approach
Two types of dorsal approaches have been described in the literature dorsal longitudinal and transverse incisions. In our case dorsal longitudinal incision is taken, the skin and subcutaneous tissue is cut and the extensor tendon is retracted medially. The capsule of the MTP joint is incised dorso-medially. After retracting the extensor tendons medially, we can see distally the base of the proximal phalanx, planter plate at the base and the head of MT is dislocated medial to the plantar plate as shown in Figure 6. A small longitudinal incision was given middle to the plantar plate to enlarge the buttonhole. The head is delivered with the small bone liver and the joint is reduced. Hynes et al. reported that the obstacle to reduction was the flexor digitorum longus tendon [1]. Nakano et al. reported that the deep transverse metatarsal ligament interfered with the manipulative reduction [2]. Hibino et al found the fibrocartilaginous plate and lumbrical tendon were the main obstacles to successful closed reduction [17]. Dorsal longitudinal incision is preferred by most of the authors as it requires less retraction and decreases edge necrosis of the wound. However, we require multiple incisions if there are more than two MTP joint dislocations.
Dorsal transverse incision was described by Neogi et al and Leung et al can be used when all the MTP joint are dislocated [3,16]. It includes transverse incision over the MTP joint, the extensor tendons were retracted and joint is open after cutting the capsule. The fibrocartilaginous plantar plate was incised longitudinally to increase the opening and other hindering structures for the reduction of the MT head in position. Advantages of transverse dorsal incision are (a) no need for multiple incisions and (b) decreases problem of wound closure when we need multiple longitudinal incisions. Disadvantages requires too much retraction and increases the risk of edge necrosis of the skin and wound gapping.
Plantar approach
Nakano et al in 2001 described the plantar approach with transverse incision over the MT head.2 In plantar approach, (a) directly approach to the obstruction, (b) the incised deep transverse metatarsal ligament and plantar plate can be sutured, (c) reduction will be stable may not require the k-wire fixation. Disadvantages of plantar approach, (a) wound related complications, (b) requires the identification and protection of the neurovascular bundle.
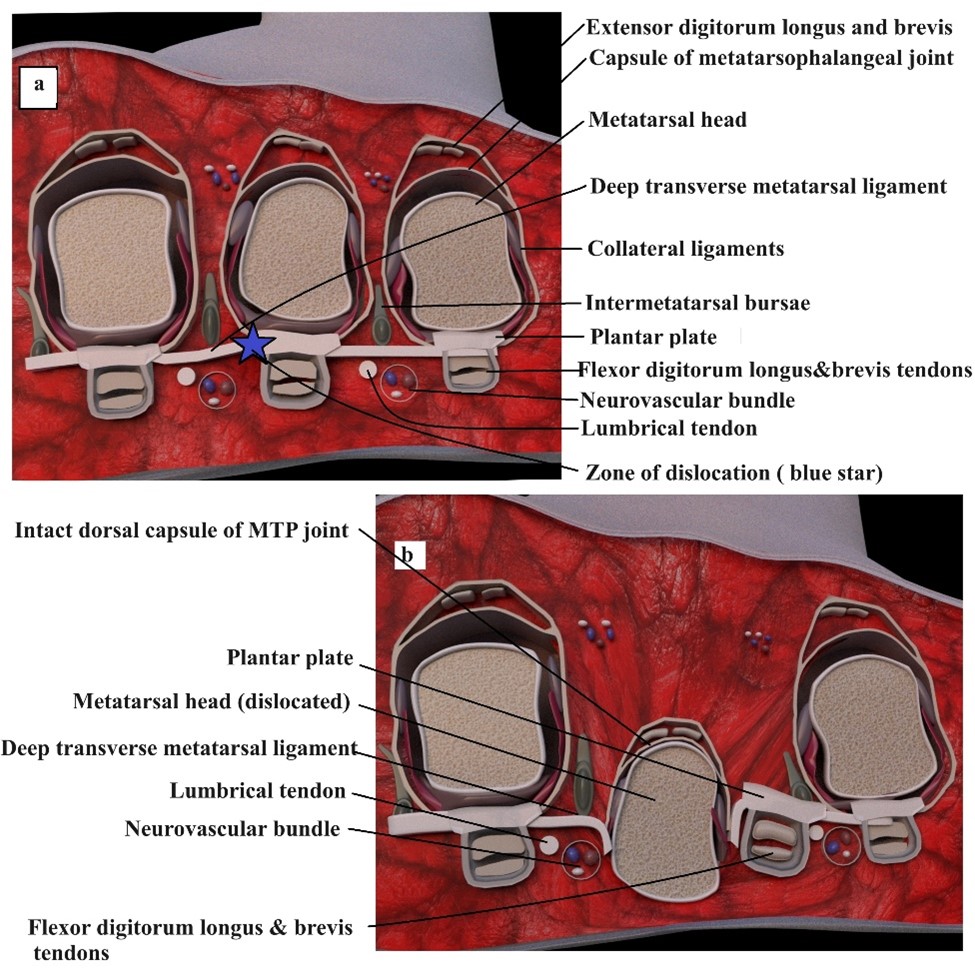
Figure 4: (a) Coronal anatomical section of normal MTP joint showing different structures and Zone of dislocation (blue star), (b) Coronal section after dislocation of MTP joint showing the structures hindering for reduction.
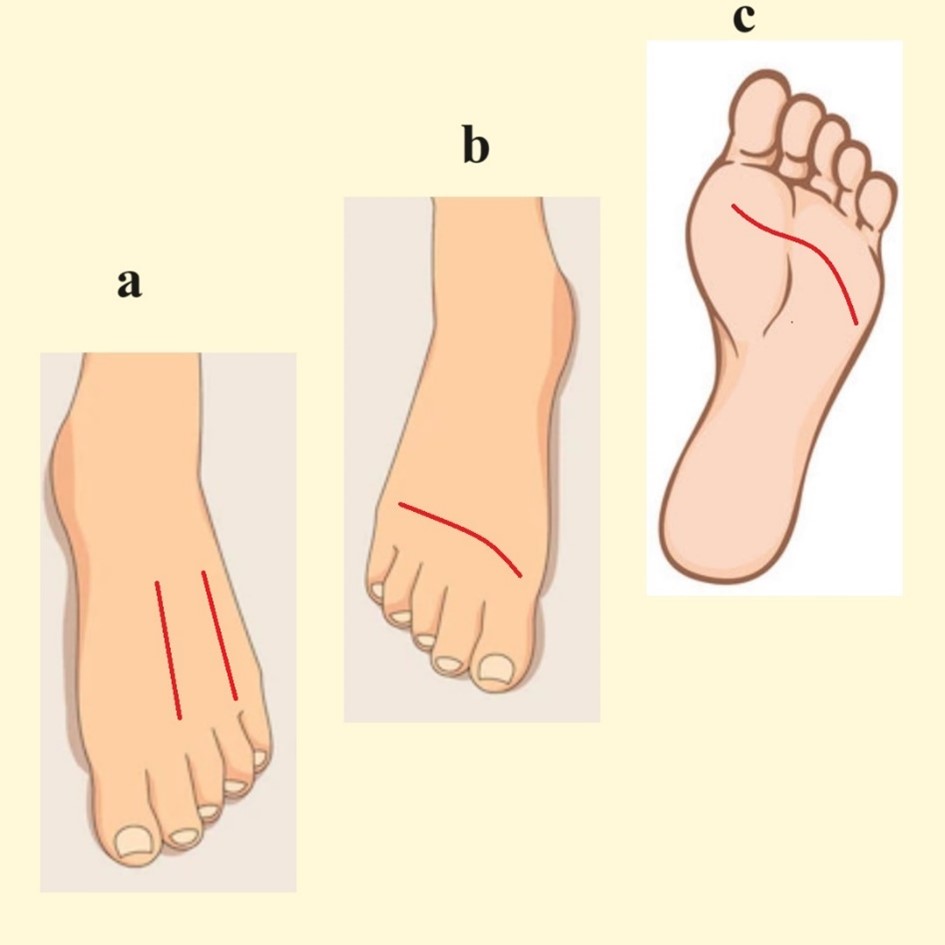
Figure 5: Picture showing various incisions described by different Author’s. (a) Dorsal longitudinal incision, (b) Dorsal transverse incision, (c) Plantar transverse incision.
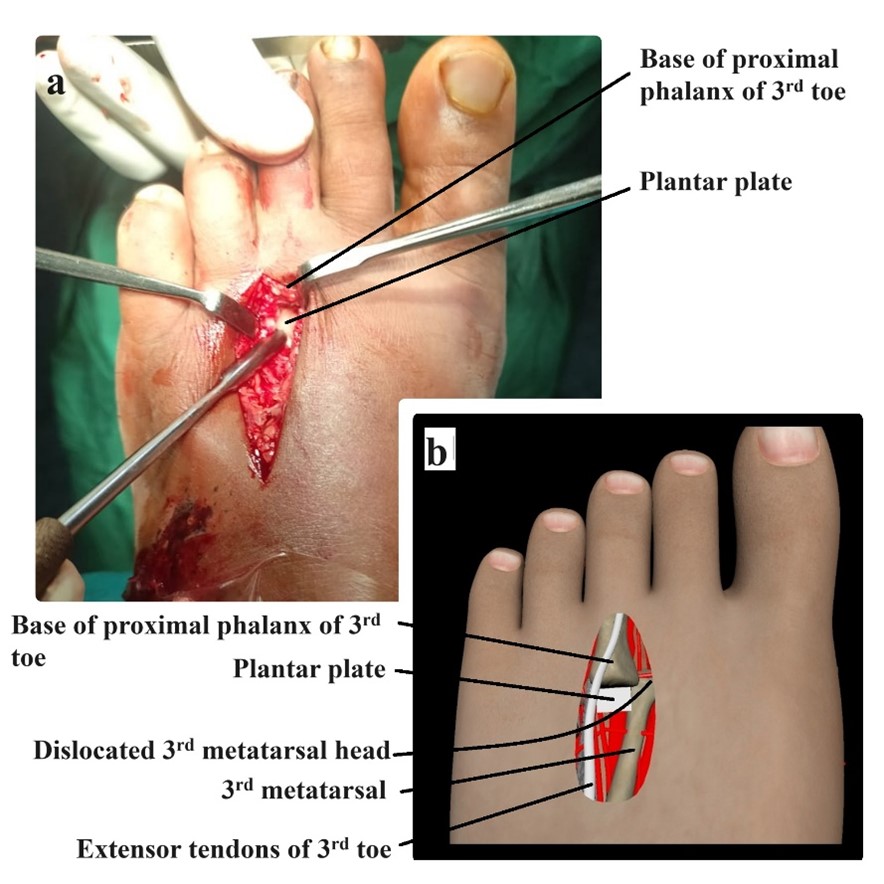
Figure 6: (a) Intraoperative picture showing plantar plate and base of the proximal phalanx of third toe before reduction, (b) Animated picture of the above clinical picture showing different structures and dislocated metatarsal head.
Table 1: Shows the characteristics of various case reports of lesser MTP joint dislocations.
Conclusion
Dorsal dislocation of lesser MTP joint is a rare injury may be associated with fracture of the adjacent metatarsals. Irreducible MTP joint requires open reduction preferably dorsal approach with or without fixation with the k-wire. The surgical repair of the plantar plate is not necessary. Surgical outcomes after open reduction, followed by effective immobilization and early rehabilitation results in good functional outcome in all cases with nil or minimal complications.
Conflict of interest: The authors declare that there is no conflict of interest with respect to authorship and /or publication of this article.
Ethics: Informed written consent was taken from patient to be research participant.
Financial statement: Authors doesn’t have any financial/personal interest.
References
- Hynes D, D’Souza LG, Stephens M. Irreducible dislocation of the fifth metatarsophalangeal joint: a case report. Foot Ankle Int, 1994; 11: 625–626.
- Nakano Y, Mogami A, Kaneko K, Inoue Y. Irreducible dorsal MTP joint dislocation in the second and third toes. Injury, 2003; 34: 870–873.
- Neogi DS, Bandekar SM, Sadekar V, Patnaik S, Bhat T, D’Mello Z. Irreducible dislocation of all the lesser metatarsophalangeal joints of the foot: a case report. Foot Ankle Spec, 2012; 5: 324–326.
- Raj S, Subramani S, Babar SJ, Balaji MS, Anand V. Rare Case Report of Closed Traumatic Dislocation of Second to Fifth Metatarsophalangeal Joints. Case Rep Cureus, 2020; 28: 12(11).
- Rao JP, Banzon MT. Irreducible dislocation of the metatarsophalangeal joints of the foot. Clin Orthop Relat Res, 1979; 145: 224–226.
- Turkmensoy F, Erinc S, Ergin ON, Ozkan K, Kemah B. Irreducible fifth metatarsophalangeal joint after car crush injury. Case Rep Orthop, 2015: 2015: 894057.
- Jahss MH. Traumatic dislocations of the first metatarsophalangeal joint. Foot Ankle, 1980; 1: 15-22.
- Kamath SU, Savur AD, Pramod S. Irreducible traumatic dislocation of the fourth metatarsophalangeal jointda case report. Injury Extra, 2005; 36: 212–213.
- Stephenson KA, Beck TL, Richardson EG. Plantar dislocation of the metatarsophalangeal joint: case report. Foot Ankle Int, 1994; 8: 446–449.
- Silver SA, Mizel MS. Open reduction and internal fixation of the simultaneous lesser metatarsal fracture and MPJ dislocation. Foot Ankle Int, 2000; 21: 52.
- Sharma A, Dosajh R, Bedi GS, Gupta K, Jain A. First and Second Metatarsophalangeal Joint Open Dislocations: A Case Report. Malays Orthop J, 2017; 11(1): 71-73.
- Roche S, Kennedy M, Lenehan B, O’Sullivan M. Irreducible plantar dislocation of the second and third metatarsal heads: a case report. Eur J Orthop Sur & Trauma, 2005; 15: 355-358.
- Pai V, Mitchell R, Pai V. Irreducible Dislocation of the Metatarsophalangeal Joints of the Foot: A Case Report. The Foot & Ankle Journal, 2008; 1(5): 5.
- Murphy JL. Isolated dorsal dislocation of the second metatarsophalangeal joint. Foot Ankle Int, 1980; 1: 30–32.
- Lo H, Liu PC, Shen PC, Chen SK, Cheng YM, Lu CC. Irreducible metatarsophalangeal joint dislocation of the lesser toes: a case report. J Am Podiatr Med Assoc, 2013; 103(3): 236-240.
- Leung WY, Wong SH, Lam JJ, Ip FK, Ko PS. Presentation of a missed injury of a metatarsophalangeal joint dislocation in the lesser toes. J Trauma, 2001; 50: 1150–1152.
- Hibino N, Amari R, Aoki M. Irreducible dislocation of the metatarsophalangeal joints of the fourth and fifth toes: a case report and anatomical study. Foot Ankle Int, 2010; 31: 339.
- Hey HW, Chang G, Hong CC, Kuan WS. Irreducible dislocation of the fourth metatarsophalangeal joint--a case report. Am J Emerg Med, 2013; 31(1): 265.e1-273.
- Bassil GF, Nader F, Lajmi A, Missaoui Z. Dorsal Dislocation of the First and Second Metatarsophalangeal Joint: A Case Report and Literature Review. Cureus, 2023; 15(9): e45407.
- Boussouga M, Boukhriss J, Jaafar A. Irreducible dorsal metatarsophalangeal joint dislocation of the fifth toe: a case report. J Foot Ankle Surg, 2010; 49: 298.
- Biyani A, Sharma JC, Mathur NC. Plantar panmetatarsophalangeal dislocationda hyperflexion injury. J Traum, 1988; 28: 868–869.
- Basciani S, Santini S, Marineo G, Santo PD, Narinozzi A. A Rare Case of Fifth Metatarsophalangeal Joint Subluxation: A Case Report. J Am Podiatr Med Assoc, 2023: 1-13.
- Mundakattu V, Veluthedath R, Pookkayil MR, Mammu S. Open Reduction of 2nd Metatarsophalangeal Joint as a Method to Reduce Combined Lesser Metatarsophalangeal Dislocation - A Case Report. J Orthop Case Rep, 2024; 14(4): 110-114.
- Ito MM, Murase K, Tanaka S, Yamashita T. Dislocation of all metatarsophalangeal joints caused by horse injury. J Trauma, 2007; 63: 938–939.
- Johnston III RB, Smith J, Daniels T. The plantar plate of the lesser toes: an anatomical study in human cadavers. Foot Ankle Int, 1994; 5: 276–282.

