Correlation Between Changes in Peripapillary Capillaries in Primary Open Angle Glaucoma by OCT Angiography and RNFL Thickness Measured by OCT
Marina Estefan1,* and Bassant Abdel El- Hamed Korany2
1Warrington and Halton teaching hospitals, UK
2Beni Suef university, Egypt
Received Date: 30/01/2025; Published Date: 27/02/2025
*Corresponding author: Marina Estefan, Warrington and Halton teaching hospitals, UK
Abstract
Background: Optical Coherence Tomography Angiography (OCTA) is a revolutionary imaging technology that enables the blood flow into the retina and optic nerve head without intravenous injection of dye. The objective of this study was to connect changes between OCT and retinal nerve fiber layer (RNFL) thickness with peripapillary capillaries in primary open-angle glaucoma (POAG) by OCT Angio.
Methods: This sectional cross-pilot study was carried out in 30 patients age between 20 to 60, patients with POAG and to correlate between localized RNFL defect and peripapillary capillary by OCT angiography.
Results: Statistically significant positive correlation between RNFL thickness and vascularity in superior sector, RNFL thickness and vascularity in inferior sector, RNFL thickness and vascularity in nasal sector. significant positive correlation between RNFL thickness measured for nasal, superior and inferior sectors. significant positive correlation between pericapillary changes measured for nasal, superior, temporal and inferior aspect.
Conclusion: The detection of reduced vessel density in POAG perimetrically shows that OCT-A can identify a significant risk of microvascular alterations in the eyes before visual area impairment is detected.
Keywords: Peripapillary capillaries; Primary open angle glaucoma; OCT angiography; RNFL
Introduction
Glaucoma is one of the world's major irreversible blindness [1]. Glaucoma's pathogenesis is complicated and unclear. Mechanically, the damage caused by the retinal ganglion is caused by increasing intraocular pressure (IOP), compared with additional elements like as blood flow in glaucoma aetiology in "vascular" hypothesis [2].
The outcome was comprehensive investigation of microvascular infusion and flow of blood to the head of the optic nerve (ONH). A variety of different diagnostic instruments are utilised in clinical practise to quantify and evaluate the course of OAG. These include the examination of the visual field and the determination of stereometric parameters using Heidelberg retina tomography by employing OCT images to examine the RNFLT thickening (HRT). OCT is extensively used to diagnose and manage retinal disorders and glaucoma, as it provides retinal thickness measurements [3].
A newly designed OCT angiography (OCTA) has proved the capacity to quickly and correctly assess retinal and disc flow [4].
It is a non-invasive technology that requires no exogenous dye or contrast agent and quantities of disc infusion close automatically.
OCTA is a revolutionary imaging technology that enables the blood flow into the retina and optic nerve head without intravenous injection of the Dye in normal and pathological vascularization. The measurement of blood flow is an interesting component of this non-invasive approach. In normal people and in diverse disorders, the reproducibility and repeatability of the flow density data were demonstrated to be high [5].
Further research in patients with glaucoma compared to healthy tests have shown a decrease disc infusion [6].
The objective of this study was to connect changes between OCT and RNFL thickness and peripapillary capillaries of primary open-angle glaucoma by using OCTA.
Patients and Methods
This sectional cross-pilot study in 30 patients aged between 20 to 60, patients with POAG and localized RNFL defect, both males and females with OCT angiography and OCT thickness evaluated in POAG correlating alterations in peripapillary capillaries in primary open angle glaucoma. The study was done at Ophthalmology department clinic at Beni-suef university hospital from 1st July 2020 to 30 of March 2021.
Exclusion criteria were patients with History of ocular or systemic diseases causing ONH damage, thinning of circum papillary retinal nerve fibre layer, visual field defects, patients with refractive error > -6 or > +3D spherical equivalent, media opacities preventing high quality imaging, vitreoretinal disease previous retinal surgery, any other diseases that could potentially cause visual field loss or optic disc abnormalities and angle closure glaucoma or neurological disease.
Cases will be chosen randomly according to inclusion and exclusion criteria.
Statistical Analysis
IBM SPSS® (version 22.0) Software was used to alter, modify and analyse the data. Average, standard deviation, minimum and maximum values have been reported in descriptive statistics for the continuous variables. As frequency and proportion, categorical variables were described. Postoperative differences were shown as a median difference, 95% confidence intervals, and the acceptable margin of Error was set at 5%. The p-value was therefore considered important: The differences were tested for statistical significance using paired t-test. The comparison between groups regarding qualitative data was done by using chi-square test. A two tailed P value <0.05 was considered significant.
Results
Table 1 showed that seventy percent of the studied patients were males and 53.3% of the studied eyes were right sided. Age ranged from 42 to 55 years with mean 47.9 years. IOP ranged from 13.5 to 16.5 mmHg with mean 15.167 mmHg. C/D ratio ranged from 0.1 To 0.8 with mean 0.563. Rim area ranged from 0.43 to 2.1 with mean 1.087. Disc area ranged from 1.2 to 2.83 with mean 1.939.
Table 1: Distribution of the studied patients according to baseline data and IOP and disc measurements.
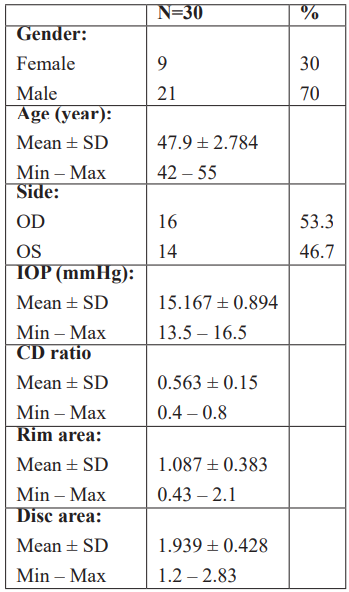
Table 2 shows that Mean RNFL thickness measured by OCT in different direction were measured by RNFL thikness and were found to be (84.47 in superior sector), (83.2 in inferior Sector), (73.8 in nasal sector) and (63.8 in temporal sector). Mean vascularity in different direction were measured by OCTA and were found to be (41.5 in superior sector), (40.47 in inferior sector), (41 in nasal sector) and (45.3 in temporal sector).
Table 2: RNFL thickness of optic disc among the studied patients measured by OCT.
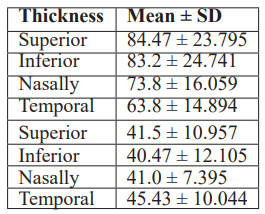
Table 3 shows that there is statistically significant positive correlation between RNFL thickness and vascularity in superior sector, RNFL thickness and vascularity in inferior sector, RNFL thickness and vascularity in nasal sector. there is statistically non-significant between RNFL thickness and vascularity in temporal sector.
Table 3: Correlation between thickness and vascularity of optic disc (superior aspect).
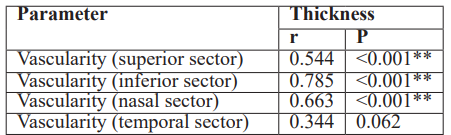
r Pearson correlation coefficient **p≤0.001 is statistically highly significant
Table 4 shows that there is no significant correlation between RNFL thickness (by OCT) at any sector and IOP, vascularity by OCTA at any sector and IOP, between disc measurements and IOP.
Table 4: Correlation between IOP of the studied patients and RNFL thickness measured by OCT, pericapillary changes by OCT angiography and disc measurements.
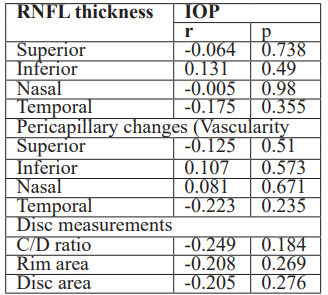
r Pearson correlation coefficient
Table 5 shows that there is statistically significant positive correlation between RNFL thickness (by OCT) measured for nasal, superior and inferior sector. However, there is non-significant correlation between temporal thickness and thickness measured in any other direction.
Table 5: Correlation between RNFL thickness in different direction by OCT.
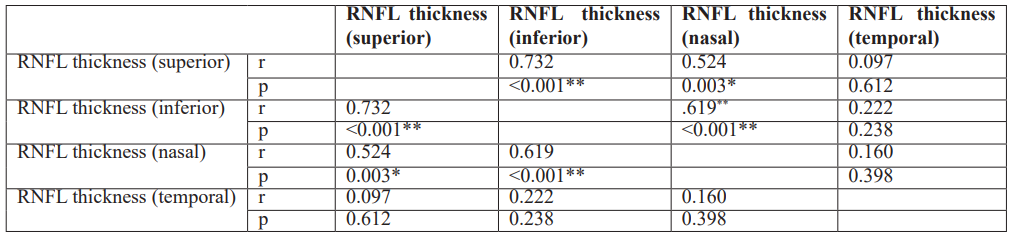
r Pearson correlation coefficient *p<0.05 is statistically significant **p≤0.001 is statistically highly significant.
Table 6 shows that is statistically significant positive correlation between pericapillary changes measured for nasal, superior, temporal and inferior aspect.
Table 6: Correlation between pericapillary changes in different direction by OCT angiography.
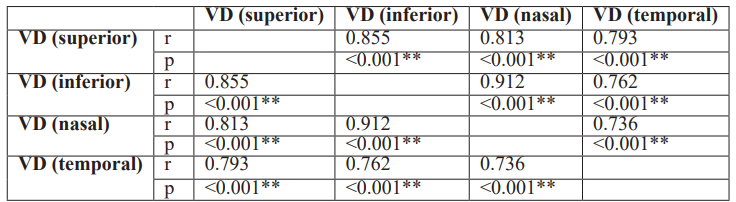
r Pearson correlation coefficient *p<0.05 is statistically significant **p≤0.001 is tatistically highly significant
Discussion
OCTA can provide detailed capillary peripapillary pictures and can generate layered microvascular structure face pictures [7]. In our current study, there is a statistically significant positive correlation in the superior, inferior, and nasal aspects between RNFL thickness (by OCT) and vascularity by OCTA, while a non-significant correlation in the temporal sector between RNFL thickness (by OCT) and vascularity (by OCT angiography) is found. The reduced vascularity in the RNFL area revealed in this study is consistent with prior OCTA investigations, where associations between the retinal vessels' density and the inner retinal layer thickness or the RNFL were identified [8,9].
In the RNFL or the inner retina, capillaries seem to be affected when neuronal tissue degenerates [10,11]. In the ONH neural tissue, same discovery was likewise shown in the eyes with glaucoma. Midgett et al., showed that the capacity loss in both test and real glaucoma eyes was proportionate to the loss of neuronal tissue inside ONH [12,13].
Park et al [9] revealed a favourable link with their respective peripapillary vascular Densities of the temporal and superior and temporal RNFL thicknesses [14].
In the current investigation, however, no important link existed between vascularity in any sector and IOP, elevated IOP as risk factor might affect the RNFL thickness.
Cronemberger et al., 2021 [6]. Contrary to many prior research, the IOP revealed a negative connection in the median inferonasal and infero-temporal fields with the peripapillary vascular density (Park et al., 2019 [9,14].
Wang et al [15] also conducted angiography of OCT in glaucoma patients, showing a strong link between ganglion-cell complex thickness and decrease in the flow index and density of the artery, indicating that blood flow in the optic disc is essential for monitoring. Moreover, a trial with Speckle Distribution OCT angiography found considerable linkage between RPC density and RNFL thickness and visual field index in the healthy persons, patients with glaucoma and those suspected of glaucoma [16]. In people with glaucoma, a link was revealed in several investigations between the findings of OCT angiography, vascular density, and peripapillary blood flow in and around the optic disc.
Our study was hampered by its cross-sectional design, it is unable to determine the difference between the effects of anti-glaucoma medication, depending upon glaucoma medicine and various phases of the POAG.
Conclusion
OCT-A identifies the decline in vessel density in the eyes of POAG patients. The reduced vascular density of the POAG eyes means that quantitative OCT-A measures indicate damage to pathophysiologically important tissues of glaucoma. The detection of reduced vessel density in POAG perimetrically shows that OCT-A can identify a significant risk of microvascular alterations in the eyes before visual area impairment is detected.
Financial support and sponsorship: None
Conflict of Interest: None
References
- Reis AS, Sharpe GP, Yang H, Nicolela MT, Burgoyne CF, Chauhan BC. Optic disc margin anatomy in patients with glaucoma and normal controls with spectral domain optical coherence tomography. Ophthalmology, 2012; 119: 738-747.
- Alward WL. The genetics of open-angle glaucoma: the story of GLC1A and myocilin. Eye (Lond), 2000; 14 (Pt 3B): 429-436.
- Bathija R, Gupta N, Zangwill L, Weinreb RN. Changing definition of glaucoma. J Glaucoma, 1998; 7: 165-169.
- Bowd C, Zangwill LM, Weinreb RN, Girkin CA, Fazio MA, Liebmann JM, et al. Racial Differences in Rate of Change of Spectral-Domain Optical Coherence Tomography-Measured Minimum Rim Width and Retinal Nerve Fiber Layer Thickness. Am J Ophthalmol, 2018; 196: 154-164.
- Chen FK, Viljoen RD, Bukowska DM. Classification of image artefacts in optical coherence tomography angiography of the choroid in macular diseases. Clin Exp Ophthalmol, 2016; 44: 388-399.
- Cronemberger S, Veloso AW, Veiga C, Scarpelli G, Sasso YC, Merola RV. Correlation between retinal nerve fiber layer thickness and IOP variation in glaucoma suspects and patients with primary open-angle glaucoma. Eur J Ophthalmol, 2021; 31: 2424-2431.
- Spaide RF, Klancnik JM, Jr. Cooney MJ. Retinal vascular layers imaged by fluorescein angiography and optical coherence tomography angiography. JAMA Ophthalmol, 2015; 133: 45-50.
- Yarmohammadi A, Zangwill LM, Diniz-Filho A, Saunders LJ, Suh MH, Wu Z, et al. Peripapillary and Macular Vessel Density in Patients with Glaucoma and Single-Hemifield Visual Field Defect. Ophthalmology, 2017; 124: 709-719.
- Park JH, Yoo C, Kim YY. Peripapillary Vessel Density in Young Patients with Open-Angle Glaucoma: Comparison between High-Tension and Normal-Tension Glaucoma. Sci Rep, 2019; 9: 19160.
- Yu PK, Balaratnasingam C, Xu J, Morgan WH, Mammo Z, Han S, et al. Label-Free Density Measurements of Radial Peripapillary Capillaries in the Human Retina. PLoS One, 2015; 10: e0135151.
- Lee EJ, Lee KM, Lee SH, Kim TW. OCT Angiography of the Peripapillary Retina in Primary Open-Angle Glaucoma. Invest Ophthalmol Vis Sci, 2016; 57: 6265-6270.
- Zabel P, Kaluzny JJ, Wilkosc-Debczynska M, Gebska-Toloczko M, Suwala K, Zabel K, et al. Comparison of Retinal Microvasculature in Patients with Alzheimer's Disease and Primary Open-Angle Glaucoma by Optical Coherence Tomography Angiography. Invest Ophthalmol Vis Sci, 2019; 60: 3447-3455.
- Midgett D, Liu B, Ling YTT, Jefferys JL, Quigley HA, Nguyen TD. The Effects of Glaucoma on the Pressure-Induced Strain Response of the Human Lamina Cribrosa. Invest Ophthalmol Vis Sci, 2020; 61: 41.
- Zhang Q, Wang RK, Chen CL, Legarreta AD, Durbin MK, An L, et al. Swept source optical coherence tomography angiography of neovascular macular telangiectasia type 2. Retina, 2015; 35: 2285-2299.
- Wang X, Jiang C, Ko T, Kong X, Yu X, Min W, et al. Correlation between optic disc perfusion and glaucomatous severity in patients with open-angle glaucoma: an optical coherence tomography angiography study. Graefes Arch Clin Exp Ophthalmol, 2015; 253: 1557-1564.
- Igarashi R, Ochiai S, Sakaue Y, Suetake A, Iikawa R, Togano T, et al. Optical coherence tomography angiography of the peripapillary capillaries in primary open-angle and normal-tension glaucoma. PLoS One, 2017; 12: e0184301.

