Brunsting-Perry Cicatricial Pemphigoid of the Scalp
Julian Camilo Sánchez Guerrero*, Karen Vincenzi, Paulina Gabriela Pacheco Buñay, Claudia Procel, Diana Carolina Vasconez Celis, Josselyn Nicole Valarezo Sánchez, Ana Leticia Boff and Renan Minotto
Dermatology Service, Hospital da Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil;
Department of Internal Medicine/Dermatology, Federal University of Health Sciences of Porto Alegre, Porto Alegre, RS, Brazil
Received Date: 17/01/2025; Published Date: 19/02/2025
*Corresponding author: Julian Camilo Sánchez Guerrero, Dermatology Service, Hospital da Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, RS, Brazil; Department of Internal Medicine/Dermatology, Federal University of Health Sciences of Porto Alegre, Porto Alegre, RS, Brazil
Dear Editor,
Cicatricial pemphigoid is a chronic autoimmune disease that affects the mucous membranes and the skin [1].
Brunsting-Perry pemphigoid (BPP) is a variant of cicatricial pemphigoid, with development of limited subepidermal blisters on the head, face, neck and upper trunk, without mucosal involvement [2].
The most striking clinical feature is the development of significant scarring [3].
The pathogenesis of cicatricial pemphigoid is related to autoantibodies against proteins BP180 , BP230 and the anchoring filament component laminin 5 [1].
We are reporting the case of a 74-year-old caucasian female patient presenting with scalp lesions and associated trichodynia. Trichoscopy revealed bullous lesions, erosions, punctiform and comma-shaped vessels, scaly crusts, and erythematous-whitish scar-like plaques located in the crown region, with significant loss of hair coverage. The histopathological findings were consistent with the diagnosis of scalp cicatricial pemphigoid (SCP). Direct immunofluorescence testing showed positivity for C3c in the dermo-epidermal junction, which corroborates the diagnosis.
Topical treatments with clobetasol and tacrolimus were initiated, associated with systemic therapy with hydroxychloroquine 400 mg per day, with significant improvement in this condition.
The discussion of this case is extremely relevant, as it is a rare case of Brunsting-Perry cicatricial pemphigoid isolated to the scalp. Therefore, clinical suspicion and investigation are of utmost importance to reach the right diagnosis and to provide the patient appropriate treatment for their pathology.

Figure 1: Lesions with different stages of evolution located in the crown region: blisters, erosions, scaly crusts, diffuse erythema and erythematous-whitish scar areas.

Figure 2: Exudative eroded lesion with scar pattern.

Figure 3: Eroded lesions with tortuous vessels and scaly crusts.
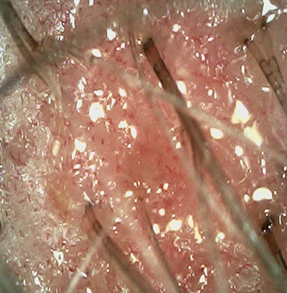
Figure 4: Exudative eroded lesions with punctate and comma-shaped vessels on the scalp.
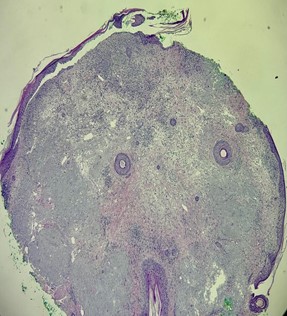
Figure 5: HE 40x: horizontal section at the level of the upper dermis and epidermis, showing a subepidermal cleft/cleavage and inflammatory infiltrate at the dermoepidermal junction. Marked photodamage (elastosis).
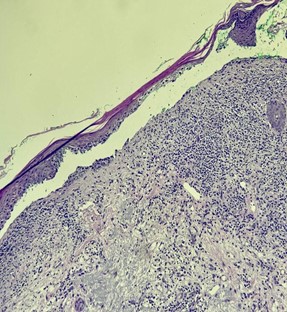
Figure 6: HE 100x in greater detail, a vesicobullous lesion with subepidermal cleavage and lymphoplasmacytic infiltrate in the upper dermis, vascular ectasia and discreet dermal fibrosis can be seen.
References
- Niknezhad N, Golchin N, Hasanzadeh S, Ghalamkarpour F. A rare case of cicatricial pemphigoid confined to the scalp with associated photodamage. Clin Case Rep, 2024; 12(8): e9281. doi: 10.1002/ccr3.9281.
- Barrón Hernández, Yevher Lorena, Lammoglia Ordiales Lorena, Toussaint Caire Sonia, Carreño Vázquez Paola Naomi, Guevara Díaz Jorge Alberto, et al. Alopecia cicatricial por penfigoide de Brunsting-Perry: reporte de caso y revisión de la literatura. Dermatología CMQ, 2022; 20(2): p. 181-184.
- Martín JM, Pinazo I, Molina I, Monteagudo C, Villalón G, Reig I, et al. Cicatricial pemphigoid of the Brunsting-Perry type. Int J Dermatol, 2009; 48(3): 293-294. doi: 10.1111/j.1365-4632.2009.03975.x.
- Das S, Blanco G, Ahmed A, Tran KT, Matthews LA, Pandya AG. Cicatricial pemphigoid of the scalp mimicking discoid lupus erythematosus. J Am Acad Dermatol, 2011; 65(4): 886-887. doi: 10.1016/j.jaad.2010.10.028.

