Relationship of PSQI with EEQ in Stress-Induced Obese Population in Gujrat Pakistan
Eman Chaudhary1, Aqna Malik2,*, Isha Asim Jarral1, Muhammad Haroon Ali1, Zumra Imran1 and Atifa Shafqat1
1Department of Pharmacy, University of Lahore, Lahore
2Department of Pharmacy, University of Chenab, Gujrat; Department of Pharmacy, University of Lahore
Received Date: 10/12/2024; Published Date: 14/02/2025
*Corresponding author: Dr. Aqna Malik, Department of Pharmacy, University of Chenab, Gujrat; Department of Pharmacy, University of Lahore, Lahore
https://orcid.org/0000-0003-3875-9621
Abstract
Background: Sleep is an essential requirement, and its frequency, quality, and consistency represent critical
variables. Alterations in sleep patterns and quality can impact individuals at an early age, resulting in effects that include diminished academic performance and worse physical and mental health. Obesity is a contributing factor to sleep problems, such as obstructive sleep apnea and restless leg syndrome.
Objective: The primary aim of the study was to evaluate the impact of workload stress on sleep duration and its quality and its link with eating disorders and obesity.
Methods: Cross-sectional study was planned in the general population in the vicinity of the University of CHENAB, Gujrat, in the Gujrat division, after ethical approval. Data was obtained from participants who had visited any psychological clinic during the past 3 months for sleep disturbances. To evaluate eating disorders, the Emotional Eater Questionnaire (EEQ) was used and to investigate sleep quality and sleep duration PSQI_TOTAL_SCORE was used. A PSQI score over 5 has been established as highly sensitive and specific in differentiating between good and poor sleepers among participants of the survey.
Results: Participants were classified according to weight as Underweight (male:7.8±0.8, Female:16.65±1.0), Overweight (male:28.89±1.01, Female:29.78±1.02), Obese Class I (male:30.30±0.9, Female:31.6±0.7), Obese Class III (male & female each 41.3±1.02) depending upon their occupation and impact of workload induced stress on their sleep duration. Participants of occupations like Labourer (male) had long working hours/day (9-10hrs) with less sleep duration (3-6hrs). Similarly, participants doing Family Business Look after, private employees, businesswomen, female teachers, males, and females who have to quit their jobs before retirement age were also suffering from sleep disturbances and less sleep duration (3-6hrs) and graded between (21-30). Due to stress and inefficient sleep quality, they tend to eat irregularly and they were classified as emotional and very emotional eaters as per the criteria of EEQ. They were grouped as overweight, Obese Class I and III due to eating disorders. Male & Female students were also suffering from stress-induced sleep disturbances and >6hrs sleep duration however they were underweight but females tend to eat irregularly.
Conclusion: The quality of sleep is associated with depression, overall quality of life, and eating disorder behaviors leading to obesity. Sleep quality was correlated with working hours, sleeping hours, and weight-related functioning while adjustment was done for age, BMI, and gender. Participants exhibiting poor sleep quality reported due to increased workload and stress. Eating disorders emerged as a significant predictor of weight-related functioning in regression analyses, with sleep showing only a tendency towards significance.
Keywords: Sleep disturbance; PSQI_TOTAL_SCORE; EEQ; Obesity; Eating disorders
Background
A disorder is a collection of symptoms that substantially disrupts an individual's daily functioning [1]. Medical conditions, including eating and sleep disorders, represent distinct biological anomalies [2]. Severe manifestations of these illnesses rapidly induce impairment and distress. Chronic unhealthy eating characterizes anorexia, bulimia, and related mental and physical problems [3] defined by an obsession with weight, body shape, and food consumption. Eating disorders frequently coexist with despondency, substance dependence, and anxiety. Sleep-wake disorders impact the quantity, timing, and quality of sleep, resulting in daytime difficulties and diminished functioning [4]. Sleep disorders impact numerous individuals and can lead to significant health complications. Anxiety, depression, and cognitive deficits commonly co-occur with these disorders [5]. The predominant sleep disorders encountered in primary care include insomnia, obstructive sleep apnoea, hyperinsomnia, circadian rhythm sleep disorders, parasomnias, REM sleep behavior disorder, and sleep-related movement disorders such as restless legs syndrome. Eating disorders are poorly understood, despite their seriousness [6]. Myths about eating disorders have grown in popularity over the last century. These myths portray eating disorders as; "a lifestyle choice," a "phase," or "about vanity." They also say that these disorders are exclusively a problem among "white upper-class females" and that they do not pose a health risk, do not affect people who are normally obese or overweight, and are even a result of parenting [16].
Polysomnography, a technique for accurately and consistently evaluating sleep and wakefulness, is fundamentally connected to the historical development of sleep psychology and sleep medicine. Sleep recording technology has significantly advanced during the past 50 years, owing to developments in both technology and science [12]. Moreover, advancements in sleep recording and assessment technologies have correlated with significant progress in sleep research and related diseases. Although polysomnography has transitioned sleep research from speculation to experimentation, the majority of studies concerning sleep and eating disorders have relied on surveys. There are no objective sleep metrics for bulimia nervosa or anorexia nervosa, and the sole data available for binge eating disorder is derived from autography. Night eating syndrome, characterized by delayed melatonin release and reduced sleep efficiency, is more correctly defined as a sleep disruption [17]. Future studies should integrate objectively recorded metabolic and sleep parameters with data on mental comorbidities to elucidate the interaction between appetite disorders and sleep disruptions in exacerbating symptoms, as well as to identify instances more susceptible to developing eating disorders [13]. Anorexia nervosa exhibits a wide prevalence among female individuals in western nations (van Eedan et al., 2021). Additional research on dietary attitudes has indicated a progressive rise in non-Western countries. Relationships between depressive mood, dissatisfaction with body weight and shape, and eating disorder behaviors [22] have been studied. The main reasons behind sleep disturbances are beverage consumption, poor mood, physical conditions, mental stress, altered circadian rhythms, workload, and excessive use of gadgets are main reasons behind sleep disturbances [22]. Stress may be due to excessive workloads, job instability, and self-dissatisfaction.
Objective: The main objective of our study was to compare the impact of eating habits on participants due to stress related with sleep disturbances.
Materials and Methods
Ethical Approval
The protocol of the study was approved by the ethics committee of the University of Chenab. An informed written/verbal consent form was provided to all participants prior participation in the cross-sectional survey-based study.
Survey procedure, sampling, and data collection
A cross-sectional study was carried out among the general population in the vicinity of the university of Chenab, Gujrat, Pakistan. Participants aged (16-50 yrs) were informed about purpose of survey and they have given verbal consent before start of survey. Partcipants were given no reward. No recruitment rate was recorded, but the vast majority of general population from different occupation and social circumstances were willing to participate. Survey was conducted by group of final year students of department of Pharmacy, university of Chenab, under supervision of Assistant Professor Dr Aqna Malik. As per inclusion criteria partcipants of both genders aged 16-50 yrs were included who were mainly facing occupational stress and sleep difficulties. Elderly and children were excluded.
Sample Size: The sample size was calculated by using Cochran provided formula with a desired confidence level (z), level of precision (e) and estimated proportion of the disease in the population. In this study by reviewing the systematic literature and expert opinion the proportion level of population is 30% with e= 6% and confidence level 95%. By using this value in formula, the minimum sample size is 225.
Instruments:
Emotional Eater Questionnaire (EEQ)
10-item questionnaire was developed to assess extent of emotions affecting eating behaviour. This questionnaire is termed as Emotional Eater Questionnaire (EEQ). Each questions had 4 possible replies 1) Never 2) Sometimes 3) Generally and 4) Always. Each reply scored from 1 to 4, the lower the score, the healthier the behaviour. Score range for explained as 0-5: non-emotional eater, 6-10: low emotional eater, 11-20: emotional eater, 21-30:very emotional eater
Pittsburgh Sleep Quality Index (PSQI)
The sleep quality of participants was assessed using the Pittsburgh Sleep Quality Index (PSQI), which was also translated into Urdu. The PSQI comprises 19 questions categorized into 7 components: sleep quality, sleep onset latency, sleep length, sleep efficiency, sleep disruptions, usage of sleep drugs, and daytime dysfunction. Each item is rated on a scale from 0 to 3, and the cumulative scores of the seven components constitute the global PSQI score, which spans from 0 to 21. A global PSQI score exceeding 5 signifies inadequate sleep compared to clinical and laboratory assessments, with elevated scores reflecting diminished sleep quality.
Data Collection Procedure:
Survey-based study was conducted from October 2023- January 2024. Demographic data regarding age, weight, height, and gender were noted. Self-reported weight &h eight enabled computation of BMI According to their BMI, Participants of survey were classified (WHO International Classification) as being under-weight (BMI: <18.5), overweight (BMI: 25.0–29.99), Obese class I (BMI: >30), Obese class III (BMI: >40). Participants were asked about their working hours, job timings and sleep time.
Statistical Analysis
Nonparametric statistics were used to compare the Pittsburgh Sleep Quality Index (PSQI) of participants with varying EDS scores of different age groups and categories (underweight, healthy weight, overweight, and obese). One sample t-test was used to analyze both instruments.
Results
Among 225 participants, 36.89% were males and 63% were females. The demographic profile of participants along with occupation, working hrs, and duration of sleep (hrs) was tabulated in (Table 1).
Table 1: Demographic distribution among participants according to BMI.
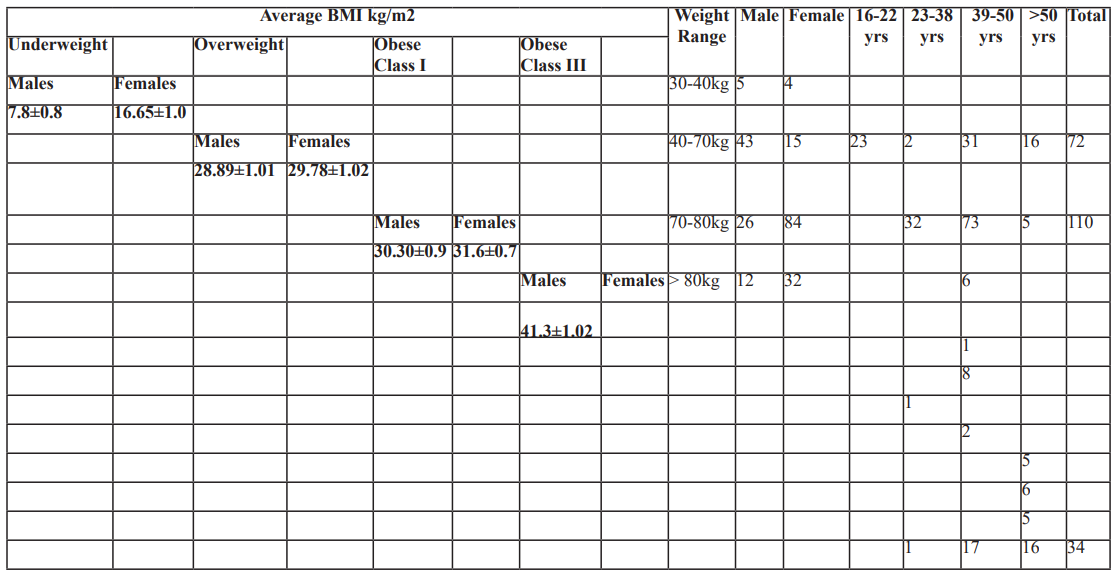
Data showed that middle aged adults from both genders have high tendency of obesity. Partcipants aged >50yrs are at greater risk of Obesity with average BMI 41.3 kg/m2 Obese Class III
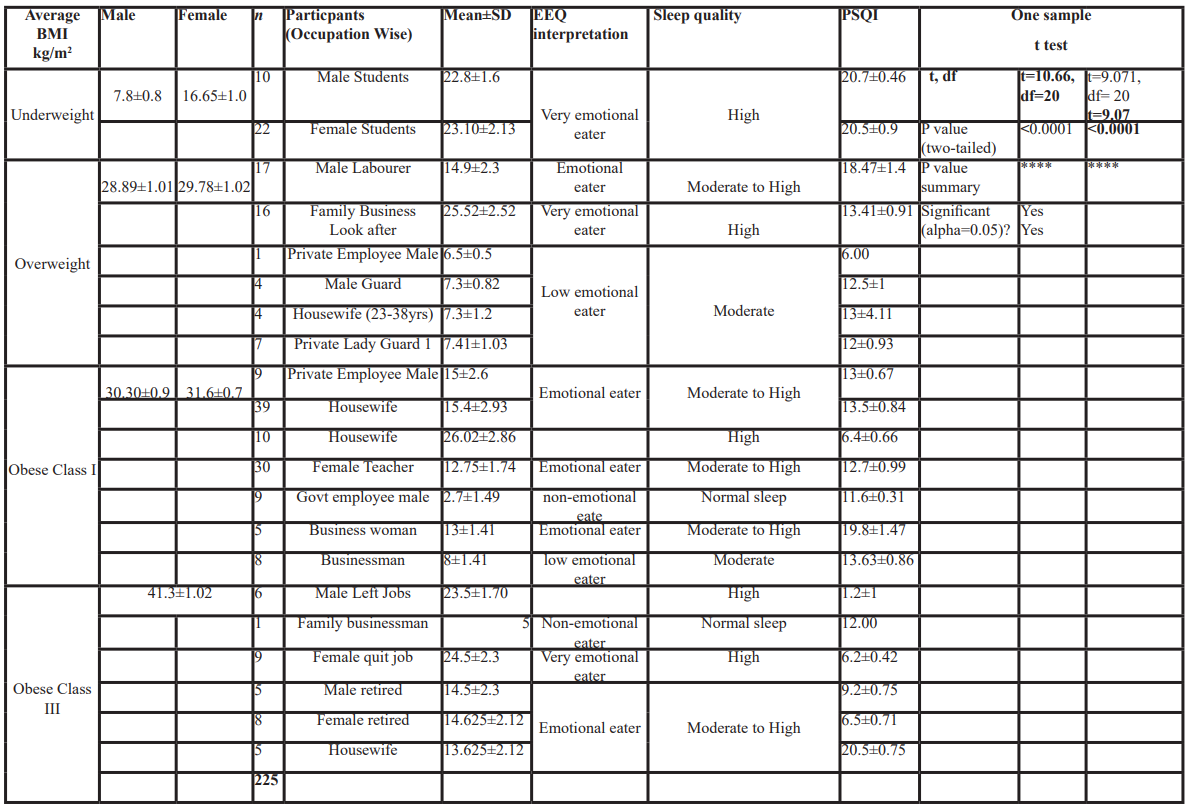
Emotional Eater Questionnaire (EEQ)
Participants were classified in 4 groups attending to the score obtained due to stress-induced due to workload and nature of the job. Replies of participants in the form of (1) Never (2) Sometimes (3) Generally and (4) Always were scored from 0 to 30. More scores value indicated poor control over eating food (Table 2).
PSQI_TOTAL_SCORE
Pittsburgh Sleep Quality Index (PSQI) was created by [10] It serves as a self-report assessment instrument to assessment sleep quality over a 1-month duration. A comprehensive (PSQI score, and 7 individual component scores were obtained from the scale, when participants from different age groups and occupations adopted it. The component scores include subjective sleep quality, sleep latency, sleep length, sleep efficiency, sleep disruptions, usage of sleep medicines, and daytime dysfunction. Each component was evaluated on a scale from 0 to 3, resulting in a total score that was from 0 to 21, A higher number indicated inferior sleep quality as seen with Male & female Students (22.8±1.6 & 23.10±2.13). A PSQI score > 5 has been established as highly sensitive and specific in differentiating between good and poor sleepers among participants of the survey (Table 3).
Table 2: Impact of stress and workload on sleep duration among participants.

Table 3: Comparison of PSQI&EEQ scoring among participants (Occupation-wise).
Discussion
Researchers who study examining the relationship between sleep quality and eating disorders eating mostly target clinical groups. This study is, to our knowledge, the first to evaluate the links between sleep disturbances and eating disorders while considering their effects on weight-related functioning in a substantial community sample. Poor sleep quality was prevalent and highly correlated with disordered eating, sadness, and compromised weight-related functioning. The robustness of these correlations persisted even after controlling for participants' age, BMI, and gender [11].
Concerning disrupted sleep, (52.9%) of participants indicated sleep quality exceeding the clinical threshold for poor sleep quality, with participants averaging 6.5 hours of average sleep during nighttime. This conclusion aligns with recent research on disrupted sleep in the general population (51%) [14] and is unexpectedly similar to prevalence estimates of sleep problems in individuals with identified eating disorders (57%) [9,14] and in a clinical population post-sleeve gastrectomy (58.6%) [23]. The rate similarities further substantiate the authenticity of the existing data obtained from MTurk. In both the paper by Lawson et al. [23] and the present study, average sleep lengths were below the National Sleep Foundation's recommendation of 7–9 hours per night for adults [41]. Previous and current findings indicate that the biggest obstacles to sleep are difficulty initiating sleep and nocturnal awakenings [22, 23]. Excess weight has been identified as a more widespread sleep-related issue in clinical populations, leading to pain and disrupted sleep. Recent data suggest that sleep intervention strategies may vary based on the population, advocating for a precision medicine approach. For instance, enhancing sleep onset in community samples as opposed to pain treatment in clinical samples. The widespread occurrence of sleep onset difficulties in various populations suggests potential environmental factors that may aggravate this issue, including technology usage, shift employment, and social demands for continuous productivity [20].
Current survey is the first of its kind which found a correlation between eating habits and sleep quality in different occupations or retired persons in the population of Gujrat, Pakistan. A strong correlation was found between the short sleep duration of students and emotional eating p<0.0001. Both male and female students face more stress due to excessive workload, which disturbs their sleep patterns [15]. Due to the short duration of sleep, they have a very emotional eating behavior which may lead to obesity. Both male and female students have nearly the same PSQI and EEQ values. Moreover, participants who look after the family business was found to have highly disturbed sleep patterns and in turn developed irregular eating patterns leading to obesity. Housewives also suffered sleep deprivation due to unequal workload and stress induced by prolonged working hours which may lead to sleep disturbances (PSQI= 26.02±2.86 and in turn increased EEQ = 6.4±0.66) [21]. Sleep deprivation may lead to increased and irregular food intake as those women found in obesity class I. Sleep deprivation is a common chronic stressor that may contribute to increased risk for obesity and metabolic diseases, including abdominal obesity, insulin resistance, hypertension, and atherosclerosis, that may predispose individuals to CVS and type 2 DM. It is estimated that roughly 30% of all adults in the US sleep > 6h per night [18,19]. Current Cross-sectional study also have found a significant association between short sleep duration and increased prevalence of obesity or higher BMI in both males and females [7]. Males and Females who quit jobs had (PSQI= 6.2±0.42 &1.2±1 and in turn increased EEQ =24.5±2.3 & 23.5±1.70) with highly disturbed sleep levels due to stress and > 6hrs sleep duration and had an increased tendency of obesity due to emotional eating behaviors.
Besides the comparatively elevated prevalence of inadequate sleep quality, significant findings encompass the correlation between sleep quality and eating disorders in the current study. Yeh and Brown et al., It was found that increased workload and social stress related with work scenarios can cause sleep deprivation and obesity.
Conclusion
The quality of sleep is associated with depression, overall quality of life, and eating disorder behaviors leading to obesity. Sleep quality was correlated with working hours, sleeping hours weight-related functioning while adjustment was done for age, BMI, and gender. Participants exhibiting poor sleep quality reported due to increased workload and stress and eating disorders emerged as a significant predictor of weight-related functioning in regression analyses, with sleep showing only a tendency towards significance.
Clinical ramifications
This study offers a cross-sectional assessment of the intricate links among eating disorders, sleep, depression, and weight-related functioning within a community sample
Strengths
- The novel amalgamation of sleep, diet, and weight-related factors represents a substantial benefit of our research. Furthermore, the sample size is significant and community-focused, with participants assessed using validated tools.
- The participants included a varied range of ages and body mass indices, comprising both males and females.
Limitations
- The participants were primarily from a single region.
- All measurements were self-reported from a convenience sample collected.
- Thorough and rigorous assessments of data validity were performed; nevertheless, examining the relationship between sleep patterns, eating disorders, and weight-related functioning in a large, diverse participant cohort could improve population-based evaluation and intervention.
A universal need exists for further research to improve comprehension and meet the needs of various community samples that may resemble clinical samples in terms of sleep duration, sleep quality, and maladaptive eating patterns.
References
- Nugraha B, Gutenbrunner C, Barke A, Karst M, Schiller J, Schäfer P, et al. The IASP classification of chronic pain for ICD-11: functioning properties of chronic pain. Pain, 2019; 160(1): 88-94.
- Foster RG. Sleep, circadian rhythms and health. Interface Focus, 2020; 10(3): 20190098.
- Ferreira BAGG. Eating Disorders and Gastrointestinal Diseases: relationship, coexistence and state of the art, 2023.
- Sun Y-Y, Wang Z, Zhou H-Y, Huang H-C. Sleep–Wake Disorders in Alzheimer’s Disease: A Review. ACS Chemical Neuroscience, 2022; 13(10): 1467-1478.
- Ramasubramanian B, Reddy VS, Chellappan V, Ramakrishna S. Emerging materials, wearables, and diagnostic advancements in therapeutic treatment of brain diseases. Biosensors, 2022; 12(12): 1176.
- Keel PK, Klump KL. Are eating disorders culture-bound syndromes? Implications for conceptualizing their etiology. Psychological bulletin, 2003; 129(5): 747.
- Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel HI, Qahwaji DM,
- Prevalence of short sleep duration and its association with obesity among adolescents 15-to-19-year-olds: A cross-sectional study from three major cities in Saudi Arabia. Annals of thoracic medicine, 7(3): 133-139.
- Barnes RD, Palmer B, Hanson SK, Lawson JL. Sleep is the best medicine: assessing sleep, disordered eating, and weight-related functioning. Eat Weight Disord, 2023; 28(1): https://doi.org/10.1007/s40519-023-01610-y.
- Buysse DJ, Reynolds CF, 3rd Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res, 1989; 28(2): 193-213. https://doi.org/10.1016/0165-1781(89)90047-4.
- Carollo A, Zhang P, Yin P, Jawed A, Dimitriou D, Esposito G, et al. Sleep Profiles in Eating Disorders: A Scientometric Study on 50 Years of Clinical Research. Healthcare (Basel), 2023; 11(14). https://doi.org/10.3390/healthcare11142090.
- De Zambotti M, Goldstein C, Cook J, Menghini L, Altini M, Cheng P, et al. State of the science and recommendations for using wearable technology in sleep and circadian research. Sleep, 2024; 47(4):
- Degasperi G, Meneo D, Curati S, Cardi V, Baglioni C, Cellini N. Sleep quality in eating disorders: A systematic review and meta-analysis. Sleep Med Rev, 2024; 77: https://doi.org/10.1016/j.smrv.2024.101969
- Fabbri M, Beracci A, Martoni M, Meneo D, Tonetti L, Natale V. Measuring Subjective Sleep Quality: A Review. Int J Environ Res Public Health, 2021; 18(3). https://doi.org/10.3390/ijerph18031082
- Faris ME, Vitiello MV, Abdelrahim DN, Cheikh Ismail L, Jahrami HA, Khaleel S, et al. Eating habits are associated with subjective sleep quality outcomes among university students: findings of a cross-sectional study. Sleep Breath, 2022; 26(3): 1365-1376. https://doi.org/10.1007/s11325-021-02506-w
- Jalali-Farahani S, Amiri P, Lashkari B, Cheraghi L, Hosseinpanah F, Azizi F. Prognostic value of different maternal obesity phenotypes in predicting offspring obesity in a family-based cohort study. BMC Public Health, 2021; 21(1): https://doi.org/10.1186/s12889-021-10932-4.
- Kennedy KE. The Mouth After Midnight: Nocturnal Wakefulness and Eating Behavior The University of Arizona, 2024.
- Knutson KL, Van Cauter E. Associations between sleep loss and increased risk of obesity and diabetes. Ann N Y Acad Sci, 2008; 1129: 287-304. https://doi.org/10.1196/annals.1417.033.
- Merdad RA, Akil H, Wali SO. Sleepiness in adolescents. Sleep medicine clinics, 2017; 12(3): 415-428.
- Ogilvie RP, Patel SR. The epidemiology of sleep and obesity. Sleep Health, 2017; 3(5): 383-388. https://doi.org/10.1016/j.sleh.2017.07.013.
- Saleh-Ghadimi S, Dehghan P, Abbasalizad Farhangi M, Asghari-Jafarabadi M, Jafari-Vayghan Could emotional eating act as a mediator between sleep quality and food intake in female students? Biopsychosoc Med, 2019; 13: 15. https://doi.org/10.1186/s13030-019-0154-3.
- Sander J, Moessner M, Bauer S. Depression, Anxiety and Eating Disorder-Related Impairment: Moderators in Female Adolescents and Young Adults. Int J Environ Res Public Health, 2021; 18(5). https://doi.org/10.3390/ijerph18052779.
- van Eeden AE, van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry, 2021; 34(6): 515-524. https://doi.org/10.1097/yco.0000000000000739.

