Hepatic Abscesses Secondary to Chorioamnionitis: A Case Report of a Rare Obstetric Complication
Soukaina Bahha*, Najlae Lrhorfi, Salma El Aouadi, Asmae Guennouni, Chaimae Abourak, Lina Belkouchi, Nazik Allali, Siham El Haddad and Latifa Chat
Mother-Child Radiology Department, Pediatric Teaching Hospital, Mohammed V University, Rabat, Morocco
Received Date: 08/11/2024; Published Date: 18/11/2024
*Corresponding author: Soukaina BAHHA, Mother-Child Radiology Department, Pediatric Teaching Hospital, Mohammed V University, Rabat, Morocco
Abstract
This is a rare case of abscess secondary to chorioamniotitis, a complication rarely encountered in gynecological practice.
A 19-year-old woman underwent a Caesarean section for chorioamnionitis, presenting with diffuse abdominal pain and fever a few days later. An abdominal and pelvic CT scan was performed, showing a hepatic collection in favor of an abscess, which was then managed by scanno-guided drainage in addition to antibiotherapy. The patient subsequently showed good clinical improvement.
Pyogenic liver abscesses are uncommon and usually polymicrobial in nature, They are also a rare etiology of puerperal fever, and are often associated with non-specific symptoms.
the prognosis for hepatic abscess remains somewhat bleak, with a mortality rate of 15% if the patient does not benefit from adequate diagnosis and prompt and effective treatment.
Keywords: Liver abscess; Chorioamnionitis; Scanno-guided drainage; Case report
Introduction
The most commonly infections in the puerperium which are being reported are endometritis, wound infections, genital tract infections, mastitis, thrombosis, and urinary tract infections.
Pyogenic liver abscesses are uncommon in clinical practice and are usually polymicrobial in nature, with members of the Enterobacteriaceae family often implicated.
They are also an uncommon etiology of fever in the puerperium and are often associated with nonspecific symptoms.
Our case shows the importance of imaging in the evaluation of the abdomen, for any female patient who has presented with diffuse abdominal pain with fever, in the puerperium especially with the antecedent of chorioamnionitis our case also shows that, despite its rarity, liver abscess should always be considered, especially in the presence of right quadrant pain.
No cases of liver abscesses secondary to chorioamnionitis have been reported in the literature.
Case Report
A 19-year-old woman with no personal medical or surgical history, who had an unattended pregnancy complicated by chorioamnionitis, following which she underwent a caesarean section in another hospital. Three days later, she presented with diffuse abdominal pain that did not respond to analgesics, associated with a fever of 38, for which she was referred to our emergency department. On admission, the patient had a correct blood pressure, was slightly tachycardic, febrile at 39, and had diffuse abdominal tenderness, blood formula numeration showed hyperleukocytosis ( 15x10 3 /μl) with neutrophilic polynuclear predominance at 7x10 3 /μl, and CRP was around 120mg/l, a pelvic ultrasound was performed, which showed a very large uterus (post-gravid), with moderate peritoneal effusion, an abdominal and pelvic CT scan were requested and showed a hepatic fluid formation involving segments IV, VII and VIII, coarsely oval, poorly bounded, not enhanced after injection (Figure 1), suggestive of a hepatic abscess, associated with a large peritoneal effusion and postoperative air bubbles (Figure 3), and of course, a uterus increases in size (post-gravidic) : (Figure 2), and hepatic ultrasound confirmed the presence of the above-mentioned collection, which had a thin wall and heterogeneous echogenic content.
Our patient underwent scanno-guided drainage of the liver abscess followed by antibiotic therapy for 6 weeks, and showed a positive outcome.
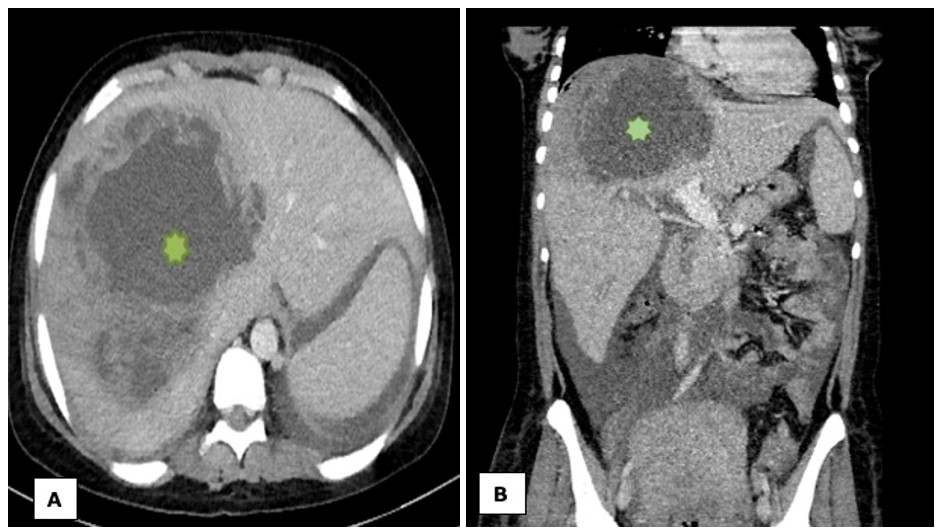
Figure 1: Axial section (A) and coronal section (B) of a portal-injected CT scan showing a voluminous collection in the hepatic segments IV, VII and VIII (green star).
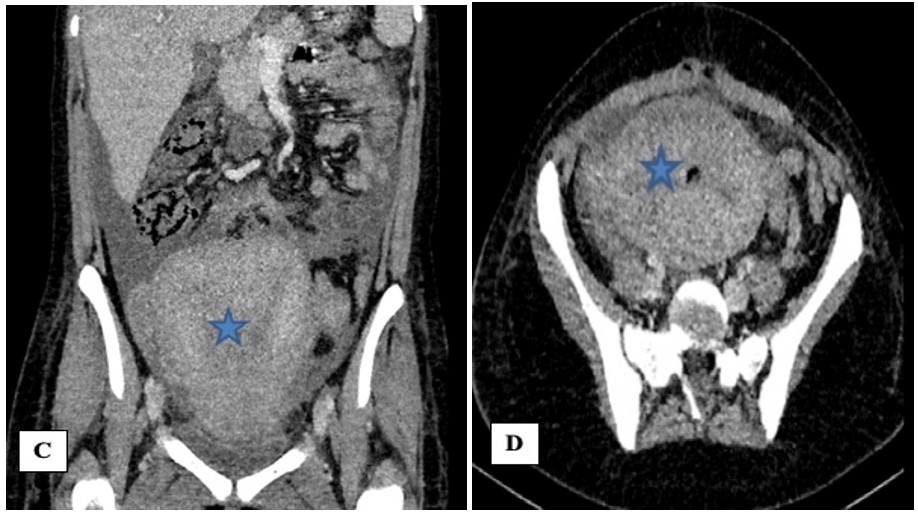
Figure 2: Coronal (C) and axial (D) sections of a pelvic injected CT scan showing a post-gravid uterus (blue star).
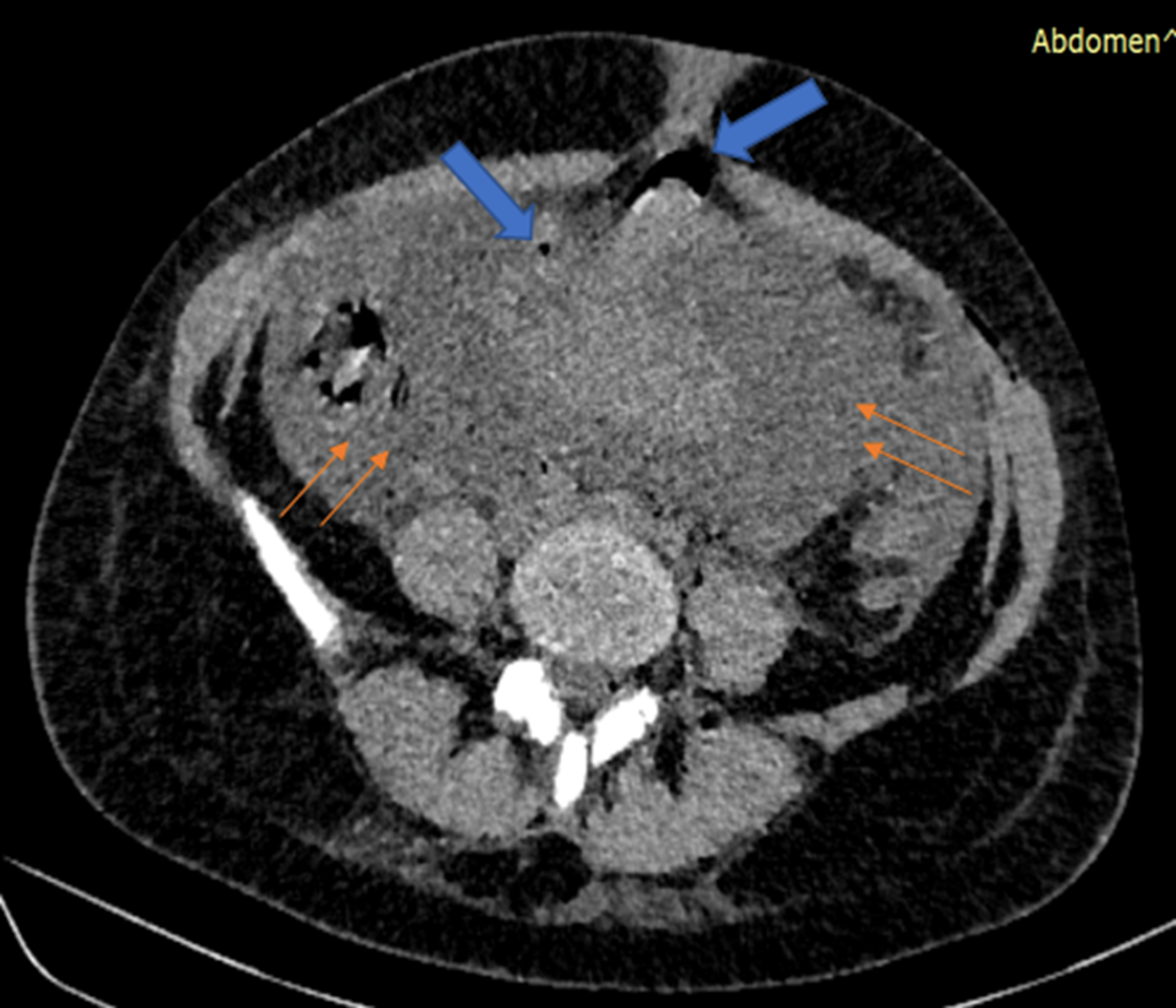
Figure 3: axial section of a pelvic injected CT scan showing large peritoneal effusion (orange thin arrows) with bubbles of pneumoperitoneum opposite the laparotomy scar (Blue arrows).
Discussion
Liver abscesses usually result from direct dissemination caused by peritonitis or biliary tract infection or, indirectly, secondary to hematogenous dissemination [1].
Various micro-organisms are associated with liver abscesses, such as amoebiasis, Listeria monocytogenes, brucellosis, Staphylococcus aureus, Escherichia coli and polymicrobial infections[2].
Pyogenic liver abscesses are rare, with only 11 cases per million people per year[3],
The main risk factor for pyogenic liver abscess is the coexistence of a biliary tract anomaly (obviously absent in our patient) [3]. It seems that in our patient, the route of dissemination was hematogenic, after she had presented with chorioamnionitis, for which she underwent a cesarean section.
Clinically, there are no specific signs pointing to liver abscess; most often, there is pain in the right quadrant with fever, biological tests are also non-specific, usually showing hyperleukocytosis, increased alkaline phosphatase and hyperfibrinogenemia, which are non-specific during pregnancy and puerperium[4].
Most infections encountered during pregnancy and in the puerperium are due to the presence of methicillin-resistant Staphylococcus aureus, and serious post-partum complications recently attributed to MRSA include surgical site infection, sepsis, septic thrombophlebitis and septic pulmonary embolism [5].
from a radiological point of view, among the diagnoses to be considered in the presence of liver fluid lesions are cysts of parasitic, fungal or pyogenic origin, simple hepatic cysts, cystic or necrotic tumors, and cysts with hematic content [2]. In our case, we found a fluid lesion with a slightly thickened wall and heterogeneous echogenic content, and in view of the patient's clinical presentation, we first considered the diagnosis of a liver abscess. CT scan, abdominal ultrasound and CT-guided drainage confirmed the existence of a liver abscess.
Treatment of pyogenic liver abscess consists of percutaneous drainage and the use of antibiotics for two to six weeks. Prompt diagnosis and treatment are essential due to the high mortality rate described in the literature, which can be as high as 100% in untreated cases. Mortality rates of 28% have been reported for patients treated with antimicrobial agents alone, versus 4% for patients treated with drainage and antimicrobial agents[2]. in our case, management was rapid, and drainage of the liver abscess was not delayed as the patient had no abnormal coagulation tests.
Conclusion
Pyogenic liver abscess during pregnancy and puerperium is a serious condition that represents a diagnostic and therapeutic challenge, with few cases reported. Normally non-specific clinical and laboratory findings can lead to late diagnosis, increasing the risk of maternal morbidity and mortality.
Contributors
- Najlae LRHORFI, Salma El AOUADI contributed to the conception, acquisition, analysis, interpretation of data, and drafted the manuscript.
- Asmae Guennouni, Chaimae Abourak contributed to the acquisition and interpretation of data.
- Siham El HADDAD, Najlae LRHORFI contributed to the conception and acquisition of data, and critically revised the manuscript.
- All authors read and approved the final manuscript.
Conflict of interest statement: The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding: No funding from an external source supported the publication of this case report.
Acknowledgements: This case report would not have been possible without the help of many doctors who worked hard and provided excellent care to the patients. We would like to thank the central radiology department of Avicenna Hospital in Rabat for agreeing to perform the ultrasound-guided drainage for our patient. We would also like to thank the visceral surgery department for agreeing to admit the patient and provide the necessary care. Additionally, we want to thank Dr. Najlae Lrhorfi for her help in the final diagnosis, and Professor Siham El Haddad for her interest in this work and for ensuring its publication.
References
- Rahimian J, Wilson T, Oram V, Holzman RS. Pyogenic liver abscess: recent trends in etiology and mortality, Infect. Dis. Off. Publ. Infect. Dis. Soc. Am., 2004; 39(no 11): p. 1654‑1659. doi: 10.1086/425616.
- Sherer DM, et al. Sonography and Magnetic Resonance Imaging of a Maternal Methicillin-Resistant Staphylococcus aureus Liver Abscess at 33 Weeks’ Gestation. Ultrasound Med., 2010; 29(no 6): p. 989‑992. doi: 10.7863/jum.2010.29.6.989.
- Khanna N, Inkster T, et al. Meticillin-resistant Staphylococcus aureus hepatic abscess treated with tigecycline. Clin. Pathol., 2008; 61(no 8): p. 967‑968. doi: 10.1136/jcp.2008.056689.
- Silva FX, Souza ASR. Puerperal sepsis caused by liver abscess: case report. Bras. Saúde Materno Infant., 2017; 17: p. 853‑858. doi: 10.1590/1806-93042017000400013.
- Methicillin-resistant Staphylococcus aureus bacteremia and chorioamnionitis after recurrent marsupialization of a bartholin abscess - PubMed. Consulté le: 2024.

