Evaluation of Drug Treatment Awareness, Prescription Patterns and Perceived Drug Adherence in COPD Patients: Vital Determinants in COPD Management
Raakhi Tripathi1,*, Nayana Shetty1, Sharmila V Jalgaonkar1, Snehalata Gajbhiye2, Sharika Pillay1 and Amita Athavale3
1Department of Pharmacology and Therapeutics, Seth GS Medical College and KEM Hospital, India
2Department of Pharmacology, All India Institute of Medical Sciences, India
3Department of Chest Medicine, Seth GS Medical College and KEM Hospital, India
Received Date: 04/11/2024; Published Date: 14/11/2024
*Corresponding author: Raakhi Tripathi, Department of Pharmacology & Therapeutics, Seth GS Medical College and KEM Hospital, Mumbai, India
Abstract
Introduction: Adherence to pharmacotherapy in patients with Chronic obstructive pulmonary disease (COPD) is essential to prevent disease progression. Patient awareness towards drug treatment and accurate inhaler use technique is one of the contributing factors to ensure adherence, hence the present study was conducted.
Methodology: A cross-sectional, single-center, questionnaire-based study was conducted in the Chest medicine OPD of a tertiary care hospital from July 2019- December 2020.Consented patients of either gender, aged > 18 years, with confirmed diagnosis of COPD, who had prescriptions of last 3 months, were included. Prescription details were recorded, subsequently patients were administered pre-validated questionnaires on drug treatment awareness (9 items, total score=9), steps of inhaler use checklist (9items, total score =9) and self-reported medication adherence (6 items, total score =6).
Results: The mean drug treatment awareness score was 5.62±1.97 and 95 (52%) patients scored > 50% (≥5 / 9). Similarly, 132/180 participants (73.3%) scored > 50%, with a mean score of 4.71±1.32 in the treatment adherence questionnaire. 115 (63.9%) participants were aware of the steps on how to use an inhaler and the mean inhaler use technique score was 5.52. COPD prescriptions (n=233) containing 903 drugs were analyzed and Tiotropium bromide inhaler and theophylline+ etophylline FDC were the most prescribed drugs.
Conclusion: COPD patients were aware of the drug regimen, inhaler use technique but awareness regarding drug name, adverse effects was poor. Similarly, awareness about inhaler use technique steps of breath holding and mouth gargling was lacking. More than 2/3rd of the participants had a perceived drug adherence score more than 50% with mean score of 4.71 out of 6. Most prescribed drug in the prescriptions was inhalational tiotropium bromide and FDC was Theophylline + etophylline. Hence patient reinforcement programs on medication regimen, adverse effect profile and compliance needs to be implemented.
Keywords: Beta agonists; Antimuscarinics; Questionnaire; Adverse effects
Introduction
Chronic Obstructive Pulmonary Disease (COPD), a chronic inflammatory disease characterized by persistent respiratory symptoms and airflow limitation. COPD is the third leading cause of death worldwide, causing 3.23 million deaths in 2019 and is the seventh leading cause of poor health worldwide [1]. In India the prevalence ranged between 2 to 22% among the men and 1.2 to 19% among women in different population-based studies [2]. The Disability Adjusted Life Years (DALYs) due to COPD increased to 36.3% from 1990 to 2016 and it became 2nd leading cause of DALYs in India. Thus, the deleterious impact of the disease is increasing over the years [3].
Non-adherence in COPD leads to an increased risk of poor clinical outcomes, poor symptom control, increasing number of relapses, higher mortality rate, increased health costs. Factors contributing to non-adherence in COPD are age, current smoking status, number of respiratory drugs / high dose frequency, incorrect inhaler use technique, presence of co-morbidities [4-6]. Patient unawareness about their treatment also adds to poor adherence to medical therapy.
Drug therapy for COPD, which includes Short acting beta agonists (SABA), Long-acting Beta agonists (LABA), Long-acting muscarinic antagonists (LAMA), Inhaled corticosteroids (ICS) etc. are administered for long duration thus it is crucial for the patient to be compliant to their medications to prevent further progression of the disease. Despite the available pharmacological treatment, the burden of COPD is still increasing.
There are ample numbers of studies assessing the prescription patterns in COPD patients and documenting low adherence of patients to COPD drug treatment. No specific study assessing patient’s knowledge of their drug treatment in terms of drugs prescribed, dose, frequency of dosing and its adverse effects. The present study was planned to assess the patient awareness to COPD drug treatment, their perceived adherence and evaluate the prescription variability in COPD patients.
Methodology
This study was a cross-sectional, single-centre, questionnaire-based study conducted in the chest medicine OPD of a tertiary care hospital from July 2019 to December 2020.The study was initiated after obtaining approval from the Institutional Ethics Committee (EC/162/2018) and was registered with the Clinical Trials Registry of India at www.ctri.nic.in. This study was conducted in compliance with the National Ethical Guidelines for Biomedical and Health Research Involving Human Participants issued by ICMR [7] and the ICH Good Clinical Practice (GCP) guidelines [8].
Participants of either gender, aged >18yrs with confirmed diagnosis of COPD (FEV1/FVC <0.70 on spirometry), who came for their annual Pulmonary Function Test check-up to the chest medicine OPDand provided written informed consent were included. COPD patients admitted in chest medicine wards/emergency department and who were critically ill were excluded from the study.Participants were recruited using convenience sampling technique.As there were no other studies done to assess drug treatment awareness amongst COPD patients no formal sample size calculation was done.
Demographic details such as age, gender, education, and socio-economic status were recorded in the case record form (CRF). Information regarding participant 's COPD disease duration and grade, smoking status, duration, and number of exacerbations in the past 1 year, presence of comorbid conditions, were also recorded.
Details (generic / brand name, dosage form, dose, frequency, type of COPD drug and duration) of the current prescription and of prescriptions given over the last 3 months were recorded in the CRF. Prescriptions were evaluated for incompleteness in terms of dose, dosage form, frequency, duration,or dosage instructions.
The participants were administered with a prevalidated (CVR= 0.8) drug treatment awareness questionnaire. The drug treatment awareness questionnaire consisted of 9 items that were grouped under 3 domains (Drug regimen, Inhaler use technique, and adverse effects). Response to each item was captured as Yes or No and scored as 1 and 0 accounting for a total awareness score =9. If patients stated that they were aware of the medicines written in their prescription they were probed further to state the number of medicines, the names, dosage form, frequency and duration of each medicine prescribed. Similarly, participants who were aware on how to use “an inhaler” were further assessed regarding the details of the steps of inhaler use using a 9 item prevalidated (CVI= 0.8) inhaler use checklist. A separate score out of 9 was given depending on number of steps stated correctly.
The participants were also administered with a Prevalidated (CVR= 0.86) drug treatment perceived adherence questionnaire consisting of 6 items. The responses were recorded as ‘yes’ (scored as 1) or ‘No’ (scored as 0), thus accounting a total perceived adherence score as 6.
The data obtained from the CRF was entered and analysed using descriptive statistics. The percentage of participants scoring above 50% (i.e., score ≥ 5) in drug treatment awareness questionnaire, who responded as Yes / No for each item of drug treatment awareness questionnaire, total awareness scores, domain wise awareness scores, the % of participants stating accurately each step on inhaler use checklist along with the inhaler use technique scores was calculated.
Drug utilization WHO indicators as average number of drugs prescribed /encounter, average number of drug class (beta agonists/antimuscarinics/steroid/methylxanthines/antibiotics)/ per encounter, percentage of drugs prescribed by generic / brand name, percentage of encounters with an injection/inhaler, percentage of drugs from the national list of essential medicines (NLEM) / WHO essential drugs list and percentage of complete/incomplete prescriptions was calculated. In addition, Prescribed Daily Dose/ Defined Daily Dose (PDD/DDD) ratiofor individual COPD drugs were also calculated.
Results
Total 180 COPD patients were enrolled. The mean(±SD) age of participants was 65+8.37years. The number of males (175, 97.2%) that participated in the study were greater as compared to females (5, 2.8%). Most of the patients belonged to the upper lower class (136, 75.6%) followed by lower middle class 39 (21.7%) while upper middle class were only 5(2.8%) patients.Most participants had completed middle school education (71, 39.4 %)while patients who completed primary school education were 64(35.6%) followed by high school 32 (17.7 %) and very few were illiterate 13(7.2%).
Maximum patients had quit smoking (130, 72.2%), currently smoking wasonly30 (16.7 %) while 20 (11%) patients never smoked. Similarly maximum participants smoked for a duration >10 years (153, 85%).
Drug treatment awareness in patients
95 participants out of 180 (52.8%) scored more than 50% i.e., ≥ 5/9, in the drug treatment awareness questionnaire. Domain I, Domain IIand Domain III had a mean awareness score of 1.75±0.94, 2.18±0.66 and 1.17±0.96 respectively and the overall mean awareness score was 5.62±1.97 (out of a total score of 9). The drug treatment awareness questionnaire itemwise responses are stated in Table 1
97 /180 (53.9%) patients mentioned the medicines written in the current prescription. Among these 97 participants it was seen that 92 (94.8%) participants were able to correctly state the number of medicines, drug frequency and 96 (99%) participants were able to correctly state the dosage form and duration of each medicine prescribed. But only 68 (70.1%) participants were able to correctly state the name of each medicine prescribed.
With regards to whether the participant was aware of the steps on how to use an inhaler, only115 (63.9%) participants responded as Yes. These 115 participants were further probed and asked to enumerate the steps. Side All 115 (100%) participants were able to enumerate that the inhaler is held correctly, while only 90 (78.3%) participants were able to enumerate that while starting to inhale by pressing down for inhalation, holding breath, and slowly breath out nose.The mean score for enumerating the steps of inhaler use correctly out of 9 among all the participants was 5.52±1.42 (mean±SD).The patient awareness on each inhaler step is mentioned in Table 2.
Drug treatment adherence in patients
In the patient perceived drug treatment adherence questionnaire, 132/180 (73.3%) participants scored more than 50% i.e., >3/6, with a mean score of 4.71±1.32. Item-wise responses of the patients have been described in table 3.
The 144 participants who responded as Yes were further probed to enumerate what they should do on skipping medications and majority (112, 77.8%) gave a correct response (i.e., to take the dose when they remember and continue regimen) followed by 19 (13.2%) participants who gave an incorrect response (i.e., to take double dose at next dosing). Whenenquired if the participant ever stopped taking medicines for a long time, against doctor advice, only 20 (11.1%) participants who responded as Yes were further probed and were asked to enumerate the reason for stopping and majority (10, 50%) could not enumerate the reason for stopping the medication followed by 5 participants who gave the reason as forgetfulness, 4 participants stated travelling and 1 participant attributed alcohol consumption for stopping medicines against doctor advice.
Prescription pattern analysis:
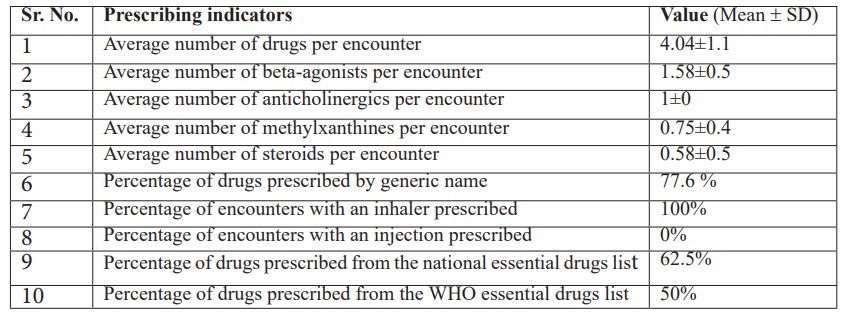
At the end of the study, 223 prescriptions were obtained for analysis from the 180 participants enrolled in the study. These prescriptions were then scrutinized based on the WHO drug use indicators (Refer Table4). Average number of drugs prescribed per encounter was4.04±1.1, while the average number of beta-agonists/ anticholinergics/ methylxanthines/ steroids per encounter were 1.58 /1 /0.75 and 0.58 respectively.
Percentage of drugs prescribed by generic name was 77.6% while percentage of encounters with an inhaler was 100%. 62.5% of the drugs were from the national essential drugs list while 50 % of the drugs were from the WHO essential drugs list.
In this study it was seen that majority of the prescriptions, i.e., 197 (88.3 %) out of 223 COPD prescriptions were complete in terms of dose, dose frequency, dosage form, duration of administration, instructions on when to take the medicine and presence of prescriber designation/signature. A total of 902 drugs were prescribed in 223 prescriptions collected. Amongst these 745 were COPD medications and remaining were concomitant drugs.
Table1: Item wise responses on drug treatment awareness questionnaire by COPD patients (n=180).
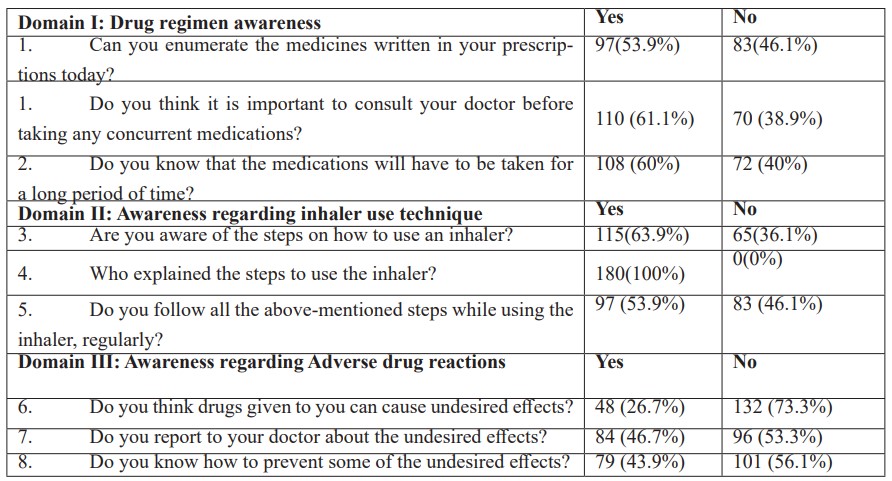
Table 2: Item wise responses on steps of inhaler use technique in COPD patients aware of inhaler use (n=115).
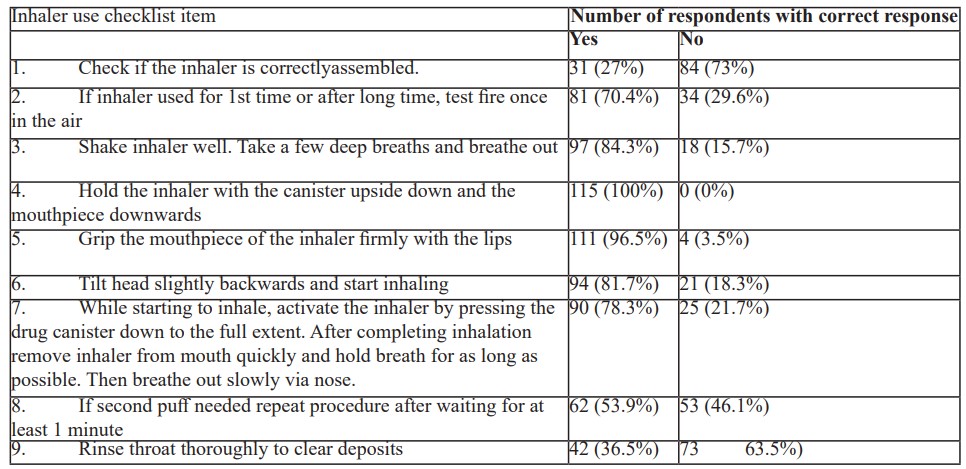
Table 3: Item wise responses of COPD patients (n=180) on perceived drug treatment adherence questionnaire.
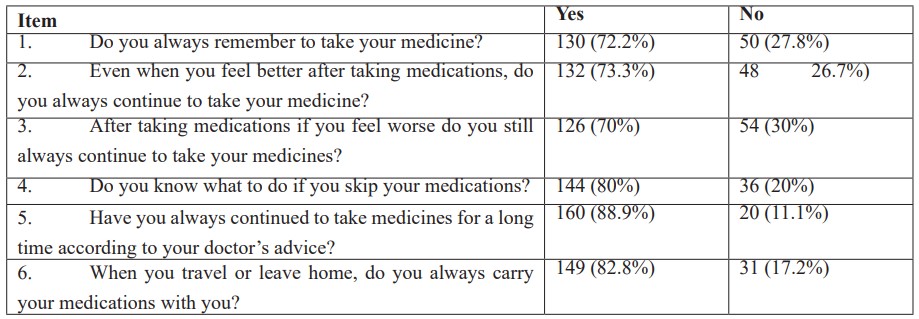
Table 4: WHO prescribing indicators from prescriptions collected from COPD patients.
Discussion
In this study COPD patients (n=180) were aware of the drug regimen but awareness regarding drug name and their adverse effects was poor. Similarly, 75% patients were aware of inhaler use technique but awareness regarding steps of breath holding and mouth gargling was poor. More than 2/3rd of the participants had a perceived drug adherence score more than 50% with mean score of 4.71 out of 6. Most prescribed drug in the prescriptions was inhalational tiotropium bromide and FDC was Theophylline + etophylline. Drugs salbutamol, levosalbutamol and theophylline + etophylline FDC were prescribed in lesser doses while formoterol +budesonide FDC was overprescribed.
There was male preponderance 175 (97.2%) in our study similar to the meta-analysis of population-based epidemiologic studies conducted to calculate gender specific global prevalence of COPD which concluded that the overall prevalence of COPD was higher in males i.e., 9.24% and 6.15% in females, respectively and when analysis was limited to populations with age cut off above 40 years, the prevalence was around 11.57% and 7.44%, for males and females respectively [9].
The mean age of the participants was 65±8.37 years. Similar finding was noted in a study conducted in Spain by Miravitlles M et al.,where a total of 4,574 COPD patients were included and the mean age of the population was 67.1 years [10]. Similarly, it was noted in a study conducted in India by Gupta A et al., majority i.e., 47 /60 (78.3%) COPD patients fell in the age category of> 51 years [11].
In the current study hypertension (22.8%) was the most common comorbidity seen. The possible mechanism that links the two is the systemic inflammatory response triggered by cigarette smoke or air pollution [12,13]. Similarly in a study done in Southwest Iran by Kiani FZ et al., hypertension was seen in 30.2% of the COPD cases [14].
In the drug treatment awareness questionnaire 52.8% participants scored more than 50% thus indicating that nearly 47% patients lacked sufficient drug treatment awareness. To avoid this, physicians must ask the patients to reiterate the medication names even in cases where patients may claim that they know about the names of medications. It is important for the patients to know about the names of their medication to avoid dispensing errors at the level of pharmacist. If the patients know about their medication names, they can themselves verify the same when the pharmacist is dispensing the medications [15].
Some studies assessing inhaler use technique in India also showed lesser compliance to inhaler use techniques. Study done in Haryana by Gupta A et al., showed that out of 60 COPD patients only 36% of the patients were compliant to the use of inhaler at the first visit [11] while a study done in Jaipur by Sehajpal Ret al., showed that correct inhaler use technique was observed only in 18 (21.17%) patients [17].
Knowledge about possible undesired effects of the prescribed drugs is of paramount importance as it will help patients identify them and bring it to the notice of the prescribing clinician who can then take further action. A study done in Gujarat by Joshi et al., showed that 78.6% patients were aware that medicines can cause ADRs but none of the respondents were aware of ADR reporting centre and 86.7% agreed to report ADR in the future [18].
According to Centres for Disease Control and Prevention patients with higher education have mortality rates less than half of those without lesser educationprobably due to their better understanding of disease and its treatment.
In COPD despite advancement of medical treatment, nonadherence to medication poses an important opposition to the disease management with an average reported adherenceof 40%–60% in COPD patients [19]. In this study we found that 73.3% (132 participants out of 180) of the participants were able to score more than 50% (i.e., >3 out of 6), in the drug treatment adherence questionnaire with a mean score of 4.71 out of a total score of 6. Thus, we can see that the adherence is satisfactory. A study assessing medication adherence in COPD patients done in Haryana by Gupta A et al., saw a 74% compliance to medications [11].
A systematic review done by Van Boven J et al., showed that non-adherence in COPD showed a clear association with increase in hospitalizations and mortality, worsening in quality of life and loss of productivity [20]. The presence of comorbidities increases the number of medications that the participants have to consume on a daily basis thus making it more complex to adhere to treatment leading to the decrease in adherence to medication with presence of comorbid conditions [20].
Considering the lack of studies pertaining to COPD prescription patterns in western India, there was a need to find the same in western India region [21-23].
Prescriptions of the last 3 months were also analysed for any changes with respect to the current visit prescription. Hence, at the end of the study, 223 prescriptions were obtained for analysis from the 180 participants that were enrolled in the study.
In our study the average number of drugs per encounter was found to be 4.04±1.1 (Mean ± SD). Contrary to this in a study done in India by Sawant MP et al., the average numbers of drugs / prescription in COPD patients admitted to medicine in patient department was 7 [24]. This, may be because the patients were admitted as severe cases warranting more drugs to be prescribed.
In this study it was seen that majority of the drugs were prescribed with their generic name (i.e., 77.6 %). Our study found that 62.5% of the drugs were available in the national essential drugs list and 50% of the drugs were available in the WHO essential drugs list.
The most common drug prescribed was tiotropium bromide inhaler (i.e., 100%). Similar finding was seen in a study done in Kerala by Unni Aet al., in which it was seen that in COPD patients (n=237) the most commonly prescribed drugs were ipratropium (91.6%) followed by levosalbutamol (88.2%) [22]. In another study done in Karnataka by Udaykumar Pet al., it was seen that tiotropium was prescribed in 73/80 patients [25]. In low-income countries because of its low cost and easy accessibility this bronchodilator FDC is commonly prescribed it may be prescribed as an alternative in the absence of other bronchodilators [26] and the cases that come to a tertiary care hospital are mostly referral cases in whom methylxanthines are usually started previously as they might have received treatment from primary health centers where availability of other drugs is lower. This is in accordance with the WHO’s Prevention and Control of Noncommunicable Diseases: Guidelines for primary health care in low resource settings [27], hence when patients are referred to tertiary care hospital these drugs are not abruptly stopped but instead continued with lowering of the dose with time.
Limitations: Awareness for non-pharmacological treatment (chest physiotherapy) was not assessed. Patient perceived adherence was calculated and not the actual drug adherence.
Conclusion
COPD patients were aware of the drug regimen, inhaler use technique but awareness regarding drug name, adverse effects was poor. Similarly, awareness about inhaler uses technique steps of breath holding and mouth gargling was lacking. More than 2/3rd of the participants had a perceived drug adherence score more than 50% with mean score of 4.71 out of 6. Most prescribed drug in the prescriptions was inhalational tiotropium bromide and FDC was Theophylline + etophylline. Drugs salbutamol, levosalbutamol and theophylline + etophylline FDC were prescribed in lesser doses while formoterol +budesonide FDC was overdosed.
References
- https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease.
- Hossain MM, Sultana A, Purohit N. Burden of Chronic Obstructive Pulmonary Disease in India: Status, Practices and Prevention. Mini Rev Int J Pul Res Sci, 2018; 2(5): 3–6.
- Lindenfeld J, Jessup M. ‘Drugs don't work in patients who don't take them’ (C. Everett Koop, MD, US Surgeon General, 1985). European Journal of Heart Failure, 2017; 19(11): 1412-1413.
- Van Haarst A, McGarvey L, Paglialunga S. Review of Drug Development Guidance to Treat Chronic Obstructive Pulmonary Disease: US and EU Perspectives. Clin Pharmacol Ther, 2019; 106(6): 1222-1235.
- Jarab AS, Mukattash TL. Exploring variables associated with medication non-adherence in patients with COPD. International Journal of Clinical Pharmacy, 2019; 41(5): 1202-1209.
- Neupane S, Thapa P, Giri A. Factors Associated with Adherence to Medication among Chronic Obstructive Pulmonary Disease Patients in Tertiary Care Hospital of Nepal: A Cross-Sectional Study”, Journal of Pharmaceutical Research International, 2020; 20: 136–144.
- National Ethical Guidelines for Biomedical and Health Research Involving Human Participants. Indian Council of Medical Research, 2017.
- E6(R2) Good Clinical Practice: Integrated Addendum to ICH E6(R1) Guidance for Industry. 2018.
- Ntritsos G, Franek J, Belbasis L, Christou M, Markozannes G, Altman P, et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. International Journal of Chronic Obstructive Pulmonary Disease, 2018; 13: 1507-1514.
- Sufyan Ibrahim, Mohan K Manu, Beulah Sarah James. Health Related Quality of Life among patients with Chronic Obstructive Pulmonary Disease at a tertiary care teaching hospital in southern India. Clinical Epidemiology and Global Health, 2021; 10: 2213-3984.
- Faheemuddin MD, Ramaiah B, Kiran SS. Evaluation of Medication Adherence in COPD patients and their Drug Utilization Pattern. Chron Obstruct Pulmon, 2016; 1(17): 2572-5548.
- Grigsby M, Siddharthan T, Chowdhury M, Siddiquee A, Rubinstein A, Sobrino E, et al. Socioeconomic status and COPD among low- and middle-income countries. International Journal of Chronic Obstructive Pulmonary Disease, 2016; 11(1): 2497-2507.
- Kocabas A, Ozyilmaz E. The effects of socioeconomic status on health outcomes in patients with COPD. 52 Monitoring Airway Disease, 2016; 48(60).
- Kiani F, Ahmadi A. Prevalence of different comorbidities in chronic obstructive pulmonary disease among Shahrekord PERSIAN cohort study in southwest Iran. Scientific Reports, 2021; 11(1): 1-8.
- Rasool Muhammad Fawad, Rehman Anees ur, Imran Imran, Risk Factors Associated with Medication Errors Among Patients Suffering From Chronic Disorders, Frontiers in Public Health, 2020; 8; 2296-2565.
- The importance of good inhaler technique [Internet]. Let's Talk Respiratory, 2021.
- Shrinath V, Thatikonda A, Pandey I. A cross sectional observational study on uncontrolled bronchial asthma and inhaler technique among out patients in a tertiary care centre in Western Maharashtra. Lung India, 2023; 5: 440-444.
- Joshi A, Shah N, Mistry M, Gor A. Evaluation of knowledge and perception toward adverse drug reactions among patients visiting tertiary-care teaching hospital. National Journal of Physiology, Pharmacy and Pharmacology, 2015; 5(4): 280-284.
- Philip A, Mohanan M, Shine M, Benny S, Ashok P. Assessment of Medication Adherence Barriers in COPD Patients in A Secondary Care Teaching Hospital. JDDT, 2020; 10(2-s): 80-85.
- Evalyne M, Jansen dSusanne J, van de Hei Boudewijn. Global burden of medication non-adherence in chronic obstructive pulmonary disease (COPD) and asthma: a narrative review of the clinical and economic case for smart inhalers. Journal of Thoracic Disease, 2021; 13: 2077-6624.
- Vikneshwari Mani T. Drug utilization pattern in chronic obstructive pulmonary disease in a tertiary care teaching hospital. Indo American Journal of Pharmaceutical Research, 2016; 6(7): pp.6258-6264.
- Shiv Kumar G, Madhuri Anju Wilson, Tigi S George. Study of Prescribing Pattern of Drugs in Chronic Obstructive Pulmonary Disease in Tertiary Care Teaching Hospital, Indian Journal of Pharmacy Practice, 2019; 12: 161-166.
- Hadia Rajesh, Bhatt Priyesha, Panchal Anadisharan, Gandhi. An Observational Study on Drug Utilization Pattern in Asthma and ChronicObstructive Pulmonary Disease in Tertiary Care Teaching Hospital. Journal of Pharmaceutical Research International, 2021; 10: 187-198.
- Sawant M, Padwal S, Kale A, Pise H, Shinde R. Study of drug prescription pattern among COPD patients admitted to medicine in-patient department of tertiary care hospital. International Journal of Basic & Clinical Pharmacology, 2017; 6(9): 2228-2232.
- Udaykumar P, Farangipete F. Are our patients with acute exacerbation of chronic obstructive pulmonary disease adequately treated? Are we in line with gold guidelines? J Basic Clin Pharma, 2017; 8: 1–10.
- UR Rehman A, Hassali M, Abbas S, Ali I, Harun S, Muneswarao J, et al. Pharmacological and non-pharmacological management of COPD; limitations and future prospects: a review of current literature. Journal of Public Health, 2019; 28(4): 357-366.
- Diana R, Tamondong-Lachica, Neil Skolnik, John R Hurst. GOLD 2023 Update: Implications for Clinical Practice. International Journal of Chronic Obstructive Pulmonary Disease, 2023; 18: 745-754.

