Squamous Cell Carcinoma of the Lips: About 29 Cases
Opango ADC*, Nshimirimana B, Nini K, Aziz Z, El Bouihi M and Mansouri-Hattab N
Stomatology and maxillofacial surgery department, Mohammed VI University Hospital, Marrakech, Morocco
Received Date: 30/10/2024; Published Date: 12/11/2024
*Corresponding author: Opango ADC, Stomatology and maxillofacial surgery department, Mohammed VI University Hospital, Marrakech, Morocco
Summary
Squamous cell carcinomas are the most common cancers of the oral cavity. Lip squamous cell carcinomas are common in our context. Patients consult late, complicating care. We report a series of 29 cases of squamous cell carcinoma of the lips treated in the stomatology and maxillofacial surgery department of the Mohammed VI University Hospital, Marrakech (Morocco).
The average age was 61.3 years, with a male predominance. Patients consulted on average after 9 months. The lower lip was the most affected (55.1%). The majority of patients were classified as AJCC stage IV A. Treatment generally combined tumor excision with lymph node dissection and reconstruction, associated with adjuvant radiotherapy. Survival was 75% at 25 months.
The management of squamous cell carcinoma of the lips in our context constitutes a real challenge, given the advanced stage of the tumor at the time of diagnosis.
Keywords : Squamous cell carcinoma; Lip; Cancer; Surgery; Radiotherapy
Introduction
Squamous cell carcinomas represent 90% of cancers of the oral cavity and upper aerodigestive tract. It is a cancer with aggressive progression potential, requiring early diagnosis and treatment. Squamous cell carcinomas of the lips are not uncommon. In our context, patients often consult late. The aim of our work is to show our approach to the management of patients with squamous cell carcinoma of the lips.
We report a series of 29 patients treated for squamous cell carcinoma of the lips in the stomatology and maxillofacial surgery department of the Mohammed VI University Hospital in Marrakech (Morocco).
Series
The average age of patients was 61.3 years, with a peak between 60-70 years. There was a clear male predominance with a sex ratio of 2.2. Patients consulted an average of 9.3 months after the onset of symptoms. The main risk factors noted were alcohol and tobacco poisoning in 58.6% of cases, poor oral hygiene in 82.7% of cases. A leukoplakia type precursor lesion was observed in 7 cases (24.1%), no case of erythroplasia was noted.
Squamous cell carcinoma was located at the level of the lower lip in 55.1% of cases, at the level of the upper lip in 13.8% of cases, at a lip corner in 6.9% of cases, and the lesion concerned the 2 lips in 24.2% of cases. All patients underwent a biopsy with histopathological examination which confirmed the diagnosis of squamous cell carcinoma. It was a conventional squamous cell carcinoma in 89.6% of cases and a verrucous squamous cell carcinoma in 11.4% of cases.
A loco-regional and remote extension assessment comprising a cervico-facial CT scan, a thoraco-abdominopelvic CT scan, and an orthopantomogram was systematically performed. At the end of this extension assessment, 75.9% of our patients were classified as AJCC stage IV A, 10.3% in stage II, 10.3% in stage III.
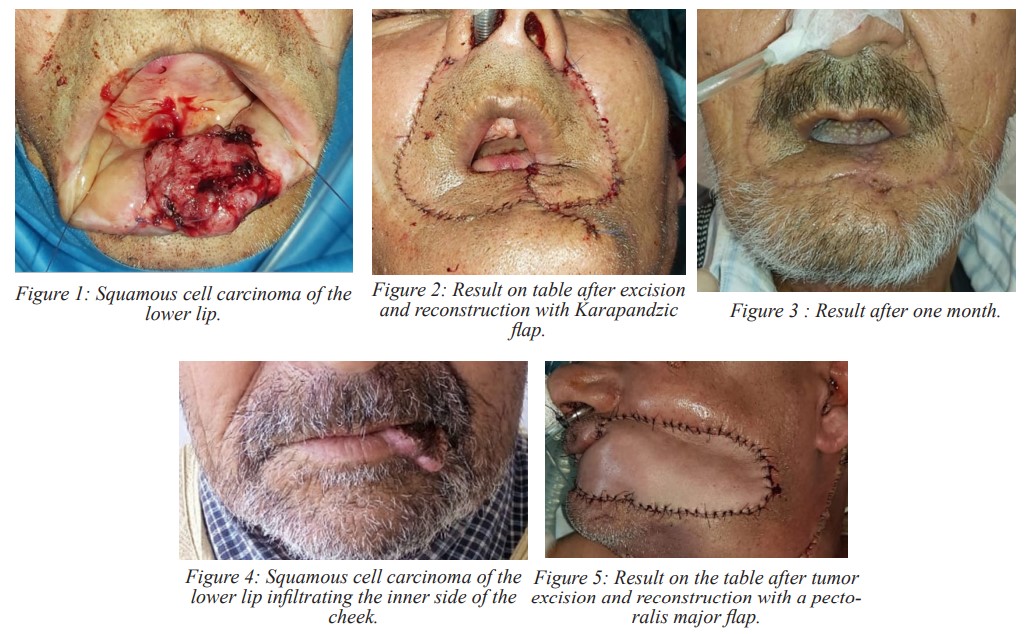
After a multidisciplinary consultation meeting, 28 patients initially benefited from surgical treatment, one patient was referred to oncology due to the significant extension of the tumor. Surgical treatment consisted of tumor excision with safety margins of 1 cm associated with unilateral or bilateral cervical lymph node removal. Associated procedures were performed: interruptive mandibular resection with immediate maxiplate reconstruction in 3 cases, hemi-maxillectomy in 3 cases. A reconstruction of the substance losses resulting from tumor excision was made, often justifying the use of loco-regional flaps: Karapandzic flap (53.6%) (Figure 1 and 2), Webster flap (17.8%). %), pectoralis major flap (10.1%) (Figure 3 and 4), Dufourmentel flap (3.5%).
All patients received adjuvant radiotherapy at the surgical site and lymph node areas.
The average follow-up duration was 25 months. We noted: 3 cases of tumor recurrence on healthy excision margins, occurring 11 months later, they benefited from surgical revision; 7 cases of death.
Overall survival within the duration of follow-up was 75%.
Discussion
Squamous cell carcinomas are serious cancers, due to their local infiltration but also their possibility of metastasizing distantly. They represent 90% of oral cavity cancers [1]. The main risk factors for the occurrence of squamous cell carcinoma are alcohol and tobacco consumption. The combination of the 2 having a synergistic effect [2-4]. Other factors have been described: poor oral hygiene, viral infections (HPV), immunosuppression (HIV AIDS), certain genetic pathologies (xeroderma pigmentosum). Precancerous lesions are known: leukoplakia and erythroplasia. Leukoplakia is common but less likely to develop into squamous cell carcinoma. Erythroplasia is less common but at high risk of transformation into squamous cell carcinoma [5,6].
Lip cancer is a typical malignancy that accounts for 25-30% of all oral cancers [7]. Oral and lip cancer is a major global health problem [8]. The warning sign on the lip is generally an ulceration or a budding ulcerative lesion which justifies consultation [9]. The diagnosis is based on the histological analysis of a biopsy which confirms the diagnosis and specifies the histological subtype. A radiological assessment makes it possible to evaluate the loco-regional (CT or cervico-facial MRI) and distant (thoraco-abdomino-pelvic CT) extension in search of distant metastases [10,11]. At the end of this extension assessment, the patient is classified according to the TNM classification of the AJCC and UICC [12]. The treatment will depend on this classification, which will be discussed in a multidisciplinary consultation meeting in order to propose a personal treatment plan.
The majority of our patients were classified stage IV A. This is explained by the delay in consultation. The therapeutic protocol at this stage includes surgical resection of the tumor, cervical lymph node dissection, reconstruction of the defect and postoperative radiotherapy. Surgical resection requires safety margins of 1cm in order to be carcinological [13]. When the tumor infiltrates the underlying bony structures (mandible or maxilla), bone resection is necessary (non-interrupting or interrupting mandibular resection, maxillectomy) depending on the extent of the infiltration. We did not use the Mohs technique.
We used selective lymph node dissection involving lymph node areas I, II and III. Cervical lymphadenectomy in the form of elective neck dissection offers improved overall and disease-free survival compared with therapeutic neck dissection for the majority of oral cancers with recent evidence suggesting advantages even for tumors less than 4 mm in thickness [14]. We did not use the sentinel lymph node technique.
Reconstruction options include local flaps, regional pedicled flaps, and microvascular free tissue transfer [15]. Hard tissues can be reconstructed using free autologous bone grafts (iliac bone, fibula), but also involve the use of free tissue transfer from the iliac crest, fibula, radius or scapula.
Adjuvant radiotherapy improves local control and overall survival in advanced tumors. It should be considered in all patients with larger T3 or T4 tumors, or N2-3 neck disease. The morbidity of radiotherapy to the primary site of the oral cavity means that the benefits and side effects must be carefully considered for each patient.
The 5-year overall survival of squamous cell carcinoma of the lips is estimated at 40-50% [13].
Conclusion
This case highlights the severe implications of Lemierre syndrome following tonsillitis and underscores the significance of subclavian DVT as a complication. Early diagnosis and intervention are essential for improving outcomes, especially in young, healthy patients with post-oropharyngeal infection symptoms. Increasing clinician awareness of Lemierre syndrome, its diagnostic challenges, and complications may prevent delays in care and reduce morbidity associated with this rare but dangerous condition.
References
- Pablo H. Montero, Snehal G. Patel. Oral cavity cancer. Surg Oncol Clin N Am, 2015; 24(3): 491-508.
- Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Research against cancer, 1988; 48(11): 3282-3287.
- McCoy GD, Wynder EL. Etiological and preventive implications in alcoholic carcinogenesis. Research against cancer, 1979; 39(7 Part 2): 2844-2850.
- Brugère J, Guenel P, Leclerc A, et al. Differential effects of tobacco and alcohol on laryngeal, pharyngeal and oral cancer. Cancer, 1986; 57(2): 391-395.
- Warnakulasuriya S, Johnson NW, van der Waal I. Nomenclature and classification of potentially malignant disorders of the oral mucosa. Journal of oral pathology & medicine: official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology, 2007; 36(10): 575-580.
- Neville BW, day TA. Oral cancer and precancerous lesions. CA: a cancer journal for clinicians, 2002; 52(4): 195-215.
- Maruccia M, Onesti MG, Parisi P, Cigna E, Scuderi N. Lip cancer: a 10-year retrospective epidemiological study. Anticancer research, 2012; 32(4): 1543-1546.
- Siakholak FR, Ghoncheh M, Pakzad R, Gandomani HS, Ghorat F, Salehiniya H. Epidemiology, incidence and mor- tality of oral cavity and lip cancer and their relationship with human development index worldwide. Bio-medical research and therapy, 2016; 3(10): 872-888.
- Rethman MP, Carpenter W, Cohen EE, Epstein J, Evans CA, Flaitz CM, et al. Evidence-based clinical rec-ommendations for screening for oral squamous cell carcinoma. J Am Dent Assoc, 2010; 141: 509-520.
- De Bree R, Prend RP, Castelijns JA, Medina JE, Stoeckli SJ, Mancuso AA, et al. Advances in diagnostic mo-dalities to detect occult lymph node metastases in squamous cell carcinoma of the head and neck. Neck head, 2015; 37: 1829-1839.
- Liao LJ, Lo WC, Hsu WL, Wang CT, Lai MS. Detection of cervical lymph node metastases in head and neck cancer patients with clinically N0 neck: a meta-analysis comparing different imaging modalities. Cancer BMC, 2012; 12: 236.
- Lacheretz-Szablewski V, Garrel R, Guillot C, Costes-Martineau V. Oral cavity tumors and TNM classification (8th edition): issues and recommendations.Annals of Pathology, 2023; 43(4): Pages 289-297.
- Kerawala C, Roques T, Jeannon Jp, Bisase B. Oral cavity and lip cancer: UK national multidisciplinary guide-lines. The Journal of Laryngology and Otology, 2016; 130(Supp.S2): S83-S89.
- D'Cruz AK, Vaish R, Kapre N, Dandekar M, Gupta S, Hawaldar R. Elective versus therapeutic neck dissection in node-negative oral cancer. N Engl J Med, 2015; 373: 521–529.
- Ragbir M, Brown J, Mehanna H. Reconstructive con- siderations in head and neck surgical oncology: UK national multidisciplinary guidelines.J Laryngol Otol, 2016; 130(Supplement S2): S191–197.

