Valentino’s Syndrome
Abdelilah El Bakouri, Zarhouni baallal malik*, Majda El mkhalet, Mounir Bouali and Khalid Elhattabi
Visceral surgical emergency department, Ibn Rochd University Hospital, Hassane II University, Faculty of Medicine and Pharmacy (FMPC), Casablanca, Morocco
Received Date: 15/10/2024; Published Date: 08/11/2024
*Corresponding author: Zarhouni Baallal Malik, Department of Visceral Surgery, Ibn Rochd University Hospital, Hassane II University, Faculty of Medicine and Pharmacy (FMPC), Casablanca, Morocco
Introduction
Valentino’s syndrome involves the presentation of a perforated peptic ulcer. The chemical fluid from the ulcer streams along the right paracolic gutter to the right iliac fossa, causing peritoneal irritation and consequent chemical appendicitis [1].
This case report describes a patient who presented to our institution with generalized abdominal discomfort accompanied by low-grade fever and vomiting. The study will also delineate the management course and associated literature.
Case Presentation
A 26-year-old man, chronic smoker at 10 packs/year, consulted for generalized abdominal pain, starting in the right iliac fossa associated with vomiting. Abdominal examination reveals generalized abdominal guarding; rectal examination is normal. his white blood cells were at 18,430 and the C-reactive protein was at 33. The chest radiograph revealed A pneumoperitoneum.
An explorative laparotomy was imminent. Following a midline abdominal incision, the exploration showed a peritoneal effusion of medium abundance made of purulent liquid with false membranes in the subhepatic and inter-loops and at the level of the right iliac fossa, then we found a pre-pyloric perforation of 01 cm on the pyloric antrum at the anterior region and an inflamed curled appendix perforated at the level of its tip with a healthy base in an internal laterocal position.
An appendicectomy was made and the perforation was closed using two Vicryl 2/0 sutures reinforced by omentum. The rest of the peritoneal cavity was irrigated using warm normal saline
The postoperative period was smooth and uneventful. The patient was kept on IV fluids, IV antibiotics, and IPP. Nasogastric tube was removed on the third postoperative day.
The patient made a full recovery and was released five days after surgery.
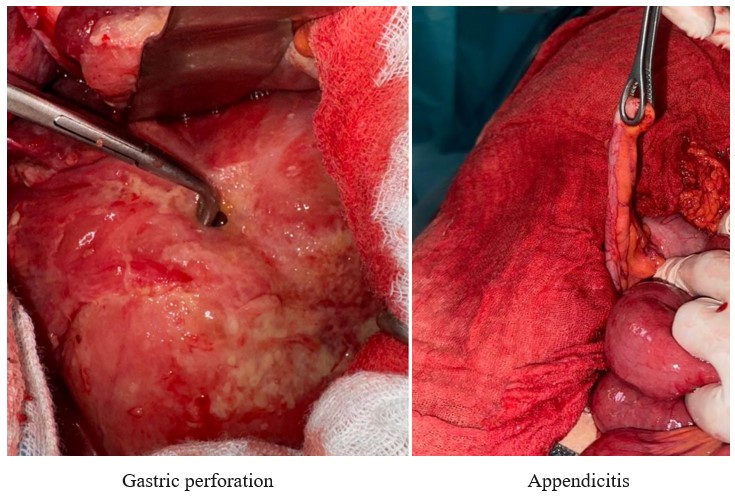
Figure: Surgical specimen-thyroid.
Discussion
Valentino's syndrome, named for the popular silent film actor Rudolph Valentino, was first described after he developed the signs and symptoms of appendicitis and underwent an appendectomy that failed to relieve his symptoms. He later developed overt peritonitis and developed multi-organ failure, to which he later succumbed. During his autopsy, it was discovered that he had been suffering from a perforated peptic ulcer [2].
By now, it has become a known fact that there are many conditions apart from VS that can present clinically similar to appendicitis and should be considered in the differential diagnosis before and during the operation [3].
After perforation of the duodenal ulcer, inflammatory fluid and alimentary tract contents seeped into the abdomen and trickled down the right colic gutter. As the purulent fluid remained in the abdomen, it caused peritonitis and referred pain from the same general area as the appendix, leading to the development of signs and symptoms mimicking acute appendicitis. Although the ulcer was not visualized endoscopically, vigilant gross examination of the duodenum led to identification of a pinhole perforation and diagnosis of Valentino's syndrome [2].
Peptic ulcers are caused by a combination of defensive factors (e.g., mucus-bicarbonate layer and prostaglandins) that protect the mucosa and aggravating factors (e.g., hydrochloric acid) that cause mucosa necrosis. Peptic ulcers can be caused by a number of factors, the most common of which is the overuse of NSAIDs, which inhibit COX and prostaglandin synthesis [3,5]. Furthermore, stress, irregular or unhealthy eating habits, H. pylori infections, and rare cases such as Crohn’s disease, Zollinger Elision syndrome, and Cushing’s syndrome or complications of malignancy, chemotherapy, or radiotherapy can all lead to peptic ulcer formation [4].
The presence of pneumoperitoneum is often formed by the intraperitoneal perforation of the stomach or first part of the duodenum, whereas pneumo-retroperitoneum (typical in the right kidney, ‘veiled right kidney sign’) is caused by a retroperitoneal perforation. The most reliable sign of appendicitis frequently manifests as epigastric or periumbilical pain that progressed to the RLQ [1].
On an erect chest X-ray, free peritoneal air may be identified as the air under the diaphragm. In ultrasonography or intraoperatively, a fluid collection is encircling the appendix as the gastric fluid courses through the right paracolic gutter into the right iliac fossa. In the context of acute appendicitis with epigastric pain, a CT scan is the suggested imaging investigation for the diagnosis of Valentino’s syndrome [5].
Conclusion
Valentino's syndrome is an uncommon cause of right lower quadrant pain and symptoms mimicking acute appendicitis. In our case it was a general abdominal pain that lead us to perform a midline incision in the first place.
Our aim is to increase the awareness of this condition, as a high degree of suspicion is essential in its preoperative diagnosis and the preoperative diagnosis may reduce patient morbidity and mortality.
References
- Machaku D, Suleman M, Mduma E, Nkoronko M, et al. Valentino’s syndrome: a bizarre clinical presentation. Surg. Case Rep., 2023; no 2: p. rjad035. doi: 10.1093/jscr/rjad035.
- A Case of Valentino’s Syndrome Presenting as Possible Appendicitis | International Surgery,
- Jaboury IA. Valentino syndrome: case report and review of literature. ANZ J. Surg., 2020; 90(no 5): p. 940‑ doi: 10.1111/ans.15883.
- Mahajan PS, et al. A Cautionary Tale: Unveiling Valentino’s Syndrome. Cureus, 2022; 14(no2). doi: 10.7759/cureus.22667.
- Mahajan PS, Abdalla MF, Purayil NK, et al. First Report of Preoperative Imaging. J. Clin. Imaging Sci., 2014; 4: no 2.

