COVID 19 or Cytarabine Sinusoidal Obstruction Syndrome’s Case Report
Latifa Khelifa*
Department of Hematology, Hedi Chaker Hospital Sfax, Tunisia
Received Date: 19/07/2024; Published Date: 08/11/2024
*Corresponding author: Latifa Khelifa, Department of Hematology, Hedi Chaker Hospital Sfax, Tunisia
Abstract
AML is a malignancy occurring in adult and mostly in aged person, with the COVID pandemia, we are more convinced of the need of new molecule less intensive and less toxic to treat such life-threatening pathology and to avoid dangerous complications.
Introduction
Veino Occlusive Disease (VOD) or recently known as sinusoidal obstruction syndrome (SOS) is characterized by injury of the sinusoidal wall integrity with subsequent sinusoidal blockage by embolized sinusoidal lining cells. Impaired sinusoidal microcirculation leads to metabolic dysfunction and ischemic damage of adjacent liver cell plates and further hepatocellular necrosis/ dropout [1,2].VOD/ SOS is responsible for a considerable morbidity and mortality in it’s severe to very severe grade (mortality exceed 80% with multiorgan Failure disease) [3] and could however, with mild to moderate form resolve progressively [4]. VOD/ SOS is well described after allogenic Human Stem Cell Transplant (HSCT) with an incidence varying from 5% to 15% [4,5]. Other causes were less studied [6] and the VOD/SOS diagnosis in no graft patients was rarely considered which could delay proper health care. Indeed, with the deployment of new drugs such as monoclonal antibodies that convey toxins, the appearance of VOD/SOS due to treatments other than allografts has taken on all the interest [7]. On the other hand, with the emergence of the pandemic of COVID attention has shifted to studying its effect on the liver. Especially that In 2003, in the SARS-CoV epidemic, approximately 60% of patients developed liver damage, and phylogenetic similarities suggested the possibility of the SARS-CoV-2 aggression on the liver [8].We present here a real clinical and histological proven case of VOD/SOS in the context of COVID infection following chemotherapy. Drawing the reader's attention to such complications makes it possible to ensure appropriate early management and therapeutic improvement possibilities in the hope of ad integrum hepatic tissue recover.
Case Report
A 48 years old male was admitted to our department for acute myeloid leukemia.
He had no prior history of liver or systemic diseases, he did not use alcohol and he was not taking any medications or herbal substances.
At diagnosis, a COVID infection was discovered incidentally via PCR. The patient was afebrile, no jaundice nor hemorrhage nor tumor syndrome, he just complained from asthenia. His biological assessments showed leucocyte at 9670/mm3, anemia and thrombopenia with 28% of blasts on peripheral smear. Gamma glutamyl transferase (GGT) was elevated (4N). Immunologic and Serological tests for hepatitis B, C, VIH and EBV were negative.
Ones he has negatived his COVID-19 PCR, the patient received AML induction (3+7) therapy with 3 days of daunorubicin (60mg/m2/day) = 360 mg total dose and 7 days of cytarabine (200mg/m2/day) = 2800 mg total dose. On day 28, He was in cytologic, cytogenetic and molecular remission.
Induction therapy was complicated on day+7 with symptomatic COVID infection by fever and curiously early deep pancytopenia with transfusion needs.
On 17th day of induction, the patient presented weight gain, jaundice, ascites, splenomegaly (21cm with ultrasound imagery) and lower limbs oedema. Biological assessments (Figure 1) revealed thrombopenia, hypoalbuminemia, elevated Gamma glutamyl transferase (GGT) level (6N) and bilirubin (130 µmol/l). Transaminases were normal. Prothrombin time (TP) was low (32%) with prolonged activated thromboplastin time (TCA). Factor V and VII of coagulation were low too. Immunologic and serological control tests for hepatitis B, C, VIH and EBV were both negative. Abdominal ultrasound showed portal hypertension with hepatomegaly and splenomegaly. The liver biopsy showed centrilobular thrombosis, sinusoidal dilatation and necrosis microfocus (Figure 2).
The diagnosis of veino occlusive disease was considered. Pharmacology analysis concluded: taking in consideration all the elements aroused and the severity of the disease (so severe prognosis: mortality of 17 to 80%), it is recommended for this patient, to contraindicate the subsequent use of aracytine and to change with another chemotherapy. It is also recommended to wait for clinical and biological recovery before administering another chemotherapy and to avoid other drugs strongly associated with this syndrome: such as busulfan, cyclophosphamide, oxaliplatin and any other hepatotoxic drug until recovery.
According to EBMT criteria (Figure 3) it was about a middle SOS complication form. The treatment was based on supportive care (diuretics, blood and platelet transfusion albumin perfusion and ursodeoxycholic acid intake).
After 2 months without further chemotherapy treatment the evolution was characterized by regression of ascites and lower limbs oedema. Prothrombin time was normal. Albuminemia level increased to 32 g/l. Bilirubinemia was in the upper normal limit, GGT level decreased to three times of the normal range but thrombopenia persist.
The clinical picture was intricate is it a complicated COVID infection? Or aracytine liver toxicity? Or liver damage to SARS-CoV-2 worsen by chemotherapy? Or vice versa?
faced to such malignant pathology (AML) with an unfortunate prognosis, the only way to overcome the imminent risk of relapse and the possibility of patient’s death was to resume treatment at lower doses with PCR COVID negative.
At day 86 induction, still in remission, we started consolidation at intermedium dose of Aracytine at low doses (200mg/m2) for five days only associated to Etoposide 100mg/m2. At the starting therapy he had no symptoms but by the day 12, he reactivated his VOD with edema, ascites and splenomegaly and laboratory tests reveal thrombopenia at 4000/mm3, a fall in Prothrombin Time to 48% and hypoalbuminemia at 23g/l but no cholestasis.
The patient was proposed for venetoclax- vidaza protocol. And recuperation ad integrum of his clinical and biological features occurred by five months later of the former episode.
Discussion
AML and protocol of treatment:
Myeloid malignancies represent 5% of all adult cancers [9,10]. Overall, AML is fatal for the majority of patients (=80%), and modern cooperative group studies show that patients younger than 55 to 60 years of age have only about 40% overall survival at 05 years [10,11]. Until very recently, the standard chemotherapy for AML remained largely unchanged for decades, and the survival improvements over time in younger patients were attributable mostly to better supportive care [10].
Already half century now, an intensive induction regimen of cytarabine and anthracycline (commonly called 7+3 regimen) was developed for the treatment of AML. After receiving induction chemotherapy, patients with favorable risk disease features (eg core binding factor (CBF) AML or NPM1 mutation without high allelic burden FLT3 internal tandem duplication (ITD) mutation) who achieve remission are generally recommended to continue with consolidative chemotherapy with HDAC based regimen [11].
Cytarabine or as known Aracytine (AraC) has been a major drug for acute myeloid leukemia (AML) treatment for decades. It was observed that high dose AraC(HDAC) maximizesanti-leukemia effect in AML patients, leading to improve disease free survive (DFS). HDAC instead of standard dose cytarabine multiagent chemotherapy has become a common practice in the treatment of AML especially in patients younger than 60 years of age in consolidation, based on guidelines of the NCCN [11,12].
AML and COVID 19:
In recent years, the whole world has been confronted with the COVID pandemic and scientific papers have wonderfully detailed its pathophysiology and its consequences [13]. It’s now obvious that COVID19 had a significantly more severe courses in patients with cancer (including admission to the intensive care unit, invasive ventilation or death) compared to non-cancer patients (p= 0,0003). However, only few comprehensive reviews provide an overview of the clinical features, prevention and treatment in this particular population. Most of the literature explicitly describing the clinical course of COVID 19 in adult AL patients’ is based on small case series and single case reports. Publications on the impact of COVID19 on AL treatment and recommendations for treatment modifications in patients with AL are scarce or mostly based on expert opinion. This gap of knowledge makes it difficult to establish the best therapeutic strategies for patients with AL and concomitant SARS-CO-2 infection [14].
In one of the most recent published studies authors report a cohort of 388 adult AML patients where the chemotherapeutic program was modified in 45% of patients with delay or discontinuation in 39% and 61% of cases respectively. Interestingly in this study authors showed that a treatment delay was protective in multivariate analysis for the clinical course of COVID 19, whereas therapy discontinuation if already started was associated with worse outcomes [15].
According to the current ASH and ECIL9 recommendations [14,16]. if possible starting intensive chemotherapy treatment should be delayed in case of SARS COV2 positivity until PCR negativity. Of note, the time of SARS COV2 clearance might be prolonged in AL patients for up to 82 days [17].
Despite the COVID 19 pandemic, consolidation therapy with cytarabine should be offered to patients in complete remission. High dose cytarabine should be reduced to 1,5g/m2 and reduction in the number of consolidation cycles should be considered. However, to avoid hospitalization and reduce transfusion frequencies in the case of local outbreaks or a shortage of beds and blood supplies, low dose therapy with azacytidine in combination with venetoclax may be considered as an alternative, especially in those patients with reduced performance status [16-18].
SOS/VOD
Epidemio
Hepatic veino occlusive disease/ sinusoidal obstruction syndrome (VOD/ SOS) is a potentially life-threatening complication. Primarily associated with hematopoietic stem cell transplantation (HSCT), and may occur in allogenic and autologous HSCT recipients. VOD/ SOS has also been increasingly recognized to occur as the consequence of high intensity chemotherapies in the non-transplant setting. The pathophysiology of VOD/ SOS is believed to involve an initial toxic injury to the sinusoidal endothelium that triggers activation of and damage to the endothelial cells, resulting in defenestration and gaps in the sinusoidal barrier [19].
The incidence of hepatic sinusoidal obstruction syndrome varies from 0 to 70% and is increasing. This wide range is attributable to the variation in patient’s characteristics, diverse criteria for diagnosis, small sample size, variable distribution of risk factors for HSOS in different series and variations in the conditioning immunosuppressive regimens used in each center [2,3,20].
At autopsy, 50% of patients with liver dysfunction who did not meet clinical diagnostic criteria of SOS had evidence of SOS lesion on histology. It is likely that some degree of sinusoidal injury occurs in most patient who receive liver toxic conditioning regimens, even in the absence of characteristic symptoms [2].
Pathophysiology:
Many factors are involved in the pathogenesis of HSOS. These include SEC glutathione depletion, nitric oxide depletion, increased matrix metalloproteinases, increased Vascular Endothelial Growth Factor (VEGF) and possibly the clotting factors. The drugs that cause HSOS are more toxic to the hepatic Sinusoidal Endothelial Cells (SECs) than to hepatocytes [3].
The lesion unit is an endothelial damage that allows the extra endothelial damage allows the extravascular deposition of red blood cells, leukocytes, and other debrides into the space of Disse, which may lead to a pathophysiological lining dissection downstream embolization, and occlusion of the microcirculation [21].
At microscopic level, the definitely emerging morphological features were characterized by diffuse alterations of intra hepatic vascular structures (portal branches and sinusoids) and variable degree of partial/ complete luminal thrombosis; CD34 decorated abnormally sinusoids in all lobar zones. Central veins did not show significant alteration of lumen caliber and of wall configuration. Majority of portal fields showed an increased number of portal veins associated with luminal severe dilatation and wall fibrosis, in a large number of portals veins the lumen focally herniated in peripheral liver parenchyma and completely circumscribed by liver cells plates. Kupffer cells were found extremely activated with large cytoplasm containing necrotic debrides [22].
Diagnosis:
Clinical picture
According to the Seattle criteria, for the diagnosis of hepatic VOD two of the three diagnostic clinical manifestations (jaundice, painful hepatomegaly, and fluid retention) must be present by day 20 after bone marrow transplantation. According to the modified Settle criteria that were developed by Mc Donald et al, two of the following three should be present in order to diagnose hepatic VOD; hyperbilirubinemia, hepatomegaly or right upper quadrant pain of liver origin, or unexplained weight gain> 2% of the baseline body weight. Similarly, according to the Baltimore criteria hepatic VOD is diagnosed when there is jaundice (bilirubin>2mg/dl) and two of the following three criteria: hepatomegaly (usually painful); ascites; or >5% weight gain. Neither the Seattle nor the Baltimore criteria consider documentation of abnormal hepatic blood flow as required for diagnosis of VOD, since the obstruction affects only small intrahepatic veins [23].
Increases in spleen size correlate with increasing grade of hepatic sinusoidal injury and can serve as a simple method for identifying patients at risk for this toxicity. Increases in spleen size is recognized as a potential etiology of persistent VOD/ SOS related thrombocytopenia [24].
Splenomegaly and thrombocytopenia have been shown to correlate with the number of cycles of chemotherapy administered, but no direct relationship has been established between the dose of administered chemotherapy and severity of VOD/SOS [2].
Clinically, It should be noted that the diagnosis of HSOS can be difficult to establish especially when only one clinical criterion is present, the timing of events is unusual, or there are clinical data suggesting another cause(3)
Biomarkers/ biology:
High serum bilirubin level is a sensitive index of HSOS, but is nonspecific as it may also be indicative of a number of other disorders in the transplant setting. Serum (ASAT) levels> 750UI/l indicates poor prognosis.
Diverse biomarkers for potential prediction and early detection of VOD/ SOS have been proposed, which may prove useful, although they are not yet widely accepted. Of these, increased plasminogen activator inhibitor 1 antigen level is perhaps, the most well studied and supported.
Also, early cases of HSOS showed elevated serum levels of procollagen III, or its N-terminal propeptide (P-III-P) even before the appearance of any clinical or laboratory sign, and can be considered as an early marker for HSOS in children. P-III-P values in adults are probably useful in predicting and monitoring the clinical course of HSOS [3,7].
Indeed, some researches have suggested using a panel of associated and interactive biomarkers, rather than just 1 or 2, for risk prediction. Biomarkers of VOD/ SOS have been identified for both the HSCT setting and for risks associated with primary chemotherapies, such as oxaliplatin [21].
Other explorations:
Researchers have also investigated the potential for various biomarkers to constitute reliable diagnostic criteria for VOD/ SOS, as well as indicators of risk. From a hematologic perspective; thromboelastography is a functional assay that can assess the balance of procoagulant and anticoagulant proteins in blood vessels, and thus determine the risk for thrombosis leading to SOS/ VOD [21].
Novel hepatic diagnostic criteria for VOD/ SOS that have been investigated include liver stiffness, measured with ultrasound or acoustic radiation force impulse shear wave elastography, as an indication of veinous congestion and fibrosis [21,25].
MRI has recently demonstrated patent hepatic veins and patchy signal enhancement compatible with sinusoidal congestion in two patients with HSOS [3].
Etiologies:
BMT related VOD/ SOS as well-known etiology and best documented cause in the literature. The incidence of SOS/ VOD reported in the contemporary literature ranges from 10 to 20% after allogenic HSCT using MA conditioning (and has a higher as 60% in a subset of pediatric patients) [5,25,26].
Aggressive chemotherapy is usually applied to eradicate cancer. This may explain the higher risk of HSOS in patients with malignancies. Other risk factors include metabolism individual variability and some virus infection was also reported as HCV, CMV [3].
Our case detailed the occurrence of VOD/ SOS in non-transplanted AML associated to COVID infection. A focus on these two circumstances, means chemotherapy for AML treatment and COVID infection, their role in VOD/ SOS is well documented.
COVID and VOD
Histological study shows pictures compatible with vascular alterationswere characterized by diffuse lesions of intra hepatic vascular structures (portal branches and sinusoids) and variable degree of partial/ complete luminal thrombosis; CD34 decorated abnormally sinusoids in all lobar zones. Central veins did not show significant alteration of lumen caliber and of wall configuration. Majority of portal fields showed an increased number of portal veins associated with luminal severe dilatation and wall fibrosis, in a large number of portals veins the lumen focally herniated in peripheral liver parenchyma and completely circumscribed by liver cells plates. Kupffer cells were found extremely activated with large cytoplasm containing necrotic debrides [22,27].
At the molecular level, p38 MAPK pathway may also be critical in promoting vaso constrictive and inflammatory phenomena, its activation is described in SCD, COVID 19 and also as a result of conditioning regimen included endothelial damage in BMT [28].
In fine, post BMT syndromes, vaso occlusive organ dysfunction in SCD and COVID 19 associated endothelitiis share common pathological mechanisms including:
- Dysregulation of homeostasis of the endothelial milieu toward a pro inflammatory and prothrombotic phenotype with thrombotic microangiopathy
- Hyperproduction of inflammatory cytokines such as IL6, IL8 AND TNFa
- Small vessel endothelitis and endothelial barrier dysfunction, leading to oedema of the microvascular bed, protein and fibrin accumulation and subsequent fibrotic shift
All these conditions if untreated irremediably lead to MOF and display similar microscopic and macroscopic features in target organs upon pathological examination [28].
VOD drug induced
Risks of VOD/ SOS outside of HSCT setting have become more broadly recognized in recent years. For example, of 1137 patients enrolled in the expanded access (T-IND) study who developed VOD/ SOS and were treated with defibrotide, 137 (12%) had SOS/ VOD associated with primary chemotherapy (non HSCT related). The most commonly administered chemotherapeutic agents were cyclophosphamide (53,7%), cytarabine (51,2%), vincristine (47,6%), methotrexate (34,1%) and thioguanine (30,5%). Gemtuzumab Ozogamicin (GO) was used in 2 patients including 1 patient with MOD [6].
SOS is caused by toxic injuries to SECs and loss of sinusoidal wall integrity with subsequent sinusoidal blockage by embolized sinusoidal lining cells. Impaired sinusoidal microcirculation leads to metabolic dysfunction and ischemic damage of adjacent liver cell plates and further focal hepatocellular necrosis/ dropout. Because drugs and toxins that cause SOS/ VOD are selectively toxic to SECs than to hepatocytes, the disease is initiated by damage at the sinusoidal level. If present, prolonged loss of normal SEC with capillarization permits HSC (hepatic stem cell) activation and perisinusoidal fibrosis and fibrous occlusion of central venules in severe cases. Thus, aberrant CD34 expression by SECs and increase in SMA positive HSCs seem to present the pathogenic consequences of sinusoidal endothelial injury, and the altered distribution pattern of GS-expressing hepatocytes may represent an adaptative process reflecting impaired sinusoidal microcirculation.
A CSI score deduced calculates using an immunohistochemical panel consisting of CD34, SMA and GS may serve as an objective marker of chemotherapy induced sinusoidal injury and could help diagnose this peculiar form of liver injury [1].
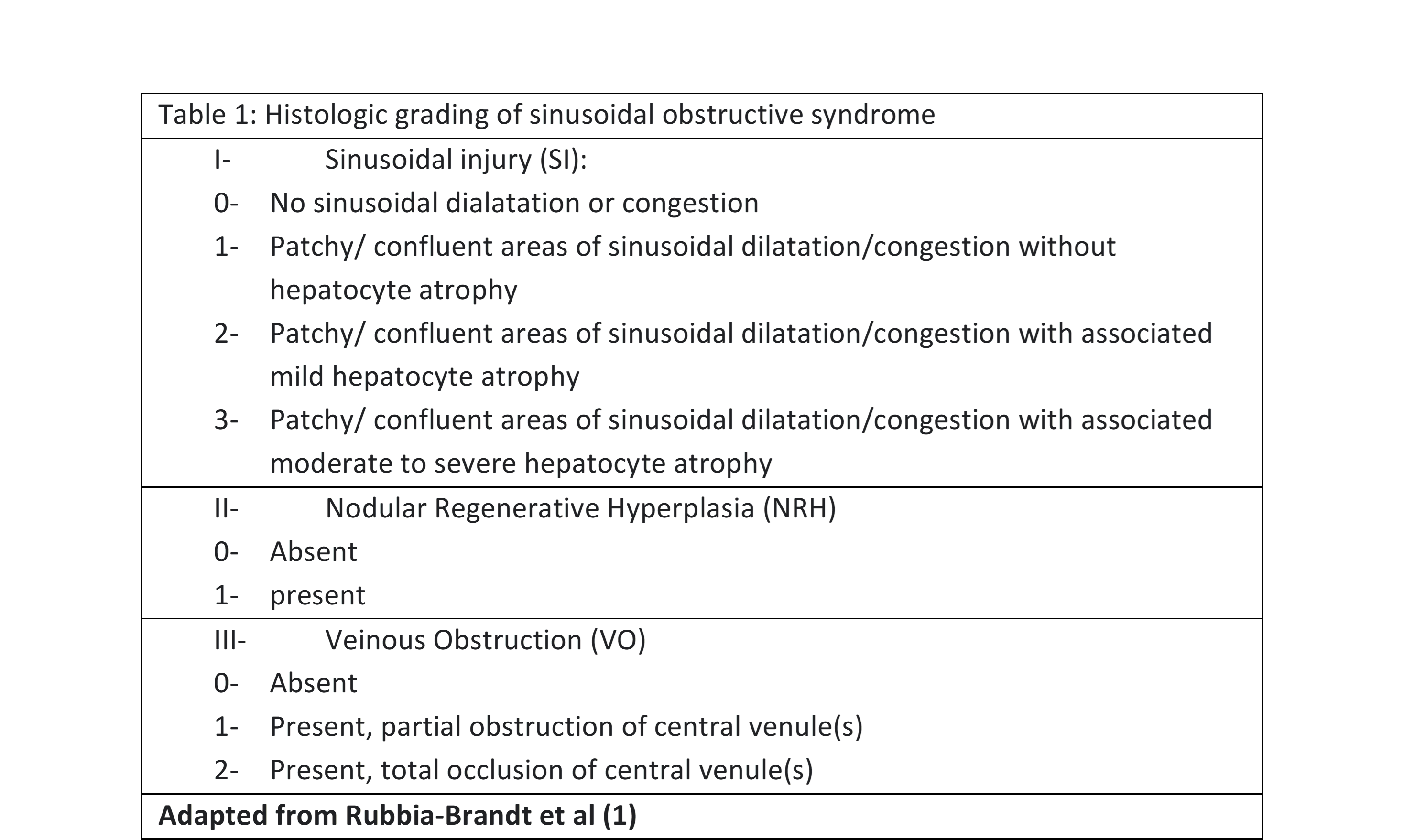
Table 1: Histologic grading of sinusoidal obstruction syndrome.
Management/ treatment:
Better comprehensive of the molecular events underlying chemotherapy associated hepatic injury [7] might also be a source of potential medical prevention, several options are beginning to emerge from studies in animal models. In the rat, administration of MMP-2/9 inhibitors or infusion of glutathione prevented the development of SOS by reducing SEC damage. In hematopoietic stem cell transplantation, preserved hepatic function was seen in patients treated with glutamine a possible inducer of glutathione synthesis. These approaches could be therapeutically viable strategies for prevention of OX- associated liver injury. Aspirin intake has been associated with reduced risk for sinusoidal lesions. Targeted biologic molecules are increasingly being used for systemic treatment of CRLM. Bevacizumab has a protective effect against Ox induced sinusoidal injury. The suggested mechanism is that VEGF blockade by Bevacizumab may lead to downregulation of MMP-9 production and release thus may attenuate endothelial lesions [2].
However, none of these modalities reduced the incidence of fatal HSOS. Although, the ursodeoxycholic acid appears to be promising and well tolerated. The only available policy to avoid HSOS is the use of less intensive regimen [3,5,18].
As 70 to 85% of patients with HSOS recover spontaneously, the treatment is mainly supportive. Ascites treated with sodium restriction, diuretics and therapeutic paracentesis for discomfort or shortness of breath with oxygen therapy [3,5].
Two molecules of interest have been largely discussed and considered in clinical trials.
Heparin: heparins have been the most widely used drugs for the treatment and prevention of endothelial cell disorders. Several animal studies and clinical trials have suggested that in addition to its well-known anticoagulant effects, heparin also processes anti-inflammatory properties, mainly mediated by inhibition of IL6 release and its activity, a phenomenon also demonstrated in patients with COVID 19 treated with Low Molecular Weight Heparin.
Defibrotide: It is currently approved for the treatment of pediatric and adult hepatic VOD/ SOS with MOF. In this setting, DF has demonstrated efficacy (pro fibrinolytic, anti-thrombotic, anti-ischemic and anti-inflammatory activity) and safety (negligible hemorrhagic risk) in critically ill patients with MOF, as well as a significant reduction in PAI-1 and other markers of endothelial stress in patients with VOD/ SOS and MOF successfully treated with DF(28).
Evolution:
It seems difficult to predict the future of SOS/ VOD secondary to COVID, considering that the diagnosed reported cases result mainly from post mortem autopsy [27-29] and the true incidence of its occurrence is unknown and sure lot of not diagnosed ones had well or bad progressed in silence.
The potential for regression of chemotherapy associated liver injury, notably SOS remains unknown, as does the time frame for this regression and weather delayed hepatic complications can arise [2].
The course of SOS/VOD induced by chemotherapy is unknown, including cytarabine induced ones. Published series concerning SOS/ VOD due to oxaliplatin reported an incidence of OC-induced SOS varies between 8,3 and 54%. Patient with OX-induced SOS in the setting of CRLM have significantly impaired functional hepatic reserve and are predisposed to increase blood transfusions and higher morbidity after hepatic resection. Recent studies have demonstrated that SOS induced by Ox based chemotherapy might diminish the response to chemotherapy in patients with CRLM. SOS may also compromise liver regeneration in patients undergoing hepatectomy [1,2,30].
Splenomegaly which is associated to Ox-induced SOS, regressed in 35% of patients 6 months after the end of chemotherapy, in 85% at one year, and in all patients at 18 months [24]. And histologic lesion regressed only after nine months without chemotherapy, whereas steatosis and steatohepatitis persist. Patients with interval time between chemotherapy and surgery more than 270 days had a significantly lower prevalence of grade 2-3 SOS (19,4% VS 40%, p=0,022) [30].
Conclusion
SOS/ VOD etiologies concern any endothelial aggressive agent as radiotherapy in TBI, chemotherapy in HSCT or AML induction and even virus could induce and worsen this complication.
Both pathologist and clinician should be aware of this syndrome as it has a relatively prevalence and may affect patients’ outcomes.
Diagnosis needs a bundle of signs, new biologic biomarker and ultrasound exam could help noninvasive recognition of SOS/ VOD.
References
- Stevenson HL, Prats MM, Sasatomi E. Chemotherapy-induced Sinusoidal Injury (CSI) score: a novel histologic assessment of chemotherapy-related hepatic sinusoidal injury in patients with colorectal liver metastasis. BMC Cancer, 2017; 17(1): 35.
- Rubbia-Brandt L. Sinusoidal obstruction syndrome. Clin Liver Dis, 2010; 14(4): 651–668.
- Helmy A. Review article: updates in the pathogenesis and therapy of hepatic sinusoidal obstruction syndrome. Aliment Pharmacol Ther, 2006; 23(1): 11–25.
- Mohty M, Malard F, Alaskar AS, Aljurf M, Arat M, Bader P, et al. Diagnosis and severity criteria for sinusoidal obstruction syndrome/veno-occlusive disease in adult patients: a refined classification from the European society for blood and marrow transplantation (EBMT). Bone Marrow Transplant, 2023; 1–6.
- Mohty M, Malard F, Abecassis M, Aerts E, Alaskar AS, Aljurf M, et al. Sinusoidal obstruction syndrome/veno-occlusive disease: current situation and perspectives-a position statement from the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant, 2015; 50(6): 781–789.
- Kernan NA, Richardson PG, Smith AR, Triplett BM, Antin JH, Lehmann L, et al. Defibrotide for the treatment of hepatic veno-occlusive disease/sinusoidal obstruction syndrome following nontransplant-associated chemotherapy: Final results from a post hoc analysis of data from an expanded-access program. Pediatr Blood Cancer, 2018; 65(10): e27269.
- Mavrikou I, Chatzidimitriou D, Skoura L, Nikolousis E, Sakellari I, Gavriilaki E. Molecular Advances in Sinusoidal Obstruction Syndrome/Veno-Occlusive Disease. Int J Mol Sci, 2023; 24(6): 5620.
- Baroiu L, Dumitru C, Iancu A, Leșe AC, Drăgănescu M, Baroiu N, et al. COVID-19 impact on the liver. World J Clin Cases, 2021; 9(16): 3814-3825.
- Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN, 2023.
- Watts J, Nimer S. Recent advances in the understanding and treatment of acute myeloid leukemia. F1000Research, 2018; 7: F1000 Faculty Rev-1196.
- Short NJ, Konopleva M, Kadia TM, Borthakur G, Ravandi F, DiNardo CD, et al. Advances in the Treatment of Acute Myeloid Leukemia: New Drugs and New Challenges. Cancer Discov, 2020; 10(4): 506–525.
- Li W, Gong X, Sun M, Zhao X, Gong B, Wei H, et al. High-dose cytarabine in acute myeloid leukemia treatment: a systematic review and meta-analysis. PloS One, 2014; 9(10): e110153.
- Mulchandani R, Lyngdoh T, Kakkar AK. Deciphering the COVID-19 cytokine storm: Systematic review and meta-analysis. Eur J Clin Invest, 2021; 51(1): e13429.
- COVID-19 and Acute Myeloid Leukemia - Hematology.org, 2023.
- Marchesi F, Salmanton-García J, Emarah Z, Piukovics K, Nucci M, López-García A, et al. COVID-19 in adult acute myeloid leukemia patients: a long-term follow-up study from the European Hematology Association survey (EPICOVIDEHA). Haematologica, 2023; 108(1): 22–33.
- Zeidan AM, Boddu PC, Patnaik MM, Bewersdorf JP, Stahl M, Rampal RK, et al. Special considerations in the management of adult patients with acute leukaemias and myeloid neoplasms in the COVID-19 era: recommendations from a panel of international experts. Lancet Haematol, 2020; 7(8): e601–612.
- Modemann F, Ghandili S, Schmiedel S, Weisel K, Bokemeyer C, Fiedler W. COVID-19 and Adult Acute Leukemia: Our Knowledge in Progress. Cancers, 2022; 14(15): 3711.
- Cristiano A, Palmieri R, Fabiani E, Ottone T, Divona M, Savi A, et al. The Venetoclax/Azacitidine Combination Targets the Disease Clone in Acute Myeloid Leukemia, Being Effective and Safe in a Patient with COVID-19. Mediterr J Hematol Infect Dis, 2022; 14(1): e2022041.
- Mohty M, Malard F, Abecassis M, Aerts E, Alaskar AS, Aljurf M, et al. Sinusoidal obstruction syndrome/veno-occlusive disease: current situation and perspectives-a position statement from the European Society for Blood and Marrow Transplantation (EBMT). Bone Marrow Transplant, 2015; 50(6): 781–789.
- U R, M C, A M, B H. Hepatic venoocclusive disease in blood and bone marrow transplantation in children and young adults: incidence, risk factors, and outcome in a cohort of 241 patients. J Pediatr Hematol Oncol, 2002; 24(9).
- Corbacioglu S, Jabbour EJ, Mohty M. Risk Factors for Development of and Progression of Hepatic Veno-Occlusive Disease/Sinusoidal Obstruction Syndrome. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant, 2019; 25(7): 1271–1280.
- Sonzogni A, Previtali G, Seghezzi M, Grazia Alessio M, Gianatti A, Licini L, et al. Liver histopathology in severe COVID 19 respiratory failure is suggestive of vascular alterations. Liver Int, 2020; 40(9): 2110–2116.
- Boula AM, Mantadakis E, Xilouri IM, Christoforidou AV, Foudoulakis AM, Samonis G. Veno-occlusive disease of the liver associated with chronic myelomonocytic leukemia treated with vincristine and standard doses of cytarabine. Am J Hematol, 2005; 79(3): 216–219.
- Overman MJ, Maru DM, Charnsangavej C, Loyer EM, Wang H, Pathak P, et al. Oxaliplatin-mediated increase in spleen size as a biomarker for the development of hepatic sinusoidal injury. J Clin Oncol Off J Am Soc Clin Oncol. 2010 May 20;28(15):2549–2455.
- Cairo MS, Cooke KR, Lazarus HM, Chao N. Modified diagnostic criteria, grading classification and newly elucidated pathophysiology of hepatic SOS/VOD after haematopoietic cell transplantation. Br J Haematol, 2020; 190(6): 822–836.
- Yoon JH, Choi CW, Won JH. Hepatic sinusoidal obstruction syndrome/veno-occlusive disease after hematopoietic cell transplantation: historical and current considerations in Korea. Korean J Intern Med, 2021; 36(6): 1261–1280.
- Sonzogni A, Previtali G, Seghezzi M, Alessio MG, Gianatti A, Licini L, et al. Liver and COVID 19 Infection: A Very Preliminary Lesson Learnt from Histological Post-mortem Findings in 48 patients, 2020.
- Calabretta E, Moraleda JM, Iacobelli M, Jara R, Vlodavsky I, O’Gorman P, et al. COVID‐19‐induced endotheliitis: emerging evidence and possible therapeutic strategies. Br J Haematol, 2021; 193(1): 43–51.
- Lagana SM, Kudose S, Iuga AC, Lee MJ, Fazlollahi L, Remotti HE, et al. Hepatic pathology in patients dying of COVID-19: a series of 40 cases including clinical, histologic, and virologic data. Mod Pathol, 2020; 33(11): 2147–2155.
- Vigano L, De Rosa G, Toso C, Andres A, Ferrero A, Roth A, et al. Reversibility of chemotherapy-related liver injury. J Hepatol, 2017; 67(1): 84–91.

