Classic Complicated Silicosis
Chaimae Lahlou*, Ihssan Hadj Hsain, Chaymae Faraj, Sara Essetti, Rachida Saouab, Hassan Ennouali and Jamal El Fenni
Radiology Department, Mohammed V Military Teaching Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Received Date: 01/10/2024; Published Date: 07/11/2024
*Corresponding author: Chaimae Lahlou, Radiology Department, Mohammed V Military Teaching Hospital, Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Silicosis is caused by the inhalation of fine particles of crystalline silicon dioxide (silica). Quartz represents the predominant crystalline form of silica. Professions involving mining, quarrying, and tunneling are commonly linked to silicosis. This disease presents in two clinical variations: acute silicosis, characterized by alveolar silicoproteinosis, and classic silicosis, characterized by chronic interstitial reticulonodular disease. Classic silicosis cases can be further categorized as either simple or complicated based on radiographic observations.
Complicated silicosis, also known as progressive massive fibrosis, evolves through the enlargement and merging of individual silicotic nodules.
On chest radiographs, complicated silicosis is typically identified by sizable, symmetrical bilateral opacities exceeding 1 cm in diameter with irregular margins. These extensive opacities arise from the coalescence of nodules and are commonly situated in the middle lung zone or the peripheral one-third of the lung on axial images, transitioning to the upper lung zone on longitudinal images. Over time, these opacities migrate towards the hilum, creating a boundary of emphysematous lung tissue between the fibrotic region and the pleural surface.
CT scans of progressive massive fibrosis reveal focal soft-tissue masses with irregular or poorly defined borders and calcifications, encompassed by regions of emphysematous alterations. The lateral boundary of the mass typically aligns with the lateral chest wall. In some cases, cavitation resulting from ischemic necrosis may develop within a mass. Enlargement of the hilar and mediastinal lymph nodes may occur before parenchymal nodular tumors manifest. Having lymph nodes calcified is frequent and usually takes place on the outskirts of the node. The pattern of calcification known as the eggshell strongly suggests silicosis.
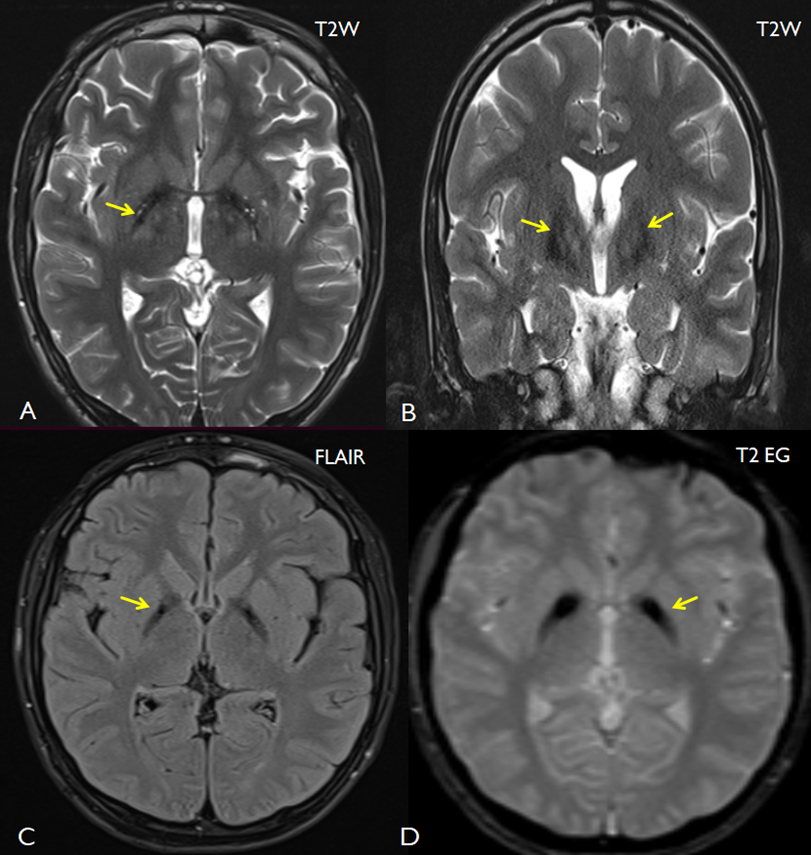
Figures A-D: An initial chest X-ray revealed bilateral nodular opacities affecting the upper lobes with irregular borders and containing calcifications (A).The CT scan revealed fibrotic masses affecting the upper lobes( pink arrows), involving the pulmonary hila and containing calcifications. Partially calcified mediastinal and hilar lymph nodes are also present (green arrows, B and C). On the parenchymal window (D), multiple bilateral pulmonary nodules and micronodules with lymphatic distribution (blue arrows) are observed, along with confluent subpleural micronodules forming pseudo pleural plaques (red arrow).
References
- Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Pneumoconiosis: comparison of imaging and pathologic findings. Radiographics, 2006; 26(1): 59-77. doi: 10.1148/rg.261055070.
- Antao VC, Pinheiro GA, Terra-Filho M, Kavakama J, Müller NL. High-resolution CT in silicosis: correlation with radiographic findings and functional impairment. J Comput Assist Tomogr, 2005; 29(3): 350-356. doi: 10.1097/01.rct.0000160424.56261.bc.

