Edema from Congestive Heart Failure as an Unusual Cause of Postoperative Ileus
Malik Peterson1,*, Sean Bassham1 and Anupam Gupta2
1Liberty University College of Osteopathic Medicine, Lynchburg VA, USA
2Good Samaritan Hospital, Mount Vernon IL, USA
Received Date: 04/10/2024; Published Date: 07/11/2024
*Corresponding author: Malik Peterson, Liberty University College of Osteopathic Medicine, Lynchburg VA, USA
Abstract
Post-emergency colectomy patients often experience a significant delay in the return of normal bowel function, which can be attributed to either mechanical issues or the development of an ileus. Prolonged ileus can often be challenging to differentiate from mechanical causes, leading to prolonged hospital stays and additional procedures. In this case, we describe an 83-year-old female patient who presented with a bleeding cecal mass and underwent robotic-assisted right hemicolectomy with intracorporeal ileal-transverse colon anastomosis. She had an intermittent return of physiological bowel function during her postoperative period. Subsequent imaging and a second surgery to evaluate the anastomotic segment revealed edema as an unusual cause of her prolonged ileus.
Keywords: Hemi-colectomy; Congestive Heart Failure (CHF); Postoperative ileus; Bowel wall edema; Dilated bowel loops
Introduction
The restoration of normal bowel function following emergency colectomy is frequently prolonged and can result from either the development of an ileus or mechanical causes [1-4]. Mechanical causes include adhesions, strictures, obstructions, intra-abdominal collection, and usually necessitate surgical correction to resolve the underlying issue [1,4,5]. Conversely, ileus is more prevalent and stems from bowel function disruptions without structural blockage [2,6]. These need supportive medical interventions such as medications, dietary modifications, fluid, electrolyte management, and time [2]. In this case, the patient's edema of the small bowel loops delayed the return of bowel function.
Case Report
An 83-year-old female with a body mass index of 15 and right-sided heart failure secondary to chronic obstructive pulmonary disease on home oxygen presented to the hospital with a bleeding cecal mass. Her past medical and surgical history were significant for hypertension, coronary artery disease, atrial fibrillation, peripheral vascular disease, status post aortic valve replacement, cardiac pacemaker, and a significant size hiatal hernia. She had a drop in hemoglobin from her complete blood work on arrival, a baseline of 12.4 to 11 gm/dl (gram/deciliter) within 2.5 hours, with symptoms of ongoing rectal bleeding and dizziness. Her baseline albumin was 2.6 gm/dL. The remainder of the blood work is noncontributory to the present case report. She underwent an emergent robotic-assisted right hemicolectomy with intracorporeal ileo-transverse anastomosis with a 60 mm (millimeter) stapler. The surgeon confirmed the intraoperative patency of anastomosis of 60mm, tension-free vascular anastomosis, and the common enterotomy was closed using absorbable V lock sutures. The mesenteric defect was closed with an additional absorbable vicryl suture.
The patient had a return of bowel function in the immediate postoperative period on day two with passage of flatus and stool with tolerance of an oral diet. Given her weak and debilitated condition, the patient was not eating enough to meet her caloric requirements and demonstrated limited mobility. Subsequently, she became obstructed on hospital day three. Bowel function in the form of flatus and stool would return and then obstruct intermittently over the next eight days. It was thought that she had prolonged ileus, given her inability to ambulate, multiple medical comorbidities, and risk factors. On hospital day 10, computed tomography of the abdomen and pelvis showed the flow of Gastrografin contrast across the ileal-transverse colon anastomosis and contrast was seen beyond the anastomosis, confirming its patency (figure 1). In addition, there were dilated loops of proximal small bowel with collapsed distal small bowel loops which appeared edematous (Figure 1).
On postoperative day 14, the patient continued to have an intermittent resolution of bowel function. There was a concern of kinking or twisting of the anastomosis, possible internal herniation, or a surgical etiology, which was resolving intermittently. In light of these concerns, the inability to adequately decompress the stomach, a large-size hiatal hernia, and fear of the patient having recurrent aspiration, a second surgery was performed on postoperative day 14. The patient underwent surgery for what was believed to be an anatomical issue. Intraoperatively, the surgeon confirmed an adequate-sized patent anastomosis with no structural issue identified aside from thickened dilated loops of terminal ileum, which appeared edematous. The anastomosis was broken down in this surgery, and the terminal ileum was converted to an ileostomy with a transverse colon mucous fistula as it was considered that this may be intermittently kinking. A revision anastomosis was not performed in view of the significant edema and a drop in albumin to 1.9 from 2.6 gm/dl. In the postoperative period, the ileostomy functioned intermittently again for one week. On day six following the second surgery, the patient underwent aggressive diuresis for extensive edema. She regained the function of her ostomy following this. As her diuresis continued, she had progressive improvement of her ostomy function.
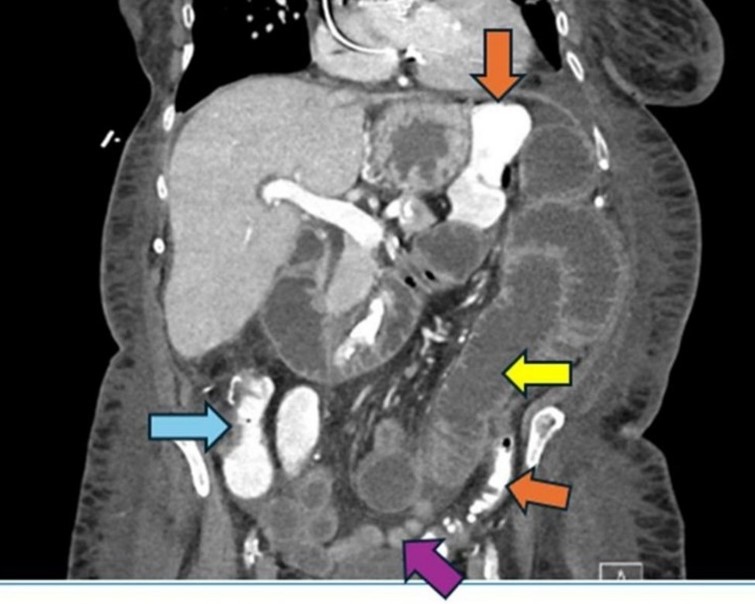
Figure 1: Hospital Day 10, Computed tomography abdomen and pelvis with Intravenous and oral contrast.
Dilated loops of proximal small bowel (Yellow arrow)
Collapsed distal small bowel (Purple arrow)
Patent anastomosis (Blue arrow)
Contrast seen beyond the anastomosis in the transverse and sigmoid colon (Orange arrows)
Discussion
Ileus post-bowel surgery is typically a normal physiological response that usually lasts less than 72 hours [7]. Delayed return of bowel function and ileus have been reported after colorectal surgery in approximately 10-25% of patients [7,8]. Ileus is often considered resolved once the patient has passed flatus [9]. There is no exact etiology known that causes ileus, and it is thought to be the result of a complex interplay of factors, such as medication, inflammation, and pharmacological agents that interfere with the neuro-hormonal pathway of the bowel loops [7-10]. There are a multitude of factors status post colorectal surgery which can cause prolonged postoperative ileus. These range from pharmacological anesthetic agents, type of surgery, postoperative ambulation, peripheral vascular disease, chronic obstructive pulmonary disease, edema, use of opioids, early enteral nutrition, etc [7-11]. Enhanced recovery after surgery pathway protocols have helped reduce postoperative ileus [9]. However, these protocols cannot be used in emergency surgery, as in our case. Management of postoperative ileus is mainly supportive care in the form of using COX-2 inhibitors, avoiding narcotics, adequate hydration to maintain normovolemia, nutritional support, postoperative ambulation, chewing gum, and time [7-10]. Prolonged postoperative ileus is often challenging to differentiate from mechanical causes of prolonged return of bowel function; they both have similar symptoms of abdominal bloating, distention, pain, nausea, vomiting, and inability to tolerate an oral diet [3,7-10,12]. Mechanical obstruction caused in the early postoperative period after colectomy may be due to anastomotic narrowing, kinking, adhesions, internal herniations, port site herniation, intussusception, leak, intra-abdominal collections, etc. Some of these will resolve with conservative management, like prolonged nasogastric decompression [3,12]. In our patient, however, we feared the risk of recurrent aspiration due to her history of a very large hiatal hernia. If the patient’s condition fails to resolve with conservative treatment, surgical correction may be required [3,12].
Our patient was an 83-year-old female with severe chronic obstructive pulmonary, worsening right-sided heart failure, anasarca, poor functional status, and multiple medical comorbidities - which can all cause prolonged ileus. It was originally thought that her symptoms were the result of a prolonged ileus caused by nonmodifiable risk factors such as age, hypertension, lack of ambulation, malnutrition, chronic obstructive pulmonary disease, peripheral vascular disease, and cardiac disease. Her intermittent symptoms, however, suggested a mechanical cause of her symptoms. Concern for a mechanical cause, in addition to deterioration in her health, led to her second surgery. Interestingly, after having a computed tomography scan with Gastrografin contrast to visualize the patency of the anastomosis, her symptoms temporarily improved. Given her past medical history and multiple risk factors for prolonged ileus, the most reasonable explanation is that her worsening obstruction was due to intramural intestinal edema secondary to right-sided heart failure, hypoalbuminemia, and inflammation. Right-sided heart failure leads to a reduction in cardiac output; as the heart loses its ability to contract, a "backlog" of blood accumulates in the venous circulation [13]. Another consideration is the patient’s prolonged non-ambulatory status. Since pelvic and abdominal bowel loops are in a more dependent position with the patient non-ambulatory, it makes sense how her lack of ambulation could contribute to her edema.
Administering excessive perioperative fluids can lead to intestinal edema, which may then lead to postoperative ileus. Edema causes dysfunction within the intestinal smooth muscle cells and activates intestinal glial cells, which can cause inflammation and reduce colonic motility [14]. This idea is further supported by the patient's improvement following the use of computed tomography with Gastrografin. Gastrografin is a hyperosmolar medium and is able to pull fluid out of the intestinal wall and into the lumen [15]. The use of Gastrografin in our patient reduced her intestinal wall edema and led to a temporary improvement in her symptoms. However, her edema eventually returned, given her underlying medical and nutritional issues, causing her bowel to become edematous again shortly thereafter. Our patient eventually required more aggressive treatment with diuresis to see a lasting improvement in her condition. Her right heart failure, hypoalbuminemia, and non-ambulatory status led to the development of significant intestinal edema, which became a significant contributor to prolonging the physiological return of bowel function.
Conclusion
As seen in our patient who underwent emergency surgery with multiple medical risk factors that can cause prolonged ileus, prolonged postoperative ileus is challenging to differentiate from mechanical causes of small bowel obstruction in the immediate postoperative phase. Our patient had multiple nonmodifiable risk factors that lead to the development of significant intestinal edema. As seen in our case, bowel loop edema can mimic a mechanical cause of obstruction and lead to a delay in the return of physiologic bowel function.
Author Contributions: Malik Peterson, Sean Bassam, and Anupam Gupta made contributions to the following:
- Concept and design of study or acquisition of data or analysis and interpretation of data
- Drafting the article or revising it critically for important intellectual content
- Final approval of the version to be published.
Guarantor: Anupam Gupta, MD
Conflicts of interests: None of the authors have any conflicts of interests to disclose
Grants: The author(s) received no specific funding for this work
References
- Krielen P, Kranenburg LPA, Stommel MWJ, et al. Variation in the management of adhesive small bowel obstruction in the Netherlands: a prospective cross-sectional study. Int J Surg, 2023; 109(8): 2185-2195. 10.1097/JS9.0000000000000471.
- Patil S, Sharma S, Paliwal S. Pathogenesis, Updates on Current Treatment Options and Alvimopan for Postoperative Ileus. Biosciences Biotechnology Research Asia, 2023; 20(2): 653-666. doi: 10.13005/bbra/3119.
- Ong AW, Myers SR. Early postoperative small bowel obstruction: A review. Am J Surg, 2020; 219(3): 535-539. doi: 10.1016/j.amjsurg.2019.11.008.
- Khawaja ZH, Gendia A, Adnan N, et al. Prevention and Management of Postoperative Ileus: A Review of Current Practice. Cureus, 2022; 14(2): e22652. doi: 10.7759/cureus.22652.
- Behman R, Nathens AB, Mason S, et al. Association of Surgical Intervention for Adhesive Small-Bowel Obstruction with the Risk of Recurrence. JAMA Surg, 2019; 154(5): 413-420. 10.1001/jamasurg.2018.5248.
- Li S, Li Y. Adhesive small-bowel obstruction: Conservative versus surgical management? World Journal of Surgical Infection, 2023; 2(1): p 21-28. doi: 10.4103/wjsi.wjsi_3_23.
- Buscail E, Deraison C: Postoperative ileus: A pharmacological perspective. Br J Pharmacol, 2022; 179(13): 3283-3305. doi: 10.1111/bph.15800.
- Penfold JA, Wells CI, Du P, et al. Relationships between serum electrolyte concentrations and ileus: A joint clinical and mathematical modeling study. Physiol Rep, 2021; 9(3): e14735. doi: 10.14814/phy2.14735.
- Ashcroft J, Singh AA, Ramachandran B, et al. Reducing ileus after colorectal surgery: A network meta-analysis of therapeutic interventions. Clin Nutr, 2021; 40(7): 4772-4782. doi: 10.1016/j.clnu.2021.05.030.
- Quiroga-Centeno AC, Jerez-Torra KA, Martin-Mojica PA, et al. Risk Factors for Prolonged Postoperative Ileus in Colorectal Surgery: A Systematic Review and Meta-analysis. World J Surg, 2020; 44(5): 1612-1626. doi: 10.1007/s00268-019-05366-4.
- Fujiyoshi S, Homma S, Yoshida T, et al. A Study of risk factors of postoperative ileus after laparoscopic colorectal resection. Ann Gastroenterol Surg, 2023; 7(6): 949-954. doi: 10.1002/ags3.12705.
- Detz DJ, Podrat JL, Muniz-Castro JC, et al. Small bowel obstruction. Curr Probl Surg, 2021; 58(7): 100893. doi: 10.1016/j.cpsurg.2020.100893.
- Rosenkranz S, Howard LS, Gomberg-Maitland M, et al. Systemic Consequences of Pulmonary Hypertension and Right-Sided Heart Failure. Circulation, 2020; 141(8): 678-693. doi: 10.1161/circulationaha.116.022362.
- Mazzotta E, Villalobos-Hernandez EC, Fiorda-Diaz J, et al. Postoperative Ileus and Postoperative Gastrointestinal Tract Dysfunction: Pathogenic Mechanisms and Novel Treatment Strategies Beyond Colorectal Enhanced Recovery After Surgery Protocols. Front Pharmacol, 2020; 11: 583422. doi: 10.3389/fphar.2020.583422.
- Esaki M, Tamura Y, Ichijima R, et al. Efficacy and timing of gastrografin administration after ileus tube insertion in patients with adhesive small bowel obstruction. Arab J Gastroenterol, 2022; 23(1): 45-51. doi: 10.1016/j.ajg.2021.12.004.

