Diagnostic Challenge of Extensive Bone Edema Mimicking Paget's Disease in Psoriatic Spondylitis
Angelo Nigro*
Department of Rheumatology of Lucania - UOSD of Rheumatology, "Madonna delle Grazie" Hospital, Matera, Italy
Received Date: 07/10/2024; Published Date: 06/11/2024
*Corresponding author: Angelo Nigro, MD. Department of Rheumatology of LucaniaUOSD of Rheumatology "Madonna delle Grazie" HospitalMatera, Italy
ORCID: 0000-0002-1234-5678
Abstract
Psoriatic spondylitis can manifest with atypical imaging and histopathological features, complicating the diagnostic process. We report the case of a 30-year-old male presenting with intense inflammatory low back pain and alternating gluteal pain. Magnetic resonance imaging (MRI) revealed extensive bone marrow edema in the left iliac wing, initially suggesting Paget's disease based on histopathological findings. However, a comprehensive clinical evaluation, including detailed examination for psoriasis, ultimately led to the diagnosis of psoriatic spondylitis. Initial treatment with non-steroidal anti-inflammatory drugs (NSAIDs) and bisphosphonates was ineffective. Subsequent therapy with adalimumab provided symptomatic relief but was discontinued due to paradoxical worsening of psoriasis. Secukinumab was initiated, resulting in significant improvement in both articular and cutaneous symptoms. This case underscores the necessity of correlating clinical findings with imaging and histopathology to avoid misdiagnosis. Secukinumab may be a particularly effective treatment option for psoriatic spondylitis when initial therapies fail or cause adverse reactions.
Keywords: Psoriatic spondylitis; Bone edema; Paget's disease; Secukinumab
Introduction
Psoriatic Arthritis (PsA) is a chronic inflammatory arthropathy associated with psoriasis, involving both peripheral joints and the axial skeleton. Psoriatic spondylitis, a subset of PsA, is characterized by inflammation of the sacroiliac joints and spine, leading to pain and functional impairment [1]. Magnetic resonance imaging (MRI) is crucial for the early detection of sacroiliitis and spondylitis. However, extensive bone marrow edema is atypical in psoriatic spondylitis and can mimic other pathologies, including infections, malignancies, or metabolic bone diseases such as Paget's disease [2]. Histopathological findings may further complicate the diagnosis if not correlated with the clinical context. We present a case that illustrates the diagnostic challenges posed by unusual MRI findings and biopsy results initially suggestive of Paget's disease, ultimately diagnosed as psoriatic spondylitis.
Case Report
A 30-year-old male presented to our rheumatology clinic with a six-month history of severe low back pain of inflammatory nature. The pain was most pronounced at night and was associated with morning stiffness lasting over one hour. The patient also reported alternating gluteal pain. There was no personal or family history of psoriasis or other rheumatologic conditions. The clinical examination revealed tenderness over both sacroiliac joints and a reduced range of motion in the lumbar spine. Skin examination showed no visible psoriatic lesions, and nail examination was unremarkable. Neurological examination showed no abnormalities. Laboratory tests showed normal Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP). Rheumatoid Factor (RF) and anti-cyclic citrullinated peptide antibodies were negative. HLA-B27 typing was also negative. Serum calcium, phosphate, and alkaline phosphatase levels were within normal limits.
MRI of the pelvis and sacroiliac joints revealed extensive bone marrow edema involving a significant portion of the left iliac wing and sacroiliac joint on Short Tau Inversion Recovery (STIR) sequences (Figures 1a and 1b). The extent of the edema was unusually extensive for typical inflammatory sacroiliitis. Given the atypical and extensive nature of the bone edema, differential diagnoses included infectious sacroiliitis, neoplastic infiltration, and metabolic bone diseases such as Paget's disease. To clarify the diagnosis, a computed tomography (CT)-guided core needle biopsy of the left iliac bone was performed. Histopathological examination reported: "Microscopic examination of periosteum and cortical bone with juxtaposition of strongly irregular cement lines, as observed in Paget's disease."
Based on the biopsy report, Paget's disease was initially considered. The patient was started on bisphosphonates, first with alendronate and subsequently with neridronate due to inadequate response. However, minimal improvement in symptoms was noted following bisphosphonate therapy. Persistent symptoms and lack of significant response to bisphosphonates prompted re-evaluation. A thorough skin examination revealed subtle erythematous scaly lesions on the scalp, consistent with psoriasis. Nail examination demonstrated mild pitting. Alkaline phosphatase levels remained normal, which is atypical in active Paget's disease. The bone edema pattern on MRI was reconsidered within the context of inflammatory spondyloarthritis. Applying the Classification Criteria for Psoriatic Arthritis (CASPAR) [3], the patient met the requirements for a diagnosis of psoriatic spondylitis. NSAIDs were initiated but failed to provide sufficient symptom control. Biologic therapy with adalimumab at 40 mg subcutaneously every 14 days was subsequently started. The patient experienced significant improvement in back pain and functional status within four weeks. At the 6-month follow-up, MRI demonstrated resolution of bone marrow edema in the sacroiliac joints. After approximately one year on adalimumab, the patient developed diffuse psoriasis with extensive plaques on the scalp, trunk, and limbs. Dermatological assessment confirmed paradoxical worsening of psoriasis, likely induced by TNF-α inhibitor therapy. To prevent further exacerbation of psoriasis, adalimumab was discontinued. Secukinumab was initiated at 300 mg subcutaneously at weeks 0, 1, 2, 3, and 4, followed by monthly maintenance doses.
The patient reported marked improvement in back pain and mobility within eight weeks of initiating secukinumab. Significant reduction in psoriatic lesions was observed, with near-complete clearance at three months. At the one-year follow-up, the patient remained symptom-free, with normal inflammatory markers and no adverse events reported.
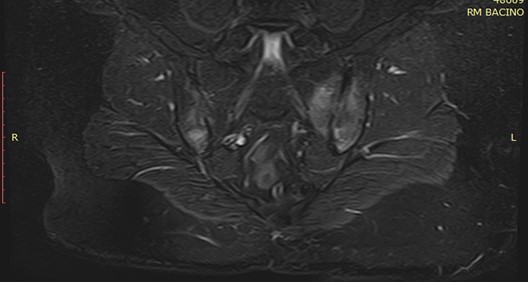
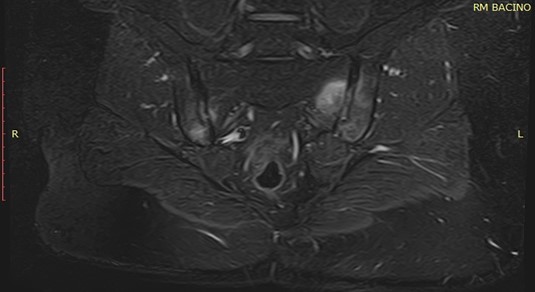
Figure 1a and 1b: MRI STIR sequences showing extensive bone marrow edema involving the left iliac wing and sacroiliac joint.
Discussion
This case highlights the complexities involved in diagnosing psoriatic spondylitis when atypical imaging and histopathological findings are present. Extensive bone marrow edema is not commonly associated with psoriatic spondylitis [4]. Such findings may prompt clinicians to consider alternative diagnoses, including infections, malignancies, or metabolic bone disorders.
The biopsy showed features suggestive of Paget's disease, specifically the juxtaposition of strongly irregular cement lines in the periosteum and cortical bone. However, the clinical features did not align with Paget's disease, which typically presents in older adults with elevated alkaline phosphatase levels and characteristic radiographic changes [5].
Reliance solely on imaging and histopathology without integrating clinical findings can lead to misdiagnosis. A comprehensive assessment, including detailed skin and nail examination, is crucial. The identification of psoriatic skin and nail changes, combined with inflammatory back pain and MRI findings consistent with sacroiliitis, supported the diagnosis of psoriatic spondylitis.
TNF-α inhibitors such as adalimumab can induce or worsen psoriasis in some patients [6]. The mechanism may involve immune system modulation resulting in an imbalance in cytokine expression, particularly affecting interferon-alpha pathways [7]. Secukinumab, an interleukin-17A (IL-17A) inhibitor, has demonstrated effectiveness in treating both the articular and cutaneous manifestations of psoriatic disease [8]. It offers a valuable alternative when TNF-α inhibitors are contraindicated or poorly tolerated.
Conclusion
This case underscores the necessity for vigilance when confronting atypical presentations of psoriatic spondylitis. The initial diagnostic challenge was compounded by the presence of extensive bone marrow edema on MRI and a biopsy report suggestive of Paget's disease, which diverted the diagnostic process. The clinical and radiological response to adalimumab helped confirm the inflammatory nature of the condition, redirecting the diagnosis to spondyloarthritis. This case emphasizes the importance of integrating clinical presentation, imaging, histopathology, and therapeutic response in complex diagnostic scenarios. A therapeutic trial with appropriate agents may be warranted when diagnostic uncertainty persists. Secukinumab proved to be an effective treatment following the development of paradoxical psoriasis with adalimumab, highlighting its utility in managing psoriatic spondylitis, especially when initial therapies fail or induce adverse reactions.
Declarations
Ethics Approval and Consent to Participate: Not applicable.
Consent for Publication: Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Availability of Data and Materials: Data sharing is not applicable as no datasets were generated or analyzed during the current study.
Competing Interests: The authors declare no competing interests.
Funding: No funding was received for this study.
Authors' Contributions: All authors contributed to the conception, drafting, and revision of the manuscript. All authors read and approved the final manuscript.
Acknowledgments: We thank the patient for his consent and participation.
References
- Ramiro S, Nikiphorou E, Sepriano A, Ortolan A, Webers C, Baraliakos X, et al. ASAS-EULAR recommendations for the management of axial spondyloarthritis: 2022 update. Ann Rheum Dis, 2023; 82(1): 19-34. doi: 10.1136/ard-2022-223296.
- Wu D, Griffith JF, Lam SHM, Wong PCH, Shi L, Li EK, et al. Progressive structural bone changes and their relationship with treatment in patients with psoriatic arthritis: a longitudinal HR-pQCT study. Arthritis Res Ther, 2019; 21(1): 265. doi: 10.1186/s13075-019-2043-3.
- Helliwell PS, Taylor WJ. Classification and diagnostic criteria for psoriatic arthritis. Ann Rheum Dis, 2005; 64 Suppl 2. doi: 10.1136/ard.2004.032318.
- Khmelinskii N, Regel A, Baraliakos X. The role of imaging in diagnosing axial spondyloarthritis. Front Med (Lausanne), 2018; 5: 106. doi: 10.3389/fmed.2018.00106.
- Tan A, Ralston SH. Clinical presentation of Paget's disease: evaluation of a contemporary cohort and systematic review. Calcif Tissue Int, 2014; 95(5): 385-392. doi: 10.1007/s00223-014-9904-1.
- Collamer AN, Guerrero KT, Henning JS, Battafarano DF. Psoriatic skin lesions induced by tumor necrosis factor antagonist therapy: a literature review and potential mechanisms of action. Arthritis Rheum, 2008; 59(7): 996-1001. doi: 10.1002/art.23835.
- Brown G, Wang E, Leon A, Huynh M, Wehner M, Matro R, et al. Tumor necrosis factor-α inhibitor-induced psoriasis: Systematic review of clinical features, histopathological findings, and management experience. J Am Acad Dermatol, 2017; 76(2): 334-341. doi: 10.1016/j.jaad.2016.08.012.
- Kolbinger F, Di Padova F, Deodhar A, Hawkes JE, Huppertz C, Kuiper T, et al. Secukinumab for the treatment of psoriasis, psoriatic arthritis, and axial spondyloarthritis: Physical and pharmacological properties underlie the observed clinical efficacy and safety. Pharmacol Ther, 2022; 229: 107925. doi: 10.1016/j.pharmthera.2021.107925.

