Mycoplasma Pneumoniae-Associated Stevens-Johnson Syndrome in A Pediatric Patient
Kalin Atanasov*, Iren Tzotcheva and Djanet Hasanova
Pediatric Clinic, University Hospital for Active Treatment and Emergency Medicine “N. I. Pirogov”, “General Eduard I. Totleben”, Bulgaria
Received Date: 23/09/2024; Published Date: 05/11/2024
*Corresponding author: Kalin Atanasov MD, Pediatric Clinic, University Hospital for Active Treatment and Emergency Medicine “N. I. Pirogov”, “General Eduard I. Totleben” Blvd. 21, 1606 Sofia, Bulgaria
Abstract
The following report showcases a pubescent boy, admitted to our department with major complaints: fever, adynamia, cough, red eye, and mouth sores, over a period of 2 weeks. Clinical observation revealed conjunctival injection, oral and genitourinary mucositis (hemorrhagic crusts, balanitis), and broncho-obstructive syndrome. A form of Stevens-Johnson syndrome was suspected, one not linked to the commonly associated medications. After departmental consideration tests were performed, which revealed acute Mycoplasma pneumoniae infection. The patient was started on antibiotic treatment with a macrolide, corticosteroids, and local antiseptic and anti-inflammatory treatment was implemented. Rapid clinical improvement ensued, and the boy was successfully discharged.
Keywords: Mycoplasma pneumoniae; Pediatric; Atypical; Mucositis; Stevens-Johnson syndrome
Introduction
Mycoplasma pneumoniae (MP) is a recognized pathogen, causing frequent outbreaks of respiratory infections in the pediatric population, mainly aged 3-15 years. The most common clinical presentation is community-acquired pneumonia. A correlation with asthma exacerbations was identified [1], attributing up to 50% of studied asthma attacks to associated Mycoplasma pneumoniae infection.
The microorganism lacks a cell wall, rendering beta-lactam antibiotics useless, and relies mostly on host metabolism to ensure its survival and replication. Cross-reactivity between MP- antigens and human tissue antigens on the basis of molecular mimicry [2] is believed to cause most extrapulmonary manifestations.
Typical MP-induced infections include tracheobronchitis and pneumonia, while the following extrapulmonary presentations are significantly rarer: central nervous system involvement (encephalitis, Guillain-Barre syndrome, ataxia), dermatological involvement (erythema multiforme, atypical Stevens-Jonson syndrome), hematological involvement (thrombocytopenia), and others.
Case Report
A previously healthy 14-year-old boy experienced fever, adynamia, odynophagia, non-productive cough and wheezing, red eye, mouth and genital sores over a period of 2 weeks prior to hospitalization. The patient was misdiagnosed with bacterial pharyngitis and treated with an oral Cephalosporin to no effect. Inspection revealed severe oral mucositis (Figure 1), conjunctival infection, non-purulent balanitis, as well as broncho-obstructive syndrome.
Laboratory markers of inflammation at presentation revealed thrombocytosis (up until discharge), as well as elevation of the erythrocyte sedimentation rate (ESR) and C-reactive protein (Table 1). Other biochemical markers, as well as kidney, liver function and hemostasis detected no abnormality. Throat swab and hemoculture yielded no bacterial co-infection.
A panel of serological markers was performed, resulting in the detection of elevated Mycoplasma pneumoniae-specific IgM and IgG titers - 24,8 AU/mL and 7,13 AU/mL, respectively (reference range for both- 0-1 AU/mL).
The latter results prompted a treatment regimen with macrolide antibiotic Azithromycin 500mg daily and the corticosteroid Methylprednisolone 1mg/kg/daily in the initial days, followed by dose tapering over 1 month. Furthermore, topical antiseptic preparations and debridement were applied. The results were full resolution of the constitutional symptoms and pulmonary complications, near-absolute regression of the mucosal inflammation. This allowed discharge on the eighth day of hospitalization (Figure 2).
Table 1: Comparison of laboratory markers on day one and day six of hospitalization.
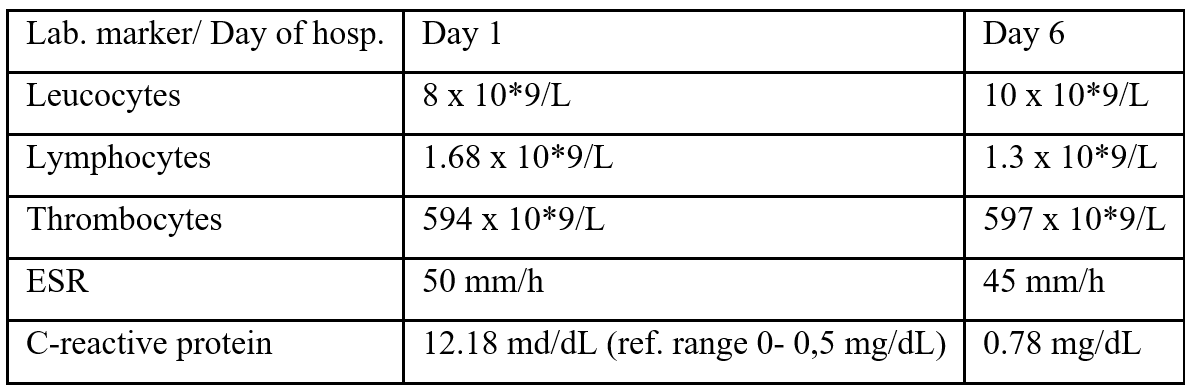

Figure 1: Oropharyngeal mucositis (day one of hospitalization) Nasal coagulum on the right due to preceding epistaxis is visible.

Figure 2: Day 8- discharge.
Discussion
Regarding the aforementioned patient, a diagnosis of atypical Stevens-Johnson syndrome (SJS) was made. SJS represents a delayed type of hypersensitivity reaction to antigens, most commonly drugs. Implicated medications include anti-epileptics, sulfonamides and some non-steroidal anti-inflammatory drugs [3]. Time-sensitive diagnosis and treatment are essential to disease outcome, since systemic complications in the form of sepsis are possible. A distinction has been made between SJS and the more severe condition toxic epidermal necrolysis (TEN), based on the degree of body surface involved. Pathognomonic for this condition is postburn-like epidermal necrosis and loss of skin. Diagnosis of TEN requires more than 30% of total body surface area involvement. An overlap between SJS and TEN is defined as 10-30% body surface injury. With less than 10% of body surface area involved, a diagnosis of SJS is made [4].
Dermatological involvement in our patient in the form of oropharyngeal and genitourinary mucositis with no epidermal lesions in the setting of serologically proven acute MP infection led us to the diagnosis of an atypical presentation of SJS. Several other infectious triggers for mucositis were considered- Epstein-Barr virus, Herpes simplex, Hepatitis B, and group A streptococci. They were dismissed, however, due to the lack of specific findings and the rapid resolution of our patient’s symptoms upon initiation of treatment.
In similar clinical settings, another medical team stressed the combined use of a macrolide antibiotic and corticosteroid in treating atypical SJS [5]. We have also found this to be of clinical benefit. A meta-analysis of the effect of combined immunoglobulin and corticosteroid use in SJS and TEN cases showed both reduced mortality and hospitalization duration, especially in those treated with high dose IVIG [6]. Fortunately, our patient did not require such a regimen.
Conclusion
Dermatological signs may be the presenting features of a myriad of infectious and rheumatologic conditions, as well as toxicological triggers. When dealing with pediatric patients, differentiating between these can be challenging, in part due to disease overlap, but also due to lacking scientific data in the form of clinical trials and case reports.
We believe this case sheds light on a rather atypical presentation of M. pneumoniae-infection, and thus provides insight on treatment options and outcomes, improving clinical knowledge in the pediatric field.
Conflicts of interests: none.
Grant information: the authors received no specific funding for this work.
References
- Biscardi S, Lorrot M, Marc E, Moulin F, Boutonnat-Faucher B, Heilbronner C, et al. Mycoplasma pneumoniae and asthma in children. Clin Infect Dis, 2004; 38(10): 1341-1346. doi: 10.1086/392498.
- Sánchez-Vargas FM, Gómez-Duarte OG. Mycoplasma pneumoniae-an emerging extra-pulmonary pathogen. Clin Microbiol Infect, 2008; 14(2): 105-117. doi: 10.1111/j.1469-0691.2007.01834.x.
- Lerch M, Mainetti C, Terziroli Beretta-Piccoli B, Harr T. Current Perspectives on Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis. Clin Rev Allergy Immunol, 2018; 54(1): 147-176. doi: 10.1007/s12016-017-8654-z.
- Gerull Roland, Nelle Mathias, Schaible Thomas. Toxic epidermal necrolysis and Stevens-Johnson syndrome: A review*. Critical Care Medicine, 2011; 39(6): p 1521-1532. DOI: 10.1097/CCM.0b013e31821201ed
- Beheshti R, Cusack B. Atypical Stevens-Johnson Syndrome Associated with Mycoplasma Pneumoniae. Cureus, 2022; 14(2): e21825. doi: 10.7759/cureus.21825.
- Ye LP, Zhang C, Zhu QX. The Effect of Intravenous Immunoglobulin Combined with Corticosteroid on the Progression of Stevens-Johnson Syndrome and Toxic Epidermal Necrolysis: A Meta-Analysis. PLoS One, 2016; 11(11): e0167120. doi: 10.1371/journal.pone.0167120.

