Clinical Implications of Psoriasis in Women's Comprehensive Health Programs: A Literature Review
Maria Inês Pulitini Bortoliero1, Valeria Petri2, Carlos Alberto Monson3,* and Marisa Teresinha Patriarca4
1Federal University of São Paulo, Escola Paulista de Medicina (UNIFESP-EPM); São Paulo (SP), Brazil
2Federal University of São Paulo, Escola Paulista de Medicina (UNIFESP-EPM), Dermatology Department; São Paulo (SP), Brazil
3Federal University of São Paulo - Oral and Systemic Health and Women’s Health - Dermatology Department; São Paulo (SP), Brazil
4Federal University of São Paulo, Escola Paulista de Medicina (UNIFESP-EPM), Interdisciplinary Center for Female Skin Pathology; São Paulo (SP), Brazil
Received Date: 22/09/2024; Published Date: 01/11/2024
*Corresponding author: Carlos Alberto Monson, Federal University of São Paulo - Oral and Systemic Health and Women’s Health - Dermatology Department; São Paulo (SP), Brazil
Abstract
Objective: This review explores the clinical and psychosocial implications of psoriasis in women's comprehensive health programs in the literature. We focus on management strategies and interventions that reduce impacts and improve clinical outcomes and quality of life.
Method: We performed a narrative literature review using relevant databases and applied strict inclusion and exclusion criteria to select consistent studies on the implications of psoriasis in women. We synthesized and analyzed the extracted data to identify patterns, similarities, and discrepancies between the studies and assess the quality and strength of the evidence presented.
Results: Psoriasis is a chronic inflammatory condition that has significant implications for the physical and psychological health of women, affecting essential aspects such as quality of life and mental and reproductive health. The prevalence and impact of psoriasis vary globally, and evidence indicates the need for clinical and public health approaches to manage and reduce the effects of the disease. Management strategies and interventions are needed, including levels of stress, anxiety, loneliness, stigmatization, and illness coinciding with the reproductive cycle, including treatment options for women of reproductive age, e.g., biological therapies. The explored publications provided valuable insights and revealed gaps in current knowledge.
Conclusion: Psoriasis substantially impacts women's whole health and quality of life, requiring a multidisciplinary approach for effective management. The present study sought to consolidate the current understanding of the topic by highlighting areas that may benefit from additional research and developing intervention strategies to optimize care for women with psoriasis.
Introduction
Psoriasis is a set of chronic skin implications, immune-mediated inflammatory with high prevalence and impact on people’s lives, especially in women, which have serious psychosocial implications associated with several comorbidities [2]. For almost thirty years psoriasis was assessed for many countries, and its impact on global health populations. It was revealed several symptoms such as pruritus and different comorbidities related, such as psoriatic arthritis, cardiovascular disease, metabolic syndrome, depression and anxiety, inflammatory bowel disease, and malignant neoplasms (lymphoma). Which lead to the physical, emotional, and social distress, related to the disfigurement, disability, loss of productivity, and overall impairment when added to the burden of chronic diseases [12].
Psoriasis affects around 100 million people worldwide. Its global prevalence varied in the range of 0.09-11.4%, only developed countries the average was between 1.5-5.0%. The highest lifetime prevalence was reported in Norway (11.43%) [4].
Lower prevalence was reported in under developing countries [9].
The pathophysiology of psoriasis is complex, such as genetic predisposition, triggering factors, and lifestyle influences the onset and progression. Psoriasis has an immune and central nervous systems implication, and the physical / emotional distresses participate in its appearance and exacerbation. The intrinsic mechanism of the disease involves inflammation and lack of control in the proliferation and differentiation of the keratinocytes, a phenomenon induced by the overproduction of cytokines and the chemokines that maintain a microenvironment favorable to the development and sustainment of inflammation [13].
Psoriasis impacts women's lives, not only physically but also through psychological and reproductive aspects, which makes sense for comprehensive women's health programs [13].
The present study sought more assertive strategies and better clinical outcomes than we have currently seen.
Objective: To analyze clinical implications of psoriasis in women.
Method
Study Design: A narrative literature review is characterized by a flexible and interpretive approach, with different data sources and standards, which explores current understanding of specific topics, identifying gaps in researches, that suggests new investigation [13].
Guiding Question: Can the clinical and psychosocial implications of psoriasis have an impact on women's general health, including well-being and quality of life?
Search in the Literature: Electronic databases without language restrictions at Evidence-Based Health statements, where were searched: Cochrane Central Register of Controlled Trials (CENTRAL) in the Cochrane Library (2021, Issue 7); MEDLINE via PubMed (2016-2021); Embase via Elsevier (2016-2021); Google Scholar (2016-2021); LILACS (2016-2021); and handsearch at the Central Library of UNIFESP (2019-2021). Psoriasis AND Women OR Woman as MeSHs.
Eligibility Criteria:
Inclusion criteria:
Type of Study: Original articles, systematic reviews, meta-analyses, and case reports about psoriasis in women.
Target Population: Women with psoriasis researches.
Clinical Aspects: Clinical, psychological, with social-economic implications of women with psoriasis.
Language: English, Portuguese, Spanish.
Publication Period: Published studies from 2016 to 2021.
Exclusion Criteria:
Target Population: Type of Study: All others studies.
Study Quality: Studies without a standard of methodological MBE.
Availability: Articles whose full text is not available.
Data analysis: A comprehensive approach was used for integrity and applicability of the findings.
Assessment of risk of bias in included studies
To assess the methodological quality of such studies, Two review authors independently and in duplicate undertook the analysis. Two scales would be used, one’s, the Higgins Bias Risk Analysis Tool for Clinical Trials adopted by the Cochrane Collaboration (Higgins 2011), for Randomized Clinical Trials. Bias is assessed as a judgment (high, low, or unclear) for individual elements from five domains (selection, performance, attrition, reporting, and other) (Higgins 2011). - Generation of the allocation sequence; - Allocation secrecy;- Masking of participants and staff;- Masking of outcome evaluators;- Incomplete data;- Selective reporting;- Other sources of bias. To evaluate the methodological quality of any Quantitative Systematic Review with Meta-analysis that was eventually retrieved by the search strategy, it was also applied the AMSTAR Scale 2, (A Measurement Tool to Assess Systematic Reviews 2) (Shea 2007), one of the most accurate tools for this purpose.
Data Extraction and Synthesis:
Data was extracted from included studies about population, methodology, main findings, and conclusions. The main findings and conclusions were extracted from each study included to a standard form, and synthetized at Table 2, for a cohesive overview of the current state of knowledge on psoriasis in women, with comparing, contrasting findings and identifying common or divergent issues. The analysis also sought to identify gaps in the literature, pointing out insights for future researches.
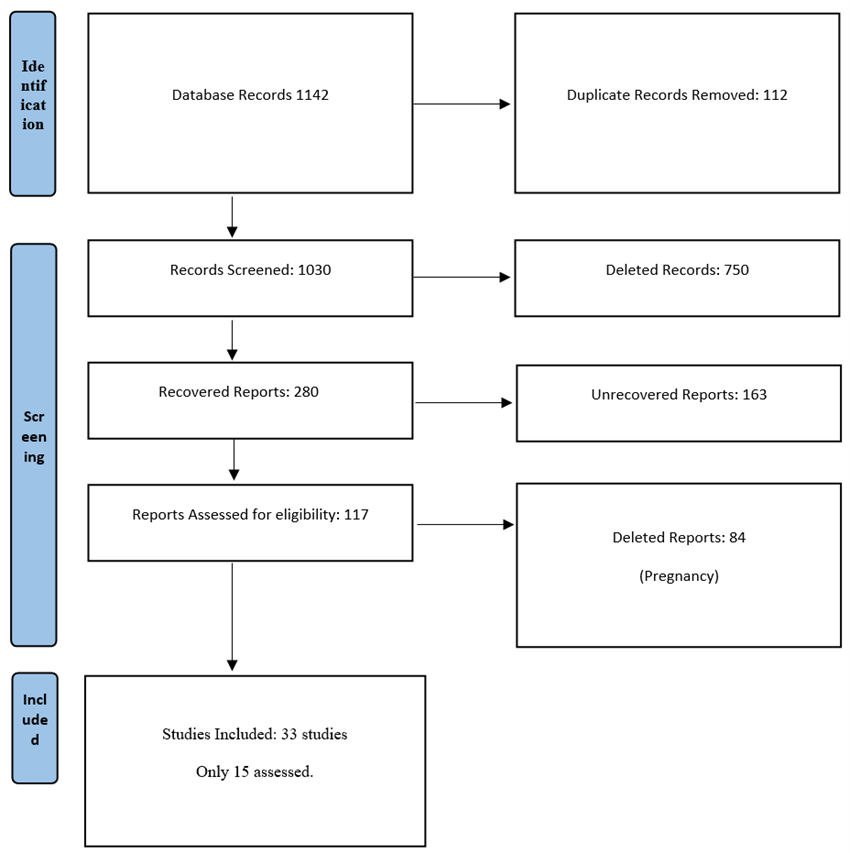
Prisma Flow
Results
From a 1,142 preliminarily eligible studies were selected, and available for full text reading, but only 33 eligibility primary studies were presented in the PRISMA flowchart (Table 1) and detailed at (Table 2).
Table 2: Different Interventions, Outcomes, Satisfaction and Reproduction:
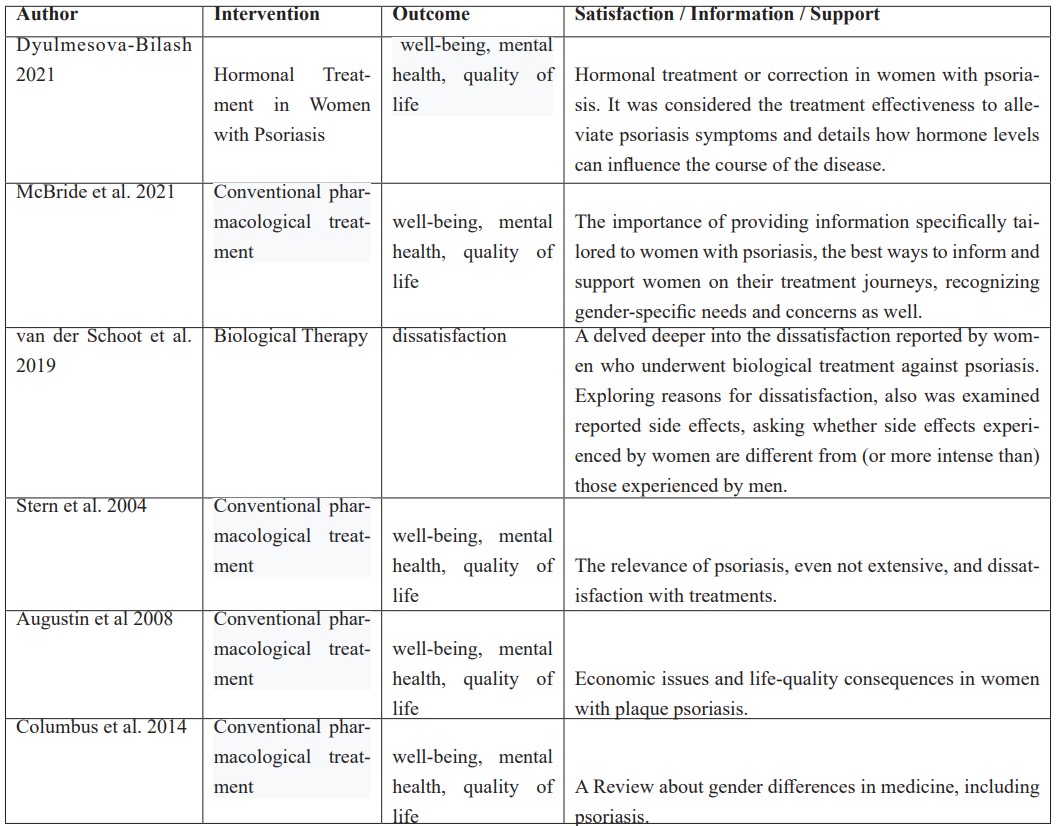
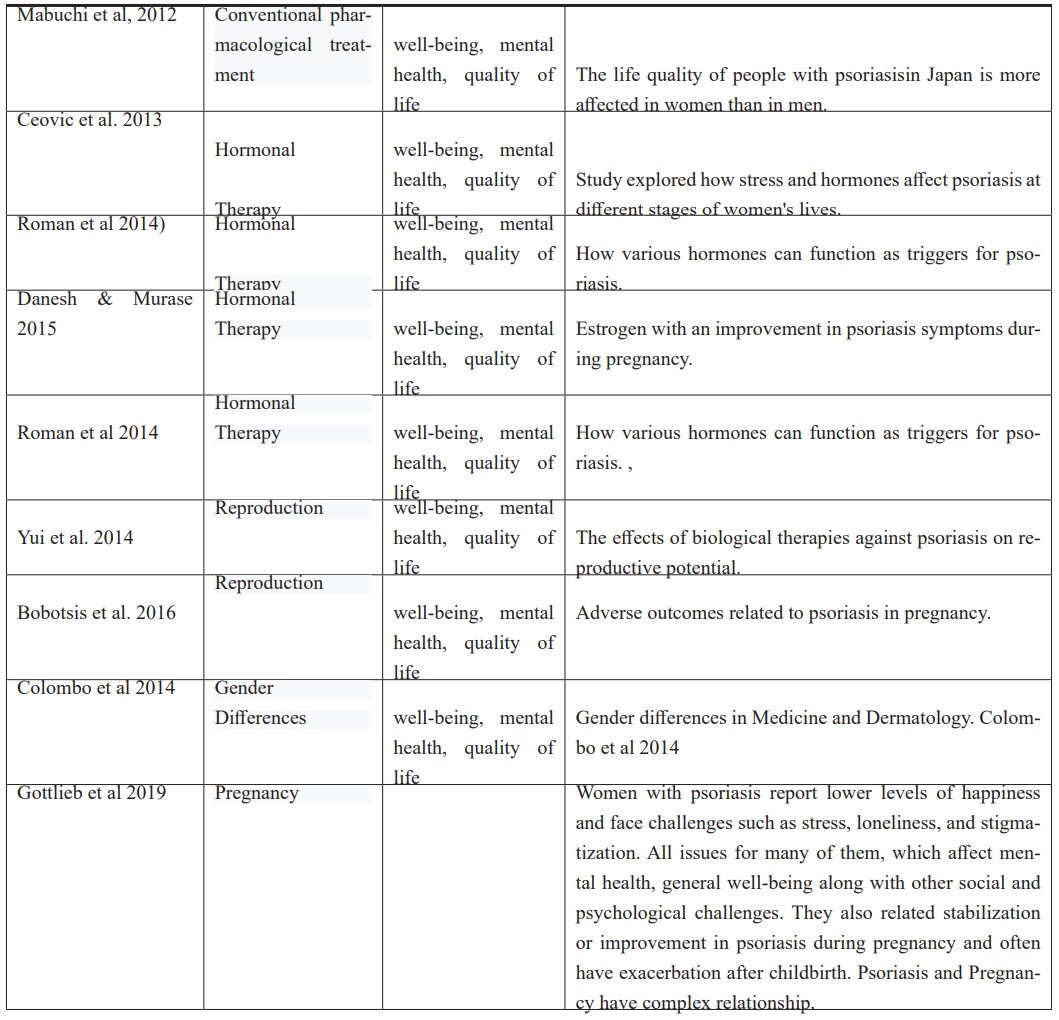
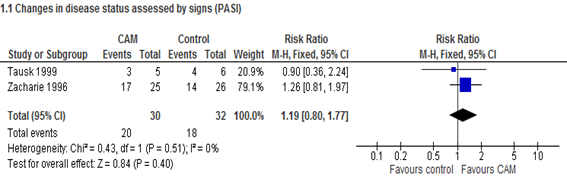
Also, it was found 2 Cochrane Systematic Review with metanalisis [18,19], and one Systematic Review Protocol [16], on well-being, quality of life, mental health, women's health and complementary therapies for psoriasis, all of them with high methodological quality, but with primary studies included with a high level biases.All, however, with meta-analyses in favor of clinical decision-making that takes into account providing well-being for women, with a view to increasing levels of mental health and quality of life, with resources from complementary therapies applied as a co-intervention to conventional therapies.
Holistic approaches help optimize treatments for psoriasis in women, in terms of physical, emotional and social impacts [16,17]. For instance, the present metanalysis on the applicability of hypnosis for psoriasis. despite the low quality of the evidence obtained, resulting from the low quality of randomized clinical trials and which even so had a minimum quality to be included in the present meta-analysis. Complementary Holistic Integrative Therapies were used in the Mind/Body Practices modality with a focus on Hypnosis. Such resources were applied as a co-intervention to conventional pharmacological treatments. As a result, the diamond point points in favor of the Hypnosis intervention [16,17].
Discussion
Psoriasis is a model of chronic systemic inflammatory process on its moderate-to-severe and severe forms, the serious repercussions on the quality of life and social and work performance [8].
Considering the valuable indicator of co-morbidities of psoriasis, the restriction of its knowledge among to clinical dermatologists is astonishing. The absence of minimum skills to face cardiovascular, metabolic, and psychiatric complications. Co-morbidities are usually under diagnosed and frequently progress and worsen without adequate treatment [11]. These flaws underwent a progressive and deep change over time. Psoriasis is no longer considered an almost strictly dermatological disease. It was treated with different topics (many of them were of popular tradition, smelly, and overlapped with the discomfort of pearly flaking and repulsive-looking plaques) until it was revealed as a systemic disease of cardiovascular, metabolic, psychiatric, and/or psychosomatic involvement, especially in moderate-to-severe and severe presentations [6,9]. The systemic, restricted, and tightly controlled treatment (methotrexate, cyclosporine, and acitretin) was insufficient to completely alleviate the discouragement. However, it became promising (with due reservations), returning to a full social life for people with access to first-line drugs, the so-called biological products [1,2]. The concept of systemic inflammatory disease began to spread internationally and specialists from related areas have become familiar with the relationships between psoriasis and risky pathological states: diabetes, hypertension, hyper-lipidemia, cardiovascular diseases, oral diseases, distress, anxiety, depression, sleep disorders, sexual dysfunctions, alcoholism, and drug abuse [3,4]. It’s important to recognize the general suffering experienced by women, including more intense than in men in the same condition and women with equally important illnesses [5]. The dysfunctional metabolic conditions (dyslipidemia, obesity, and diabetes), women with psoriasis are more subject to drug addiction when discouragement and the difficulty of containing the disease outweigh the positive aspects of their behavior (women have greater chance of adhering to treatments in comparison to men). Feelings of isolation, humiliation, and disgust underlie the deterioration in the mental health of women who face deformation of self-image and loss of the will to live. Social and family losses can result from the lack of receptivity for these women by structures that should identify the critical situation and build satisfactory viable solutions [2]. The psychological damage associated with psoriasis in its moderate and severe forms is related to damage intensity, which can lead to despair and suicidal ideation. Psoriasis has also come to induce serious psychosomatic and somatic disorders that feed on themselves [13]. Data were incisive and decisive regarding the systemic risks that harm the quality of life and the importance of the mental health of women with psoriasis in any age and hormonal (procreative or not) range. Thus, the importance of dermatologists is crucial, but their experiences do not reach the skills of endocrinologists (diabetes and nutrition), cardiologists (myocardial infarction, arterial hypertension, and hyperlipidemia), and psychologists and/or psychiatrists (stress, depression, suicidal ideation, and tendency to alcoholism), but have to made the difference [10]. Specialists must to consider psoriasis as a public health with an important risk marker of general health and psychophysical well-being aspects that should be considered in women's health programs. There is little doubt that women are an appreciable contingent of people subjected to a greater burden of suffering in comparison to other injuries of the same dimension, but not visible, not externalized to public judgment in everyday life and not subject to daily scrutiny with all consequent stress overloaded [13].
Practical Implications
1) Psoriasis is not a disease restricted to the dermatologists but it is well defined as a paradigm of systemic inflammatory disease that severely compromises the quality of life, mainly for women;
2) Psoriasis (moderate-to-severe forms) is linked with serious comorbidities, and must be controlled: metabolic syndrome, obesity, diabetes, high blood pressure, myocardial infarction, alcoholism, depression, oral health and other psychic disorders, requires monitoring; Psoriasis is an indicator of comorbidities that requires multidisciplinary attention;
3) Programs of differentiated attention to women with psoriasis as a function of comorbidities, fluctuations, and hormonal influences in the course of life are seminal.
4) Precise diagnosis and recognition of psoriasis must be disseminated across medical specialties, emphasizing its role as a systemic inflammatory disease model aiming to reduce the risks and consequences awareness of insufficient of comorbidities.
5) Evidences point that appropriate treatment of women with psoriasis can reduce associated comorbidities.
6) Mind & Body Therapies approaches help optimize treatments for psoriasis in women, in terms of physical, emotional and social impacts improving levels of mental health, well-being and quality of life [16,17].
Research Implications: Better studies for news concerns such as women and psoriasis.
References:
- Puchner, et al. Immunosuppressives and biologics during pregnancy and lactation: A consensus report issued by the Austrian Societies of Gastroenterology and Hepatology and Rheumatology and Rehabilitation. Wien Klin Wochenschr, 2019; 131(1-2): 29-44. doi: 10.1007/s00508-019-1448-y.
- Griffiths, et al. Psoriasis - Seminar. Lancet, 2021; 397(10281): 1301-1315. doi.org/10.1016; SO140-6736(20)32549-6.
- World Health Organization. Global report on psoriasis. Geneva, Switzerland: World Health Organization, 2016.
- Elmets, et al. Joint AAD-NPF guidelines of care for the management and treatment of psoriasis with awareness and attention to comorbidities. J Am Acad Dermatol, 2019; 80(4): 1073-1113.
- The burden of psoriasis: a call for awareness. e-Clinical Medicine. Part of The Lancet, 2021; 38: 101114. org/10.1016/j.eclinm.2021.101114.
- Romiti, et al. Prevalence of psoriasis in Brazil - a geographical survey. Int J Dermatol, 2017; 56(8): e167-e168. doi: 10.1111/ijd.13604. Epub 2017 Mar 27.
- Dyulmesova, et al. Clinical considerations for the management of psoriasis in women with disorders of the menstrual cycle. Journal of Education, Health and Sport. Online, 2021; 11(9): 816-827. DOI: 10.12775/JEHS.2021.11.09.097.
- McBride, et al. Impact of psoriatic disease on women aged 18 to 45: Results from a multinational survey across 11 European countries. Int J Womens Dermatol, 2021; 7(5Part B): 697-707. doi: 10.1016/j.ijwd.2021.08.011.
- Murer, et al. Gender differences in psoriasis: a Swiss online psoriasis survey. Arch Dermatol Res, 2021; 313(2): 89-94. doi: 10.1007/s00403-020-02066-1.
- Tokuyama, et al. New Treatment Addressing the Pathogenesis of Psoriasis. Int J Mol Sci, 2020; 21(20): 7488. doi: 10.3390/ijms21207488.
- Gottlieb, et al. Clinical considerations for the management of psoriasis in women. Int J Womens Dermatol, 2019; 3: 141-150. doi: 10.1016/j.ijwd.2019.04.021.
- Van der Schoot, et al. Female patients are less satisfied with biological treatment for psoriasis and experience more side-effects than male patients: results from the prospective BioCAPTURE registry. J Eur Acad Dermatol Venereol, 2019; 33(10): 1913-1920. doi: 10.1111/jdv.15733.
- Mehrmal, et al. Identifying the prevalence and disability-adjusted life years of the most common dermatoses worldwide. J Am Acad Dermatol, 2020; 82(1): 258-259. doi: 10.1016/ j.jaad.2019.09.066. doi: 1016/ j.jaad.2019.09.066
- Ko, et al. Lifestyle changes for treating psoriasis. Cochrane Library, 2019. https://doi.org/10.1002/14651858.CD011972.pub2
- Andrade, et al . Interventions for chronic pruritus of unknown origin. Cochrane Library, 2020. https://doi.org/10.1002/14651858.CD013128.pub2
- Monson, et al. Protocol: Complementary therapies for chronic plaque psoriasis. Cochrane Database of Systematic Reviews 2014; 1(7): Article No: CD011243. DOI: 10.1002/14651858.CD011243. Copyright © 2014 The Cochrane Collaboration. Published by JohnWiley & Sons, Ltd. London / UK.
- Monson CA, Monson ASC. Terapias Complementares para o Paciente Crônico na Perspectiva da Saúde Baseada em Saúde Baseada em Evidências. Primeira Edição. Appris Editôra, 2019.
- Ko SH, Chi CC, Yeh ML, Wang SH, Tsai YS, Hsu MY. Lifestyle changes for treating psoriasis. Cochrane Database of Systematic Reviews, 2019; 1(7): Article No: CD011972. DOI: 10.1002/14651858.CD011972.pub2.
- Andrade A, Kuah CY, Martin‐Lopez JE, Chua S, Shpadaruk V, Sanclemente G, et al. Interventions for chronic pruritus of unknown origin. Cochrane Database of Systematic Reviews, 2020; 1(1): Article No: CD013128. DOI: 10.1002/14651858.CD013128.pub2.

