Coexistence of Sacroiliitis and Facet Joint Syndrome in an Aged Lady of Sjögren’s Syndrome: Unexpected Involvement of Symphysis Pubis
Chun-Yi Lin1, Ta-Chung Chao2, Chuang-Hsin Chiu3,4 and Shin-Tsu Chang2,5,*
1School of Medicine, National Defense Medical Center, Taipei, Taiwan
2Department of Physical Medicine and Rehabilitation, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taipei, Taiwan
3Department of Nuclear Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan
4Institute of Medical Science, National Defense Medical Center, Taipei, Taiwan
5Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
Received Date: 12/09/2024; Published Date: 30/10/2024
*Corresponding author: Dr. Shin-Tsu Chang, MD, MS, PhD, Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital; Department of Physical Medicine and Rehabilitation, School of Medicine, Tri-Service General Hospital, National Defense Medical Center, Taiwan
ORCID number of STC: 0000-0003-4005-209
Abstract
Primary Sjögren's Syndrome (SS) often leads to systemic manifestations that primarily involve the musculoskeletal system, predominantly affecting peripheral joints. Involvement of the axial skeleton is less common. We report a 68-year-old lady with a 14-year history of chronic lower back and lumbar pain, diagnosed as SS ten years ago. She was also diagnosed with bilateral sacroiliitis and lumbar facet joint syndrome through skeletal scintigraphy. While these conditions are often attributed to age-related degeneration, SS could play a significant role. Additionally, we unexpectedly identified a lesion in the symphysis pubis, an area not previously associated with SS in the literature to our knowledge.
Keyword: Sjögren’s syndrome; Sacroiliitis; Facet joint; Symphysis pubis; Pubalgia; Fortin finger sign; Stork test; Scintigraphic rehabilitation
Introduction
Primary Sjögren's Syndrome (SS) is a persistent autoimmune disease that primarily impacts the exocrine glands, leading to their infiltration by lymphocytes and a surge in B cell hyperactivity. SS often exhibits underlying features such as increased levels of immunoglobulins in the blood and a variety of serum autoantibodies. These autoantibodies include antinuclear antibodies, rheumatoid factor, and cryoprecipitate immunoglobulins. Particularly significant are antibodies of the ribonucleoprotein complexes Ro (SS-A) and La (SS-B), which serve as hallmarks of SS [1,2].
Broadly speaking, chronic lower back pain (LBP) is a chief reason of disability and significantly diminishes the quality of life [3]. Facetogenic chronic LBP, also known as lumbar facet joint (LFJ) syndrome, affects around 15% - 41% of patients suffering from LBP [4,5]. Additionally, sacroiliitis is also an important and significant contributor to LBP that cannot be overlooked [6]. The sacroiliac (SI) joint is one of the largest joints in human to connect the ilium to the sacrum, and its inflammation commonly causes pain in the buttom and lower back region and frequently shows similarity to many other back pain sources. Sacroiliitis, a leading sign of LBP, should be considered and diagnosed first before emergence of other conditions. Sacroiliitis can be primarily due to chronic degeneration, or be secondary to rheumatologic, stress, infectious, drug-related, or oncologic factors. Osteitis condensans ilii, a sacroiliitis-like disorder, can cause sciatica [7]. Rheumatology-related disorders leading to sacroiliitis may stem for ankylosing spondylitis, primary psoriatic arthritis, Behçet’s disease, hyperparathyroidism, post-streptococcal infections, or even bottom-up from periostitis [8-13]. However, secondary causes of sacroiliitis are rarely associated with SS. Further, the disorder of symphysis pubis is a notably rare condition.
We herein present a lady with SS who showed lesions involving the axial skeleton, including the vertebral arch, lumbar facet joints, bilateral SI joints, and the symphysis pubis.
Case Presentation
A 68-year-old female housewife presented with several years of lower back and lumbar pain. Her lower back pain history extends back fourteen years. Ten years ago, she was diagnosed as SS, exhibiting symptoms of severe dry eyes and mouth for several months and a positive sialoscintigraphic scan. She also experienced morning stiffness in both hands and pain in the proximal interphalangeal joints (PIPs) for years. Additionally, she reported numbness in her left hand and was diagnosed with autoimmune thyroiditis. Laboratory data revealed that her anti-Ro 60 levels were elevated to 20.0 as of last year (with a reference value of 10.0), Table 1.
In the outpatient evaluation for her lower back and lumbar pain, due to her chronic and long-standing pain and positive Fortin finger sign and Stork test, there were a suspicion of sacroiliitis and LFJ syndrome. Therefore, a skeletal scintigraphy using Tc-99m methylene diphosphonate (MDP) was conducted, which showing high sensitivity for early detecting bone/joint lesions [14-17]. There was increased uptake (hot spots) in the lumbosacral spine and SI joints on whole body bone scan (Figure 1), and identified hot spots in the LFJs (Figure 2), bilateral SI joints, vertebral arch (Figure 3) and the symphysis pubis (Figure 4) on Single-Photon Emission Computed Tomography-Computer Tomography (SPECT-CT). The Quantitative SI Scintigraphy (QSS), one of skeletal scans for differentiating the chronic LBP as rheumatology- or stress-related origins [18,19], showed the sacroiliac joint-to-sacrum ratio on both sides ranging from 1.02 to 1.22 (Table 2). Those findings together with medical history and positive clinical testing confirmed the diagnosis of bilateral sacroiliitis and LFJ syndrome. Consequently, she was prescribed centrally acting skeletal muscle relaxants (Mocolak tablets 400 mg, TID) for 12 days. Additionally, she underwent various therapeutic modalities, including low-level laser therapy and interferential current therapy.
Table 1: ANA: antinuclear antibody; anti-SSA: anti-Sjögren’s syndrome-related antigen A; anti-SSB: anti-Sjögren’s syndrome-related antigen B.
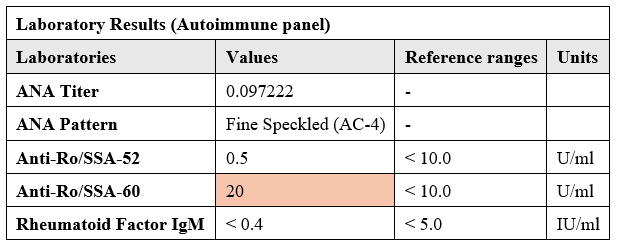
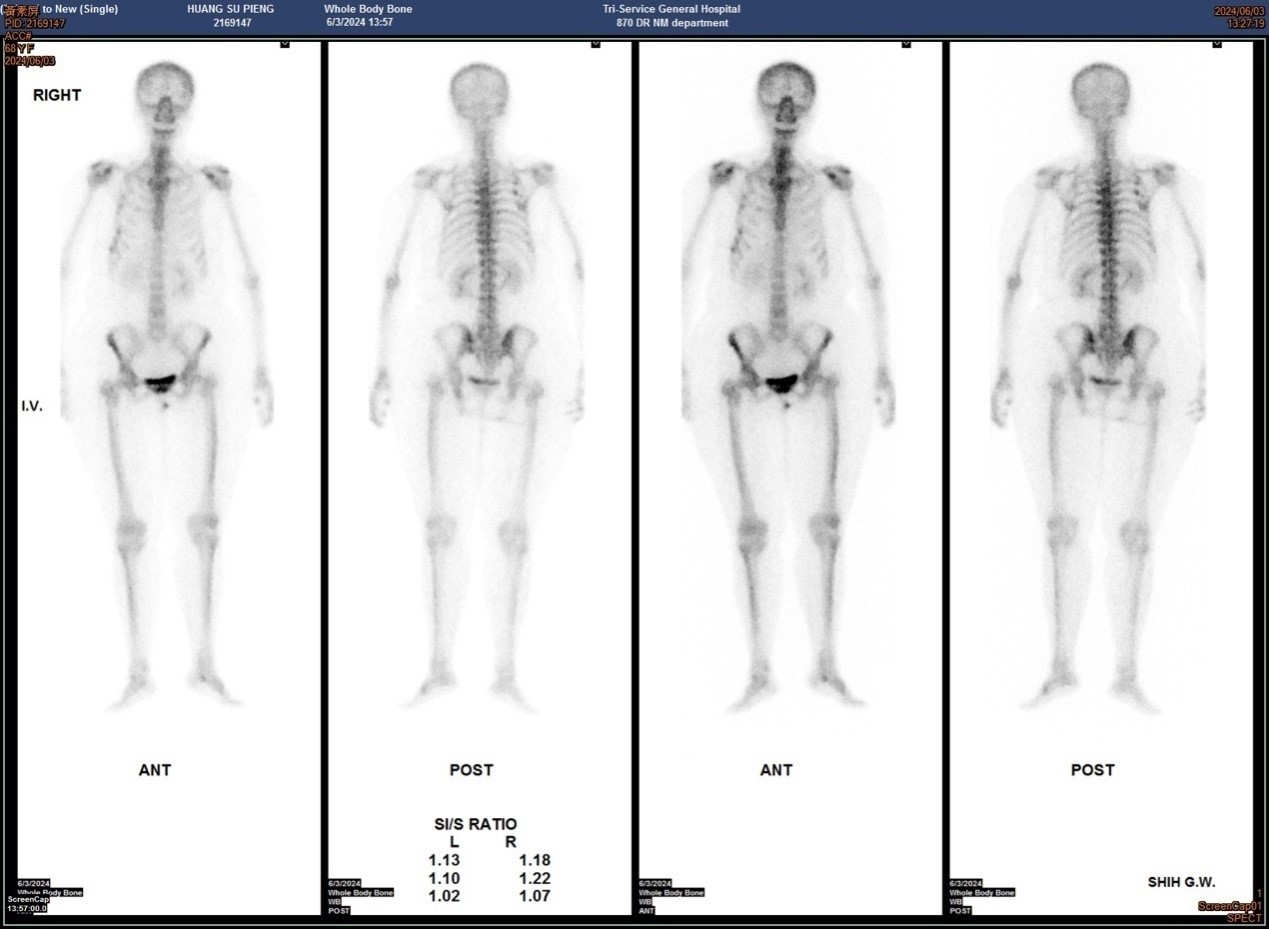
Figure 1: Whole body bone scan (WBBS) of our case. A, B is the radioactivity image after the Tc-99m MDP was injected intravenously 4 hours later. A is anterior view and B is posterior view. The red circles represent the unusual uptake of the radiotracers, which can be observed at lumbosacral spines and sacroiliac joints.
Table 2: Notes: Early arthritis corresponds to radiographic grade I-II.Late arthritis corresponds to radiographic grade III-IV. Data collected from Nuclear Medicine Annual 1983.
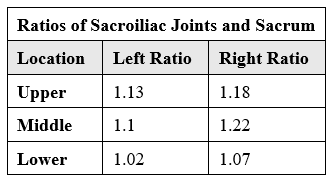
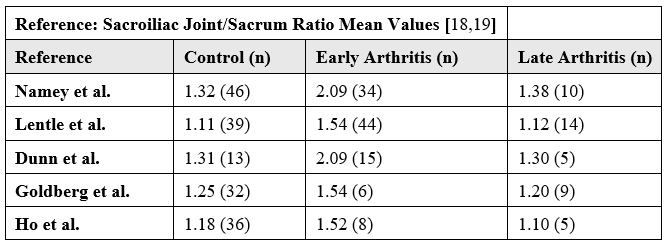
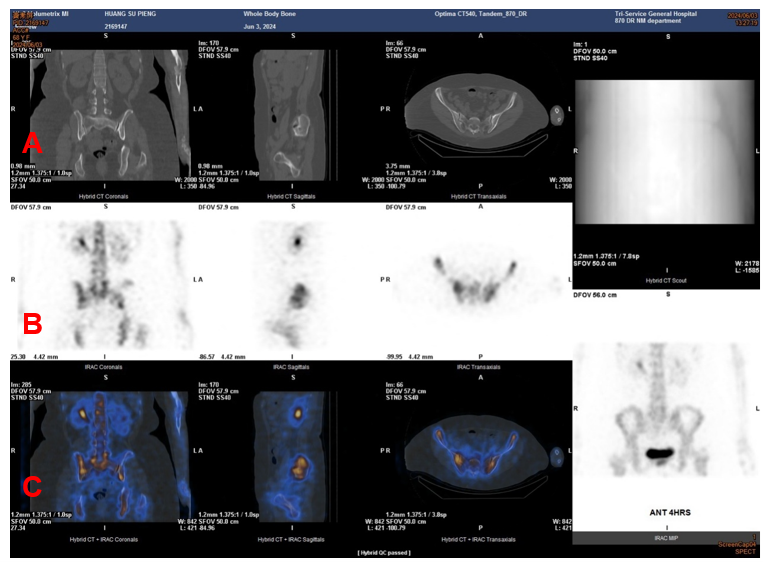
Figure 2: Skeletal scintigraphy with hybrid images of SPECT/CT of the patient’s spine. (A) CT scan films of the pathologic lumbar facet joints and both sacroiliac (SI) joints. (B) Bone scan images with noticeable pathologic spine in black. (C)SPECT/CT image with significantly increased bone turnover at the the lumbar facet joints and both sacroiliac (SI) joints.
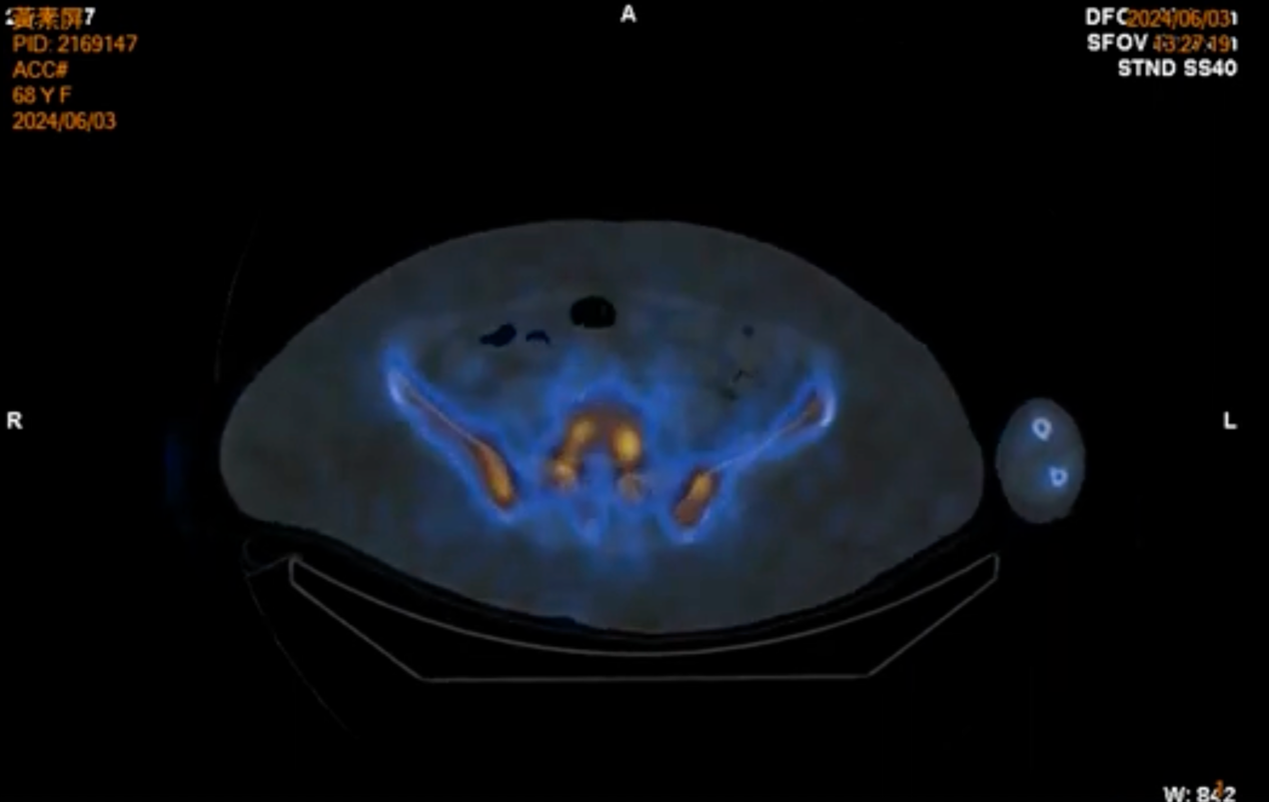
Figure 3: The SPECT/CT scan reveals pathological changes in the vertebral arch and bilateral sacroiliac (SI) joints, both of which show increased radiotracer uptake (Red arrow).
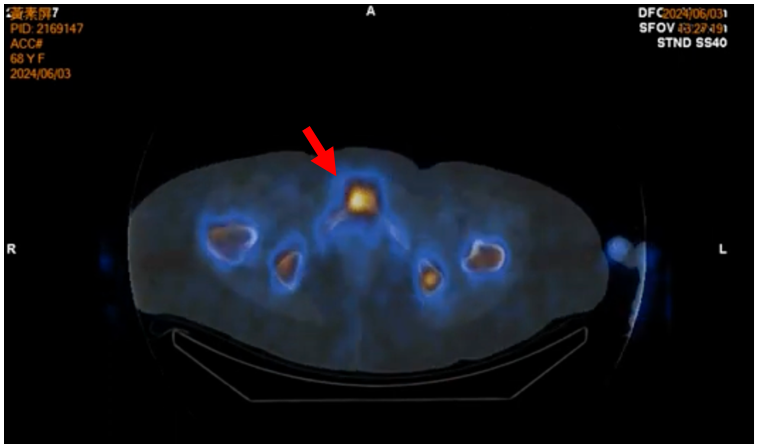
Figure 4: The enhancements of the hybrid SPECT-CT at the symphysis pubis confirmed the lesion. (Red arrow).
Discussion
Our case of SS presented with LBP, and upon examination, multiple lesions were identified in the axial skeleton, including the LFJs, bilateral SI joints, and vertebral arch. To our surprise, an inflammatory lesion was also found in the symphysis pubis. To our knowledge, this is the first case having such findings.
Systemic manifestations of SS encompass various systemic organs and tissues, including the musculoskeletal system [20]. SS often leads to systemic manifestations that primarily involve the musculoskeletal system, specifically tissues of bone, joint, synovium, and cartilages, with sparing the musculacture [21]. Additionally, the significant prevalence of thyroid disease in those SS implicates potential disruptions in bone and cartilage metabolism, calling for more detailed analysis. In patients with SS, 96% experience peripheral joint pain, while 1.8% develops arthritis. Reports indicate that arthritis rates can be as high as 70% [22,23]. In our case, the patient also presented with peripheral joint pain, including morning stiffness in both hands and chronic pain in the PIPs for years. Additionally, our patient exhibited axial skeleton involvement, a condition that is relatively rare among those with SS. Although sacroiliitis and facet joint syndrome could potentially be attributed to age-related degeneration [5,8-10,24], several factors raised the possibility that SS may play a significant role in the coexistence of these conditions like our case. We will explore these factors in detail in the following discussion.
With respect to the facet joint syndrome, the LFJ is unique as the only pure synovial joint within the spine, undergoing a degenerative course akin to that observed in appendicular joints, which course encompasses the changes in joint capsule, subchondral bone, cartilage, synovium, and adjacent soft tissues [24]. Therefore, it is plausible that SS may also lead to the development of LFJ syndrome, as synovitis in appendicular joints is a common symptom of SS. Moreover, the primary etiology of the facetogenic pain is degenerative osteoarthritic changes of the facet joint, which condition is intimately linked to the degeneration of the spinal discs, a process often correlated with significant physical labor performed before the age of 20 [24]. Our patient is a housewife with no history of heavy labor or intervertebral disc degeneration, we have excluded these mentioned common causes, leading us to consider that SS may play a key role in the development of her skeletal disorders.
Next, we address the characteristics of sacroiliitis. The coexistence of Inflammatory Back Pain (IBP) and SS was first described in 2006 by Chang et al. [26], who identified this coexistence as an unusual discovery. Eren et al. [27] found lately that patients with primary SS had a elevated prevalence of IBP (24.7% vs. 4%) and sacroiliitis (10.5% vs. 2%) compared to controls. Ankylosing spondylitis is the primary disorder associated with IBP and sacroiliitis [28,29]. However, our case developed sacroiliitis in the absence of ankylosing spondylitis and with negative HLA-B27 status, suggesting that SS may contribute to the development of sacroiliitis.
This case is notable for identifying a symphysis pubis lesion via SPECT/CT imaging. While the etiology of osteitis pubis (pubalgia) is unclear, it is commonly linked to repetitive trauma and shear forces across the symphysis pubis in athletes [30-34], often due to opposing forces from the rectus abdominis muscles and the adductor longus during activities like kicking or rapid directional changes [35]. It is widely accepted that lesions in the symphysis pubis are closely related to the muscles attached to this anatomical site. Traditionally, osteitis pubis is observed more frequently in men than in women, with previous studies indicating a prevalence 2 to 5 times higher in men [36]. Notably, our patient is a non-athletic female housewife, making it challenging to attribute her symphysis pubis lesion to the athletic-related causes. This necessitates consideration of other, less common pathological conditions. In this context, it is plausible that the lesion may be associated with SS, suggesting a potential impact of SS on the axial skeleton that has not been extensively recognized.
However, there are some contradictions to consider. Firstly, facet joint syndrome is characterized by cartilage erosion and inflammation [3], whereas SS typically leads to non-erosive synovitis [37]. Although rare, there are instances of SS presenting with erosive arthritis, so it cannot be entirely ruled out that SS may lead to facet joint syndrome [38]. Secondly, patients with SS may develop autoimmune thyroiditis, which can result in hypothyroidism [39]. In our case, she had autoimmune thyroiditis. Thyroid hormones have been known to affect the cell proliferation and tissue differentiation of bone/cartilage cells, and the hypothyroid state appears to induce decreased bone resorption and turnover [40], which contradicts the pathological phenomena observed in facet joint syndrome. Facet joint syndrome is typified by increased subchondral bone resorption and turnover [24]. Based on the above, it is evident that the thyroiditis associated with SS is unrelated to facet joint syndrome, and SS does not affect the facet joints through this pathophysiology.
Conclusion
Although there are some facts that SS might contribute to the development of facet joint syndrome and sacroiliitis, further research is needed to verify this association. We might be able to investigate this by collecting data from patients who have all three conditions and confirming whether they developed these diseases without exposure to risk factors for degenerative arthritis. Facet joint syndrome and sacroiliitis significantly impact patients' quality of life. If SS is indeed a risk factor for these conditions, physicians should inform and work with patients who have SS early on to prevent or delay the onset of these diseases. When managing patients with SS who present with LBP, the pathology of the symphysis pubis should also be considered. Skeletal bone scan is a very useful tool in scintigraphic rehabilitation for early detection of clinical disorders.
References:
- Mavragani CP, Moutsopoulos HM. The geoepidemiology of Sjögren's syndrome. Autoimmun Rev, 2010; 9: A305-310. 10.1016/j.autrev.2009.11.004.
- Routsias JG, Tzioufas AG. Autoimmune response and target autoantigens in Sjögren's Eur J Clin Invest. 2010; 40: 1026-1036. 10.1111/j.1365-2362.2010.02342.x
- Wang JC, Le DT, Alem N. Facet joint injection. Eur Spine J, 2021; 2021: 1–13.
- Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: a study in an Australian population with chronic low back pain. Ann Rheum Dis, 1995; 54: 100–106. doi: 10.1136/ard.54.2.100.
- Tee DAG, Chang ST. Appearance of facet joint syndrome in a case of chronic sacroiliitis: Evidenced from quantitative sacroiliac scintigraphy and dual images of SPECT-CT. International Journal of Frontiers in Biology and Pharmacy Research, 2024; 05(01): 019-023. DOI: https://doi.org/10.53294/ijfbpr.2024.5.1.0028.
- Liu TJ, Chang CC, Chen LC, Chu HY, Hsu CS, Chang ST. Relationship of HS CRP and sacroiliac joint inflammation in undifferentiated spondyloarthritis. Open Medicine, 2018; 13(1): 113-118.
- Chang ST, Wu YT, Tsai IH, Chen LC, Chu HY. Relief of sciatica after sacroiliac joint injection in a female with osteitis condensans ilii. Asia Life Sciences, 2016; 25(1): 511-515.
- Slobodin G, Hussein H, Rosner I, Eshed I. Sacroiliitis - early diagnosis is key. J Inflamm Res, 2018; 11: 339-344.
- Chahal BS, Kwan ALC, Dhillon SS, Olubaniyi BO, Jhiangri GS, Neilson MM, et al. Radiation exposure to the sacroiliac joint from low-dose ct compared with radiography. AJR Am J Roentgenol, 2018; 211(5): 1058-1062.
- Gutierrez M, Rodriguez S, Soto-Fajardo C, Santos-Moreno P, Sandoval H, Bertolazzi C, et al. Ultrasound of sacroiliac joints in spondyloarthritis: a systematic review. Rheumatol Int, 2018; 38(10): 1791-1805.
- Chang ST, Ku CH, Cherng SC. Evidence-based correlation between anti-streptolysin O serum titer and sacroiliac joint disorder. The Journal of Rheumatology, 2007; 34(8): 1746–
- Chang CC, Chu HY, Chiang SL, Li TY, Chang ST. Impairment of static upright posture in subjects with undifferentiated arthritis in sacroiliac joint in conjunction with elevation of streptococcal serology. Journal of Back and Musculoskeletal Rehabilitation, 2009; 22(1): 33-41.
- Chang CC, Ku CH, Hsu CS, Chang ST. Improvement of sacroiliac joint stress bottom-up after convalesce of foot periostitis: A randomized controlled trial. Asia Life Sciences, 2016; 25(1): 137-149.
- Tee DAG, Huang TY, Lai CY, Chang ST. The utilization of single photon emission computed tomography/computed tomography (SPECT/CT) for detecting early-phase diffuse idiopathic skeletal hyperostosis. International Journal of Clinical Studies & Medical Case Reports, 2023; 26(4): 1-4. DOI: 10.46998/IJCMCR.2023.26.000645.
- Huang TY, Tee DAG, Lai CY, Chang ST. Subclinical rib fractures detected by SPECT/CT imaging in a patient with chest wall pain following a car accident. MOJ Orthopedics & Rheumatology, 2023; 15(2): 50-55. DOI: 10.15406/mojor.2023.15.00617.
- Huang YL, Chang ST. High-riding conus medullaris syndrome: a case report and literature review-its comparison with cauda equina syndrome. Tomography, 2023; 9(6): 1999-2005. doi: 10.3390/tomography9060156.
- Tung CC, Tung SC, Chang ST. Adjacent segment disease of lumbosacral spines with lower limb pain and tightness after spinal fusion: observation from SPECT/CT scintigraphy. International Journal of Research in Medical and Clinical Science, 2023; 1(2): 101-107.
- Lim ZW, Tsai SC, Lin YC, Cheng YY, Chang ST. A worthwhile measurement of early vigilance and therapeutic monitor in axial spondyloarthritis: a literature review of quantitative sacroiliac scintigraphy. European Medical Journal (EMJ) Rheumatology, 2021; 8(1): 129-139.
- Chang ST. The role of quantitative sacroiliac scintigraphy in clinical relevance: a literature review. MOJ Orthopedics & Rheumatology, 2023; 15(6): 233-237. DOI: 10.15406/mojor.2023.15.00652.
- Jonsson R, Brokstad KA, Jonsson MV, Delaleu N, Skarstein K. Current concepts on Sjögren's syndrome—Classification criteria and biomarkers. J. Oral Sci, 2018; 126: 37–48. doi: 10.1111/eos.12536.
- Saraux A, Pers JO, Devauchelle-Pensec V. Treatment of primary Sjögren's Nat. Rev. Rheumatol, 2016; 12: 456–471. doi: 10.1038/nrrheum.2016.100.
- Aksoy A, Solmaz D, Can G, Cetin P, Balci A, Akar S, et al. Increased frequency of hand osteoarthritis in patients with primary Sjögren syndrome compared with systemic lupus erythematosus. Rheumatol, 2016; 43: 1068–1071. doi: 10.3899/jrheum.150841.
- Ramos-Casals M, Solans R, Rosas J, Camps MT, Gil A, Del Pino-Montes J, et al. Primary Sjögren's syndrome in Spain: Clinical and immunologic expression in 1010 patients. Medicine, 2008; 87: 210–219. doi: 10.1097/MD.0b013e318181e6af.
- Netzer C, Distel P, Wolfram U, et al. Comparative analysis of bone structural parameters reveals subchondral cortical plate resorption and increased trabecular bone remodeling in human facet joint osteoarthritis. Int J Mol Sci, 2018; 19(3): 845.
- Perolat R, Kastler A, Nicot B, lat JM, Tahon F, Attye A, et al. Facet joint syndrome: from diagnosis to interventional management. Insights Imaging, 2018; 9(5): 773-789.
- Chang HK, Bang KT, Lee BH, Kim JH, Bae KW, Kim MJ, et al. Concurrence of Sjögren's syndrome in a patient with Chlamydia-induced reactive arthritis; an unusual finding. Korean J Intern Med, 2006; 21(2): 116–119.
- Eren R, Can M, Alibaz-Öner F, Yilmaz-Oner S, Yilmazer B, Cefle A, et al. Prevalence of inflammatory back pain and radiologic sacroiliitis is increased in patients with primary Sjögren's syndrome. Pan Afr Med J, 2018; 30: 98. doi: 10.11604/pamj.2018.30.98.15588.
- Ghasemi-Rad M, Attaya H, Lesha E, Vegh A, Maleki-Miandoab T, Nosair E, et al. Ankylosingspondylitis: A state of the art factual backbone. World J Radiol, 2015; 7(9): 236-252. doi: 10.4329/wjr.v7.i9.236.
- Chang ST. Balance impairment induced by challenged trials in HLA-B27 carriers with inflammatory back pain. Examines in Physical Medicine and Rehabilitation: Open Access, 2023; 4(4): 000593. DOI: 10.31031/EPMR.2023.04.000593.
- Radic R, Annear P. Use of pubic symphysis curettage for treatment-resistant osteitis pubis in athletes. Am J Sports Med, 2008; 36(1): 122-128. doi: 10.1177/0363546507306160.
- Wiley JJ. Traumatic osteitis pubis: the gracilis syndrome. Am J Sports Med, 1983; 11(5): 360-363. doi: 10.1177/036354658301100516.
- Williams JG. Limitation of hip joint movement as a factor in traumatic osteitis pubis. Br J Sports Med, 1978; 12(3): 129-133. doi: 10.1136/bjsm.12.3.129.
- Major NM, Helms CA. Pelvic stress injuries: the relationship between osteitis pubis (symphysis pubis stress injury) and sacroiliac abnormalities in athletes. Skeletal Radiol, 1997; 26(12): 711-717. doi: 10.1007/s002560050316.
- Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes. PAIN (Performing Athletes with Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med, 2000; 28(1): 2-8. doi: 10.1177/03635465000280011501.
- Cohen B, Kleinhenz D, Schiller J, Tabaddor R. Understanding athletic pubalgia: A Review. R I Med J (2013), 2016; 99(10): 31-35.
- Johnson R. Osteitis pubis. Curr Sports Med Rep, 2003; 2(2): 98-102. doi: 10.1249/00149619-200304000-00009.
- Guedes LKN, Leon EP, Bocate TS, Bonfigliolli KR, Lourenco SV, Bonfa E, et al. Characterizing hand and wrist ultrasound pattern in primary Sjögren's syndrome: A case-control study. Clin. Rheumatol, 2020; 39: 1907–1918. doi: 10.1007/s10067-020-04983-y.
- Carubbi F, Alunno A, Conforti A, Riccucci I, Di Cola I, Bartoloni E, et al. Characterisation of articular manifestations in primary Sjögren's syndrome: clinical and imaging features. Clin Exp Rheumatol, 2020; 38 Suppl 126(4): 166-173.
- Baldini C, Ferro F, Mosca M, Fallahi P, Antonelli A. The association of Sjögren syndrome and autoimmune thyroid disorders. Front Endocrinol (Lausanne), 2018; 9: 121. doi: 10.3389/fendo.2018.00121.
- McLean RM, Podell DN. Bone and joint manifestations of hypothyroidism. Seminars in arthritis and rheumatism, 1995; 24(4): 282–290. https://doi.org/10.1016/s0049-0172(95)80038-7

