Perianal Seborrheic Keratosis – Mimicker of Anogenital Warts
Prasad Palanisamy1,*, Kathleen Wung Bi-Lin2, Trevor Woo1 and Emile K Tan1
1Department of Colorectal Surgery, Singapore General Hospital, Singapore
2Department of Anatomical Pathology, Singapore General Hospital, Singapore
Received Date: 13/09/2024; Published Date: 30/10/2024
*Corresponding author: Dr. Prasad Palanisamy, MRCS (Ed), General Surgery Resident, Department of Colorectal Surgery, Academia @ SGH, 20 College Road, Singapore General Hospital, Singapore
Abstract
Seborrheic keratosis is a common benign skin lesion that typically affects sun-exposed areas. It classically presents as a well-demarcated pigmented plaque with a “stuck-on” appearance. However, it can occasionally occur in the skin around the perianal region and can be misdiagnosed as an anogenital wart. The authors present a case of perianal seborrheic keratosis in a 56-year-old man who presented with a slowly enlarging bilateral verrucous growth involving the skin around the perianal region of three years duration. A complete excision of the lesions was performed and histopathology confirmed the diagnosis of seborrheic keratosis. This case report highlights to fellow clinicians the diagnostic challenges of perianal skin lesions and importance of surgical excision and histopathological examination to confirm the diagnosis.
Keywords: Seborrheic keratosis; Perianal; Anogenital warts
Introduction
Seborrheic keratosis is the most common benign epithelial tumor of the skin seen in clinical practice with a high prevalence in older populations [1,2]. These lesions are generally asymptomatic and typically present as a well-demarcated exophytic plaque with warty surface and a “stuck-on” appearance [1,3,4]. It consists of immature epidermal keratinocytes [3]. On histopathology, seborrheic keratosis can be diagnosed based on the presence of acanthosis, hyperkeratosis, papillomatous architecture, keratin cysts and keratin pseudocysts [3]. Seborrheic keratosis can occur on any hair-bearing skin except on soles, palms and mucus membranes [3]. However, these lesions have a higher tendency to form on sun-exposed areas compared to non-exposed areas with the highest distribution found on the head, neck and upper limbs [5,6]. Although seborrheic keratosis can be easily diagnosed when it presents with typical features, atypical presentation might pose a diagnostic dilemma due to some morphological overlap with other skin lesions such as warts and basal cell carcinoma [2,6]. Accurate diagnosis is paramount as it avoids subjecting patients to ineffective treatments and reduces unnecessary patient stress. Seborrheic keratosis involving the perianal region is a rare atypical presentation and has not been described much in literature [7-10]. In this case report, we describe a patient with perianal seborrheic keratosis.
Case Report
A 56-year-old Indian gentleman, non-drinker, non-smoker, with a past medical history of hypertension and hyperlipidemia, presented to the colorectal outpatient clinic with bilateral large verrucous growth involving the skin around the perianal region. It started out as a small papule which then gradually increased in size over a three-year duration. There were no symptoms such as bleeding, discharge, pain or itchiness. There was no history of anal intercourse or sexual promiscuity in either of the spouse. There was also no family history of any skin disease or malignancy.
On physical examination, two well demarcated brown papillomatous lesions were seen involving the perianal skin arising from the anal verge ranging from one to five o’clock and seven to eleven o’clock (Figure 1). Both lesions measure about 4.5 x 1.5 cm. There were no surrounding skin changes around the lesions. There was no intra-anal mass felt and no inguinal lymphadenopathy bilaterally. Colonoscopy performed was unremarkable with no anal canal warts seen. Full blood count, renal function and liver function tests were within normal limits. Viral serology for HIV and Hepatitis B/C were negative.
Subsequently, the perianal lesions were excised under general anesthesia (Figure 2) and were entirely submitted for histopathological examination. Histopathology of the specimen showed skin tissue with acanthosis, papillomatosis, and a proliferation of basaloid keratinocytes forming anastomosing strands (Figure 3A and 3B). Brown pigment within the basaloid keratinocytes and pseudo-horn cysts were seen (Figure 4). Features suggestive of anogenital warts such as alternating columns of hyperkeratosis and parakeratosis, presence of koilocytes and keratohyalin granules were not identified. There was no dysplasia or malignancy. A histological diagnosis of seborrheic keratosis was made.
At two-month follow-up, patient was doing well with the wounds fully healed. He had no further recurrences seen.

Figure 1: Pre-operative photo of the lesions.

Figure 2: Post excision of the lesions.
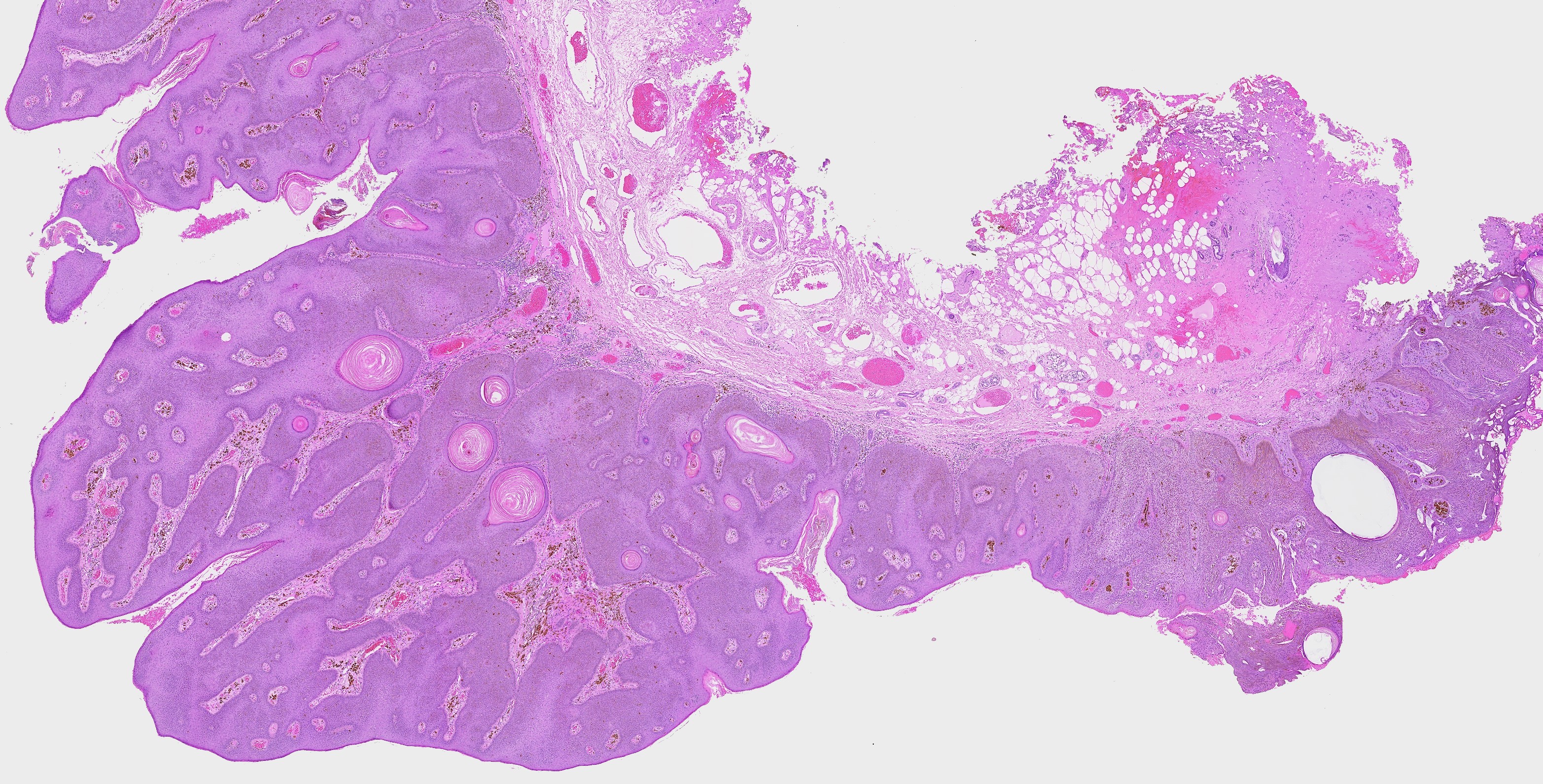

Figure 3A and 3B: Epidermal acanthosis and papillomatosis (H & E staining; Original magnification × 1).
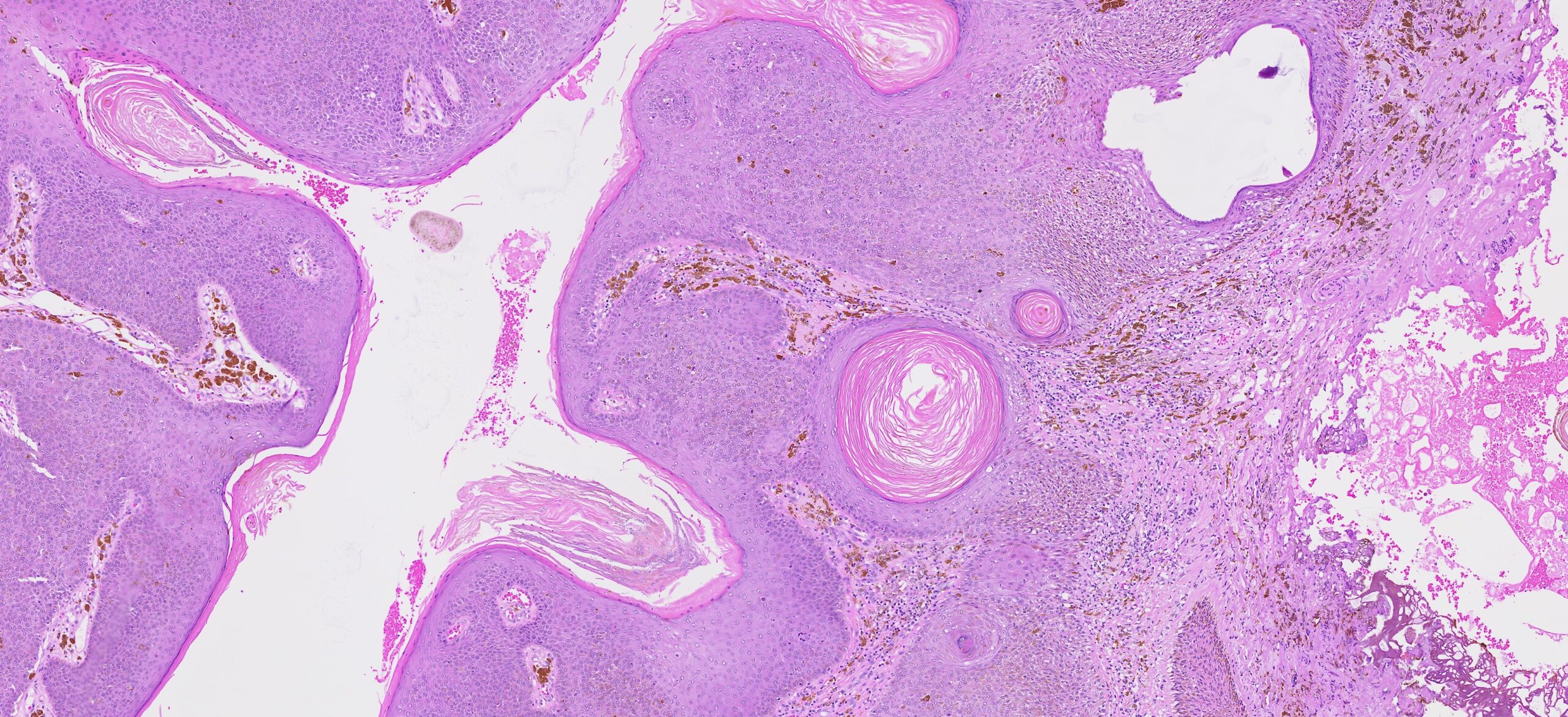
Figure 4: Pseudo-horn cysts and brown pigment within the basaloid keratinocytes (H & E staining; Original magnification × 10).
Discussion
Seborrheic keratosis is a highly common benign skin tumor with its prevalence increasing with advancing age [3, 5, 11]. Prevalence among 50-59-year-olds can be as high as 69% with both men and women being affected equally [12]. It can present with a variety of clinical morphologies but most commonly, it appears as a shiny, greasy and sharply demarcated oval shaped lesion with a verrucous surface that is fissured [3, 7]. It is usually asymptomatic. However, symptoms such as pruritus, pain and bleeding can occur particularly with lesions located in areas exposed to mechanical irritation or skin folds [11].
Seborrheic keratosis can appear on any non-glabrous surface of the body; head, neck and upper limbs having the highest incidence [1,5]. In our case, seborrheic keratosis at the perianal region is an unusual presentation with only three cases being described in literature [8-10]. Furthermore, seborrheic keratosis often tends to measure on average between 0.5 to 1.0 cm but in our case, it has a slightly larger measurement of 4.5 cm [3,6,7]. Given that it can present in an atypical manner, seborrheic keratosis can be easily misdiagnosed as other benign and malignant skin lesions including anogenital warts, basal cell carcinoma and melanoma [7,8,10,13].
As seborrheic keratosis presents mostly in a typical manner, it can be diagnosed based on clinical appearance. If there are any doubts, dermatoscopy can be used to identity horn pseudocyst and pseudofollicular openings producing a gyrus sulcus pattern, which are characteristic of seborrheic keratosis [14]. This is one of the limitations of our case as dermatoscopy was not performed. If diagnosis is still not certain, histopathological examination is required in the form of biopsy or surgical excision. The diagnosis of seborrheic keratosis can then be made based on the presence of acanthosis, hyperkeratosis, papillomatous architecture, keratin cysts and keratin pseudocysts [3].
The pathogenesis of seborrheic keratosis is not well understood despite it being a common condition. As mentioned earlier, age is one of the risk factors. Some papers have noted that genetic predisposition is a risk factor, though the exact form of inheritance has not been identified [3,15]. Another risk factor is Ultra Violet (UV) exposure. There are several papers that have shown the positive association between cumulative UV exposure and prevalence of seborrheic keratosis, particularly when comparing the population in Australia and United Kingdom [5,4]. Human Papilloma Virus (HPV) infection has also been postulated to be a risk factor but evidence is inconsistent [3,13].
Being a benign condition, there is no need for any treatment [11]. An exception to this being atypical presentation and a large lesion. In such situations, the lesion should be surgically fully excised en bloc for histopathological examination to confirm diagnosis and exclude malignancy [7]. In other situations, patients might still desire for the lesion to be removed mainly for cosmetic reasons. There are several options available such as shave excision, cryotherapy and ablative laser treatment [3]. Topical therapies have not been proven to be effective in treating seborrheic keratosis [14].
Conclusion
Seborrheic keratosis is a common skin lesion with diagnosis relatively straight forward based on its typical appearances. However, atypical presentations can result in diagnostic difficulties. Perianal seborrheic keratosis is one such rare presentation and can be easily misdiagnosed as anogenital warts. As such, a thorough histopathological examination is required to confirm the diagnosis and exclude malignancy. Complete surgical excision should be considered in these group of patients as it has both diagnostic and therapeutic benefits.
Authors Contributions:
Prasad Palanisamy: Substantial contribution to conception and design, acquisition and analysis of data, drafting of article, revising of article for important intellectual content, and final approval of the version to be published. Guarantor.
Kathleen Wung Bi-Lin: Substantial contribution to conception and design, acquisition and analysis of data, drafting of article, revising of article for important intellectual content, and final approval of the version to be published.
Trevor Woo: Substantial contribution to conception and design, acquisition and analysis of data, drafting of article, revising of article for important intellectual content, and final approval of the version to be published.
Emile K Tan: Substantial contribution to conception and design, acquisition and analysis of data, revising of article for important intellectual content, and final approval of the version to be published.
Disclosure Statement: The authors declare that they have no financial or non-financial disclosures to make.
Funding: None
Acknowledgments: None
References:
- Mary D Sun, Halpern AC. Advances in the Etiology, Detection, and Clinical Management of Seborrheic Keratoses. Dermatology, 2022; 238(2): 205-217.
- Wollina U. Recent advances in managing and understanding seborrheic keratosis. F1000Res, 2019; 8(F1000 Faculty Rev-1520).
- Barthelmann S. Seborrheic keratosis. J Dtsch Dermatol Ges, 2023; 21(3): 265-277.
- Minagawa A. Dermoscopy-pathology relationship in seborrheic keratosis. J Dermatol, 2017; 44(5): 518-524.
- Yeatman JM, Kilkenny M, Marks R. The prevalence of seborrhoeic keratoses in an Australian population: does exposure to sunlight play a part in their frequency? Br J Dermatol, 1997; 137(3): 411-414.
- Karadag AS, Parish LC. The status of the seborrheic keratosis. Clin Dermatol, 2018; 36(2): 275-277.
- Lahbacha B, Nechi S, Chaabane A, Bani A, Kchaou M, Chtourou F, et al. Seborrheic Keratosis: Report of a Rare Presentation and Reminder of the Current Knowledge of the Problem. Clin Pathol, 2024; 17.
- Salah B, Mahseeria M, Al-Alib Z, Gaitha A, Aldwana T, Al-Rawashdeh B. Giant perianal Seborrheic keratosis: A case report. Int J Surg Case Rep, 2018; 51: 296–301.
- Phiske M, Mamidwar S, Dhurat R, Jerajani HR, Randive N, Joshi M. Giant lobulated seborrheic keratosis at an unusual site. Indian J Pathol Microbiol, 2003; 46(1): 96-97.
- Stefanaki C, Rozakou A, Stefanaki K, Christofidou E, Antoniou C. Giant perianal seborrhoeic keratosis mimicking Condylomata acuminata. Int J STD AIDS, 2009; 20(3): 213-214.
- Jackson JM, Alexis A, Berman B, Berson DS, Taylor S, Weiss JS. Current Understanding of Seborrheic Keratosis: Prevalence, Etiology, Clinical Presentation, Diagnosis, and Management. J Drugs Dermatol, 2015; 14(10): 1119-1125.
- Kennedy C, Bajdik CD, Willemze R, Gruijl FRD, Bavinck JNB. The influence of painful sunburns and lifetime sun exposure on the risk of actinic keratoses, seborrheic warts, melanocytic nevi, atypical nevi, and skin cancer. J Invest Dermatol, 2003; 120: 1087–1093.
- Kaur R, Atreja CB, Singh S, Gupta S. Giant genital seborrheic keratosis: A case report and review of the literature. Indian J Case Reports, 2020; 6(5): 232-234.
- Hafner C, Vogt T. Seborrheic keratosis. J Dtsch Dermatol Ges, 2008; 6(8): 664-677.
- Hafner C, Vogt T, Landthaler M, Müsebeck J. Somatic FGFR3 and PIK3CA mutations are present in familial seborrhoeic keratoses. Br J Dermatol, 2008; 159(1): 214-217.

