A Mistreated Laryngeal Hamartoma
Ulrik Ørsø Andersen1,*, Marie Røsland Rosenørn2 and Bahareh Bakhshaie Philipsen1
1Department of Otorhinolaryngology and Maxillofacial Surgery, Zealand University Hospital, Køge, Denmark
2Department of Pathology, Zealand University Hospital, Roskilde, Denmark
Received Date: 02/09/2024; Published Date: 29/10/2024
*Corresponding author: Ulrik Ørsø Andersen, Department of Otorhinolaryngology and Maxillofacial Surgery, Zealand University Hospital, Køge, Denmark. Email: ulle08@gmail.com
Abstract
Hamartomas are tumor-like masses resulting from the focal growth of mature normal cells in a disorganized pattern. They are rarely found in the ear, nose, and throat region, with only 35 cases previously reported in the larynx. This case report presents a 49-year-old man with a two-year history of progressive stridor and hoarseness, initially misdiagnosed, and treated for asthma. Subsequent examination revealed a large obstructive laryngeal lesion, which was surgically excised. Histological analysis confirmed the diagnosis of hamartoma. This case highlights the importance of considering a laryngeal mass as a differential diagnose in patients with persistent stridor, particularly when conventional treatments fail.
Keywords: Hamartoma; ENT; Laryngeal obstruction
Introduction
A hamartoma is a tumor-like mass resulting from the focal growth of mature normal cells, but in a disorganized pattern and abnormal proportions [1,2]. They are most commonly located in the lungs, spleen, and kidneys. They rarely present in the ear, nose, and throat region and extremely rarely in the larynx. This condition can occur in both adults and children. In the larynx, the tumor most frequently presents in the supraglottic area, with the most common symptoms being stridor, dyspnea, and hoarseness. In children, poor thriving is also observed [1]. In the adult population, the aforementioned symptoms develop slowly, complicating diagnosis, which often leads to mismanagement of the disease, as in this case.
Imaging with MRI and CT will illuminate the anatomical extent of the hamartoma, but cannot provide a definitive diagnosis, which must be made histologically. Treatment is surgical and, depending on the extent of the tumor, can be endoscopic and rarely open surgery, such as laryngectomy [3]. This article aims to highlight a rare cause of a mass in the larynx and to raise awareness of this condition as a differential diagnosis for laryngeal obstruction, which can be seen in both pediatric and adult populations.
Case Report
A 49-year-old man, previously healthy, experienced progressively worsening stridor and hoarseness over a period of two years. He consulted his general practitioner, who ordered a CT scan of the thorax, which revealed no abnormalities. Suspecting asthma, the doctor-initiated treatment with an inhalation steroid and administered a Betamethasone injection, but this provided only short-term relief. The patient was subsequently seen by a private otologist, who noted both inspiratory and expiratory stridor. Fiber laryngoscopy revealed a smooth, space-occupying lesion obstructing most of the rima glottidis. The tumor moved between the subglottic and supraglottic areas during breathing. The patient was referred semi-urgently to the Ear, Nose, and Throat (ENT) clinic for further evaluation and treatment.
Shortly thereafter, he developed an upper respiratory infection and experienced worsening dyspnea, to the point where he could only breathe in a sitting position. His partner observed periods of apnea during sleep, and he was subsequently admitted via ambulance. Upon arrival, the patient was stable but had resting stridor and significant use of accessory breathing muscles. Fiber laryngoscopy revealed the previously mentioned obstructive lesion, which was obstructing 90% of the rima glottidis (Figure 1). He was treated with intravenous Solu-Medrol, adrenaline inhalations, and was closely monitored in the intensive care unit. Biochemically, his CRP was normal, but there was a slight leukocytosis with leukocytes at 11.2 x 109/L (normal range 3.5-8.8x109L). The differential count was normal.
The following day, he underwent surgery via direct laryngoscopy, which revealed a pendulous lesion originating from the cartilaginous posterior portion of the left vocal fold. The rest of the larynx and pharynx appeared normal. The tumor was excised and submitted to histological examination. The histological examination showed a rounded soft tissue tumor that was well delineated but without actual encapsulation. The bulk of the tumor was a tight mass of small eosinophilic spindle cells with a tendency towards parallel arrangements. Scattered rounded myxoid clearings occurred throughout the tumor with apparent chondroid differentiation in one of those. The walls of the blood vessels were hyalinized to some extent. A few glands and scattered fat cells were incorporated in the tumor. There was no inflammation and no necrosis. The tumor cells showed a peculiar immunohistochemical profile with concurrent expression of S100, CD34 and Desmin. There was no expression of STAT6, CK-AE, Caldesmon, Actin, EMA, HMB45, SOX10, GLUT1 or Neurofilament and the expression of TRIMH and INI-1was normal. There was no mitosis in PHH3. Furthermore, there was no mutations by NGS analysis using the Oncomine Childhood Cancer Research assay, which includes RB1 and DICER1. In conclusion the process was considered benign and harmatomatous (Figure 2). At subsequent follow up the patient was asymptomatic, but he has declined follow-up with fiberlaryngoscopy and further check-ups. Thus, it has not been possible to assess the postoperative laryngeal conditions.

Figure 1: Inspection via fiberlaryngoscopy of the hypopharynx and endolarynx revealed an obstructive tumor with a smooth, light pink mucosa. The tumor originates from the left vocal fold and obstructs the rima glottidis.
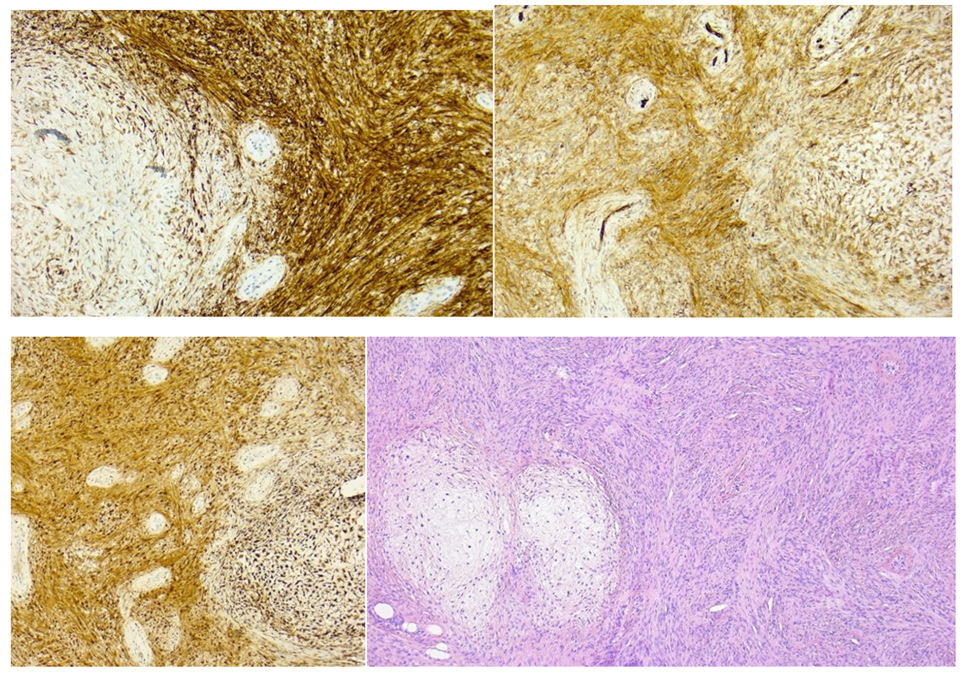
Figure 2: Microscopic pictures of the removed tissue – laryngeal harmatoma. Figure 2A shows rounded myxoid areas surrounded by a dense mass of small eosinophilic spindle cells, with somewhat parallel orientation and slightly palisading nuclei. At the right, a few small blood vessels with thickened walls are present. HE stain. Figure 2B, 2C and 2D shows immunohistochemical staining for respectively S100, CD31 and Desmin.
Discussion
Obstruction of the larynx can cause stridor, and acute onset is most often caused by foreign bodies, edema, or infections. A more gradual onset of obstruction-based stridor can be caused by conditions such as benign or malignant tumors.
Hamartomas are very rarely seen in the ENT throat region, with only 35 cases previously described in the larynx [3]. Hamartomas, in general, can arise from any organ – most commonly in the lungs, liver and spleen - and consist of mature cells arranged in a disorganized pattern and abnormal proportions [2]. A malignant progression or metastasis has not been described before in laryngeal harmartomas [2]. Laryngal hamartomas is typically present in children with an average age of about 2 years and in adults with an average age of about 50 years and there is a male predominance [1,3]. The most common symptoms are stridor, dysphonia, or airway obstruction [2], as in this case: the laryngeal hamartoma caused slowly progressing airway symptoms, culminating in persistent stridor and sleep apnea. This clinical presentation makes an early diagnosis difficult with great risk of misjudgment and mistreatment as in this case, where inhalation medication for asthma was attempted.
The treatment for hamartomas is surgical. Based on the extent, which can be visualized with CT and MRI scans, surgical treatment can be planned. Most often, hamartomas are removed endoscopically, for example, by microlaryngeal surgery with laser [4]. For large hamartomas, partial or total laryngectomy has been described [3].
Patients presenting with persistent stridor that does not respond to standard therapeutic interventions, including inhaled medications and antibiotics, should undergo evaluation by an otolaryngologist. In such cases, laryngeal hamartoma should be included in the differential diagnosis.
Acknowledgment: Special thanks to Søren Daugaard, MD, Department of Pathology, Copenhagen University Hospital, Rigshospitalet, Denmark, for the histological description.
References:
- Windfuhr JP. Laryngeal hamartoma. Acta Oto-Laryngologica. marts, 2004; 124(3): 301–308.
- Ucar S, Zorlu P, Yildirim I, Metin O. Hamartoma of the Larynx: An Unusual Cause of Stridor. Balkan Med J, 2015; 31(4): 349–351.
- Veselski Krajinović K. Rare Laryngeal Hamartoma: A Case Report. ACC, 2022.
- Mäkitie AA, Lehtonen H, Aaltonen LM, Bäck L, Leivo I. Hamartoma of the Larynx: An Unusual Cause of Dyspnea. Ann Otol Rhinol Laryngol, 2003; 112(10): 841–843.

