Cemented Modular Bipolar Hip Hemiarthroplasty: Outcomes in Elderly with Femoral Neck Fracture
Vishnudharan Nagarajan*, Prabhu Ethiraj and Siyad M Nazar
Department of Orthopaedics, India
Received Date: 05/09/2024; Published Date: 29/10/2024
*Corresponding author: Vishnudharan Nagarajan, Department of Orthopaedics, India
Abstract
Background: Femur neck fractures are a common occurrence in rural areas. Hemiarthroplasty is used to treat older patients since they have low bone quality, a reduced ability to mend, and associated co-morbidities that would not necessitate repeated treatments if the initial osteosynthesis fails. In India, research on the radiological and functional results of stand-alone cemented modular bipolar hemiarthroplasty hip is extremely few.
Aim: To analyze the functional results of a cemented modular bipolar hemiarthroplasty in a fractured neck of the femur using the Harris hip score.
Method and Materials: This Prospective study was conducted fromDecember 2020 to July 2022. Patients admitted in Orthopaedics ward from Emergency medicine department and Outpatient department at R. L. Jalappa Hospital and Research centre, attached to Sri DevarajUrs Medical college, affiliated to SDUAHER university meeting the inclusion criteria were included on this study. Data analysis was done by coGuide Statistics software, Version 1.0.
Results: Majority of the patients in our study were 64.52% aged between 60-70 years, followed by 22.58% aged between 70-80 years, and 12.9% aged > 80 years. Garden stages 3 and 4 were the stages seen in our study population, with 45.16% having stage 3 and 54.84% with Garden’s stage 4. At 6th month follow up, on assessment of Harris Hip score, 38.71% had excellent score, 58.06% had good score and 3.23% had fair functional score. At first month follow up, the radiological score was excellent in 41.94% and good in the rest 58.06%. It remained the same at the 3rd month and 6th month follow ups. P value < 0.05 was indicating significance statistically.
Conclusion: It was concluded that modular bipolar cemented hemiarthroplasty gives good functional and radiological outcome in elderly patients with femoral neck fracture.
Keywords: Femur neck fractures; Cemented Modular Bipolar Hemiarthroplast; Elderly femur neck fractures and healing
Introduction
Proximal femur fracture is one of the serious health problems that affect the elderly the most [1]. The frequency of co-morbidities in seniors increases the risk of post-surgical morbidity and death in addition to lengthening the recovery period after surgery [2]. The Gardens and Pauwels methods of categorization have continued to be the gold standard for characterising femoral neck fractures and guiding surgical management [3]. Non-displaced fractures are normally treated with hip preservation, whereas displaced fractures are frequently treated with replacements [4]. The main justification for arthroplasty in patients with displaced femoral neck fractures is to avoid nonunion and avascular necrosis, which have been observed to be as high as 39% in subjects treated with screw fixation [5,6]. Hemia or Total Hip Arthroplasty (THA) are indeed the preferred therapies for mobility in elderly people. The best approach is still debatable; while THA improves function and relieves pain, it also lengthens surgery and causes more loss of blood, both of which raise the chance of death [7].
An additional inner bearing is positioned between the stem and the endoprosthetic head component in a bipolar hemiarthroplasty [8]. This design should reduce acetabular erosion, protrusion, and dislocation, in theory. Additionally, it improves hip functionality and maintains the joint's stability [9,10]. While cemented fixation has the advantage of boosting initial fixation strength in elderly people with low bone quality, cementless fixation promotes physiological fixation and can reduce cardiovascular toxicity [11]. The prosthesis in femur neck fractures may become less prone to loosening after a cemented hemiarthroplasty, but the procedure also raises the risk of emboli and lowers cardiac output while the bone cement is being introduced [12]. Uncementedhemiarthroplasties, on the other hand, take less time to complete and result in less intraoperative blood loss, but they have greater rates of complications [13].
The Harris Hip Score (HHS) was developed as an outcome metric after moulded cup arthroplasty. It is an evaluation of health-related quality of life (HRQoL) by a qualified healthcare professional that is disease- and location-specific. It was created to offer a system for assessing hip problems and available treatments. The categories that are examined include mobility, deformity rarity, performance, and pain [14].
Methodology
All patients were evaluated by detailed history, clinical examination & radiographic findings. A sample size of 31 was selected meeting the inclusion and exclusion criteria. Inclusion criteria were patients above 60 years of age and diagnosed with femoral neck fractures. Exclusion criteria were patients who are unwilling and unfit for surgery, patients with pre-existing osteoarthritis of hip. Patients had undergone cemented modular bipolar hemiarthroplasty via posterior approach after pre-anesthetic evaluation. Following surgery patients were followed up at 1st, 3rd and 6th month. At the time of follow up patient were assessed functionally and radiologically. Functionally patients were assessed using Harris hip score. Radiologically patients were assessed by the presence of acetabular erosion, superior and medial migration, subluxation and sclerosis. Radiological score and functional score were depicted as outcome parameters. Data analysis was done by coGuide Statistics software, Version 1.0
Results
A total of 31 samples included into the study. Among the study population, 20 (64.52%) participants were between 60-70 years age group, 7 (22.58%) were between 70-80 years, 4 (12.9%) were aged between >80 years (Table and graph1).
In the study population, 14 (45.16%) participants were in stage 3 and 17 (54.84%) participants were in garden’s stage 4 (Table 2 and graph 2).
In the study population, at 1st month 7 (22.58%) participants had fair functional score and 24 (77.42%) participants had poor functional score. At 3rd month 6 (19.35%) participants had excellent, 20 (64.52%) participants had good and 5 (16.13%) participants had fair functional score. At 6th month 12 (38.71%) participants had excellent, 18 (58.06%) participants were with good and 1 (3.23%) participant reported fair functional score (Table 3).
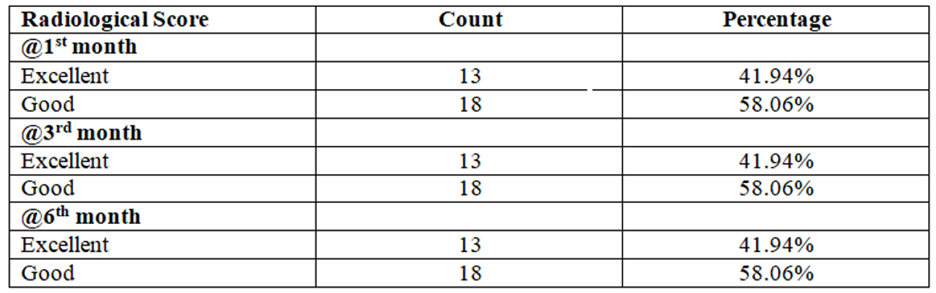
In the study population, at 1st month 13 (41.94%) participants had excellent radiological score and 18 (58.06%) participants had good. At 3rd month 13 (41.94%) participants had excellent, 18 (58.06%) participants had good radiological score. At 6th month 13 (41.94%) participants had excellent, 18 (58.06%) participants had good radiological score (Table 4).
Table 1: Distribution of Age (years) (N=31).
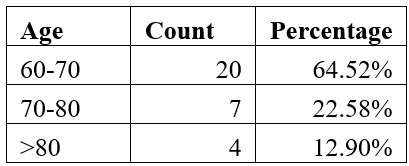
Graph 1: Bar Chart of Age groups (years) (N=31).
Table 2: Garden’s Stage distribution in our study participants (N=31).
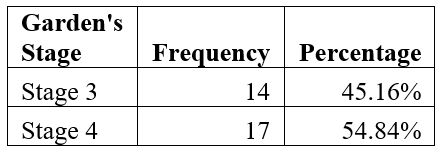
Graph 2: Pie chart of Garden’s Stage in the study samples (N=31).
Table 3: Descriptive analysis of Functional Score in the study population (N=31).

Table 4: Descriptive statistics for radiological Score (N=31).
Discussion
Majority of the study population in our study, 64.52%, are aged between 60-70 years, followed by 22.58% aged between 70-80 years, and 12.9% aged >80 years. The majority of (34.8%) study participants were aged between 71 years and 80 years, followed by 61–70 and 50–60 years age group was 30.2 and 18.7%, respectively in Ramasamy et al.’s study [15]. Rakshith Kumar et al.’s study included patients in the range of 50 to 92 years of age, with an average age of 65 years [16].
Garden type 3 and 4 fractures are seen in our study population, with 45.16% having type 3 and 54.84% with Garden’s type 4. In Sharma et al.’s study, majority had Garden type 4 fracture, followed by 40% with type 2 fracture, and 2% had type 1 [17].
On analysis of presentation to the ED after injury, 58.06% presented within 24 hours of the injury, 38.71% in the 24-48 hours’ period and 3.23% took more than 48 hours to be seen in the hospital. Majority of the patients at 21% took more than week after the injury to present to the hospital in Sharma et al.’s study. Only 8% presented within 24 hours of injury, 12% in the 24-72-hour period and 9% 72 hour to a week [17]. Adapureddi et al reported that 15% of the patients were brought to the hospital between 72 hours to 1 week and the remaining 15% presented for treatment after one week and 15% of patients after 3 weeks [18]. In our country, it is a frequent occurrence for patients to delay the hospital visit resulting in a challenging post-operative rehabilitation course.
Assessment of functional score was done using the Harris hip score and at first month follow up, 22.58% had fair functional score and 77.42% had poor functional score. At 3rd month follow up, 19.35% had excellent functional score, 64.52% had good and 16.13% had fair functional score. At 6th month follow up, 38.71% had excellent score, 58.06% had good score and 3.23% had fair functional score. Our findings were comparable with those of Sharma et al [17], Adapureddi et al [18], Ramasamy et al [15] and Rakshith Kumar et al [16]. In Sharma et al study, the mean Harris hip score at 12 months was 85.83 7.54, with 42.50% receiving an outstanding score, 37.50% a good score, 12.50% a fair score, and 7.50% a bad outcome [17]. At the final followup of 6 months, the mean Harris hip score in Ravikumar et al.’s study was 88 points with excellent results were observed in 70% cases, good in 20% cases, fair in 10% cases and poor in 0% cases [6].
At first month follow up, the radiological score was excellent in 41.94% and good in the rest 58.06%. It remained the same at the 3rd month and 6th month follow ups. In the research by Sharma et al., there was no evidence of acetabular erosion, painful stem loosening, protrusion acetabuli, or secondary osteoarthritis during the study period [17]. Ravikumar et al. reported no cases of infection, no cases of hip dislocation, no evidence of Stem subsidence, Heterotropic Ossification, Sciatic nerve palsy in any of the patients during the follow upperiod [6]. Adapureddi et al. found no late postoperative complications like loosening, dislocation, erosion, secondary osteoarthritis, protrusion acetabuli or periprosthetic fracture in their study [18].
At 6th month follow up, 83.87% complained of mild pain and 16.13% had moderate pain. Adapureddi et alstudy .'s found that of all study participants evaluated with regard to their satisfaction with the operation and their capacity to resume their pre-fracture level of activity, 35% were "extremely satisfied," 50% were "somewhat satisfied," and 15% were "not satisfied." The Harris Hip Score, an objective measurement, and the degree of satisfaction, a subjective rating, did not correspond well.[18]. Most of the participants in Ramasamy et al.’s study had a short hospital stay, less pain, no lasting limp, early mobilization, early return to pre-injury level, and a superior quality of life [15]. Rakshith Kumar et al. reported 35% of their study population had a very satisfied result with regards return to pre-fracture levels of activity, 50% had fairly satisfied result and 15% were not satisfied with the procedure [16].
The primary hypothesis of the current study is that a bipolar prosthesis with its additional artificial joint between the two components of the prosthesis offers better stability and function of the hip joint, and the cemented prosthesis helps in reduction of pain and improves mobility. This was in line with Sharma et al study's which found that cemented bipolar hemiarthroplasty offers positive outcomes in terms of range of motion, pain-free motions, return to daily activities, and independent living in older patients with fracture neck of the femur while taking the complication rates into consideration [17].
Conclusion
In this study Garden stages 3 and 4 fractures were treated with modular bipolar cemented hemiarthroplasty which resulted in excellent outcomes in majority of patients and good in the rest at 1 st month follow-up. It remained the same at the 3rd month and 6th month follow ups. So, this study demonstrates that modular bipolar cemented hemiarthroplasty gives good functional and radiological outcomes and can be considered a preferred modality of management in elderly with femoral neck fractures.
Limitations and recommendations: Our study was limited by its small sample size and lack of long-term follow-up. Due to the short follow-up, we were unable to remark on long-term effects like acetabular erosion. The Harris Hip Score was the only score used in this study to evaluate functional outcomes; however, adding additional scores would have increased the study’s overall impact.
References:
- Lizaur-Utrilla A, Serna-Berna R, Lopez-Prats FA, Gil-Guillen V. Early rehospitalization after hip fracture in elderly patients: risk factors and prognosis. Arch Orthop Trauma Surg, 2015; 135(12): 1663-1667.
- Patel KV, Brennan KL, Brennan ML, Jupiter DC, Shar A, Davis ML. Association of a Modified Frailty Index with Mortality After Femoral Neck Fracture in Patients Aged 60 Years and Older. ClinOrthopRelat Res, 2014; 472(3): 1010-1017.
- Florschutz AV, Langford JR, Haidukewych GJ, Koval KJ. Femoral Neck Fractures.J Orthop Trauma, 2015; 29(3): 121-129.
- Miller CP, Buerba RA, Leslie MP. Preoperative Factors and Early Complications Associated with Hemiarthroplasty and Total Hip Arthroplasty for Displaced Femoral Neck Fractures. GeriatrOrthopSurgRehabil, 2014; 5(2): 73-81.
- Keating J, Grant A, Masson M, Scott N, Forbes J. Displaced intracapsular hip fractures in fit, older people: a randomised comparison of reduction and fixation, bipolar hemiarthroplasty and total hip arthroplasty. Health Technol Assess (Rockv). 2005; 9(41).
- Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur - 13-year results of a prospective randomised study. Injury, 2000; 31(10): 793-797.
- Maceroli MA, Nikkel LE, Mahmood B, Elfar JC. Operative Mortality AfterArthroplasty for Femoral Neck Fracture and Hospital Volume. GeriatrOrthopSurgRehabil, 2015; 6(4): 239-245.
- Giliberty RP. Hemiarthroplasty of the hip using a low-friction bipolar endoprosthesis. Clin Orthop Relat Res, 1983; (175): 86-92.
- Bhattacharyya T, Koval KJ. Unipolar Versus Bipolar Hemiarthroplasty for Femoral Neck Fractures: Is There a Difference? J Orthop Trauma, 2009; 23(6): 426-427.
- Gilbert MS, Capozzi J. Unipolar or Bipolar Prosthesis for the Displaced Intracapsular Hip Fracture? ClinOrthopRelat Res, 1998; 353: 81-85.
- Choy WS, Ahn JH, Ko J-H, Kam BS, Lee D-H. Cementless Bipolar Hemiarthroplasty for Unstable Intertrochanteric Fractures in Elderly Patients.ClinOrthop Surg, 2010; 2(4): 221.
- Parker MJ, Gurusamy KS, Azegami S. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database of Systematic Reviews, 2010.
- Khan R, MacDowell A, Crossman P, Datta A, Jallali N, Arch B, et al. Cemented or uncementedhemiarthroplasty for displaced intracapsular femoral neck fractures. IntOrthop, 2002; 26(4): 229-232.
- Harris WH. Traumatic Arthritis of the Hip after Dislocation and Acetabular Fractures: Treatment by Mold Arthroplasty: An end-result study using a new method of result evaluation. JBJS. 1969; 51(4).
- Ramasamy V, Nallan R. Functional Outcome of Bipolar Hemiarthroplasty for Proximal Femoral Neck Fractures in Elderly: A Prospective Study. Journal of Orthopedics and Joint Surgery, 2022; 4(1): 22-25.
- K RK M. Prospective study of hemiarthroplasty for intracapsular fracture neck of femur using modular bipolar prosthesis. International Journal of Orthopaedics Sciences, 2018; 4(4): 92-95.
- Sharma A, Sahu S, Jain BK, Sagar S, Singh J. A prospective study to evaluate the functional outcome in fracture neck femur treated by cemented bipolar hemiarthroplasty in elderly patients. International Journal of Health and Clinical Research, 2022; 5(2): 147-156.
- Adapureddi HT, SBK, Kumar A, Paturi SK, Anne S, Reddy JP. Prospective study of management of fracture neck of femur by hemiarthroplasty with cemented bipolar. J Evol Med Dent Sci, 2015; 4(98): 16309-16314.

