A Duodenal Ulcer Mimicking a Dieulafoy Lesion
Mariam Lagrine1,2,*, Rabiy Elqadiry1,2, Houda Nassih1,2, Aicha Bourrahouat1,2 and Imane Ait Sab1,2
1Department of Pediatrics, Children’s University Hospital, Marrakech, Morocco
2Child Health and Development Research Unit, Cadi Ayyad University, Marrakech, Morocco
Received Date: 22/08/2024; Published Date: 28/10/2024
*Corresponding author: Mariam Lagrine, Department of Pediatrics, Children’s University Hospital, Marrakech, Morocco; Child Health and Development Research Unit, Cadi Ayyad University, Marrakech, Morocco
Abstract
A severe case of upper gastro-intestinal bleeding very likely due to a duodenal ulcer. This is a rare localization of a condition that is itself rare in children. It is often diagnosed in children when complications arise, the most frequent of which are digestive haemorrhage and perforation. The particularity of this case is the severity of the digestive haemorrhage and the endoscopic characteristics of the lesion, which led to the suspicion of a Dieulafoy lesion, linked to the existence of an abnormally large arteriole in the submucosal layer of the digestive wall. The patient was successfully treated with Proton Pump Inhibitors (PPIs) initially by injection (IVL) and then orally.
Keywords: Bulbar Ulcer; Dieulafoy lesion; Digestive haemorrhage; Proton pump inhibitors
Introduction
Dieulafoy's Lesion (DL) is a rare but important cause of Gastrointestinal (GI) haemorrhage in which bleeding occurs from a non-ulcerated punctate arterial lesion. While the vast majority of DLs are located in the stomach within 6 cm of the gastro-oesophageal junction, other locations in other parts of the gastrointestinal tract are possible [1]. We report a case of massive upper gastrointestinal bleeding from a duodenal lesion.A number of differential diagnoses can be confused with this lesion, namely gastro-duodenal ulcers, but the endoscopic appearance is a strong guide, and management is either endoscopic or surgical [2].
Case Report
A 6-year-old girl, previously in good health and not taking aspirin, presented with haemorrhagic shock caused by hematemesis and melena for 2 days, with no other associated signs, in particular no vomiting or abdominal pain. She was admitted to emergency with active external bleeding with blackish pebbly hematemesis and intense muco-cutaneous pallor. On examination; the child was conscious, HR= 128 bpm, RR = 44 bpm, CRT > 3s.The haemoglobin level was at 5.4 g/dl with otherwise normal blood chemistry.Na+= 134 mmol/l, K+ = 3.68 mmol/l, ALT = 18 U/L, AST= 34 U/l, Albumine= 35.44 g/l. She was urgently transfused with 500 cc of packed red blood cells.During an emergency oesophago-gastro-duodenoscopy (EGD), the vision was blurred, allowing oesophageal varices to be ruled out but limited by the abundance of bleeding and the need for re-transfusions. Family history of gastro-duodenal ulcers was negative. The child underwent emergency transfusion.
Within 24 hours, the need for a 2nd transfusion was indicated due to the persistence of hematemesis with increased muco-cutaneous pallor.
It was indicated in view of the rapidly worsening anaemia as a result of the resumption of massive hematemesis related to the presence of active bleeding in his upper gastro-intestinal tract. We performed a 2nd emergency upper gastrointestinal fibroscopy under general anaesthetic using a small-diameter upper endoscope. During the fibroscopy, blackish blood and clots were observed in his stomach. Exploration ruled out the presence of a gastric ulcer lesion and revealed a healthy gastric mucosa.
On reaching the duodenum, the bright red blood was determined to be of duodenal origin (figure 1) and careful observation revealed the presence of a minimal superficial lesion measuring 3 mm in diameter and taking on the appearance of a D (figure 2), no abnormality of the mucosa surrounding the lesion was noted and biopsies were taken; the lesion was therefore diagnosed as most likely a Dieulafoy lesion. Further exploration of the lesion was limited due to the absence of arteriography in our institution.
We started the child on PPI 40mg/day IVL for 48 hours. When the bleeding stopped, we switched to the oral route.Within a week, the girl had made a full recovery and was in excellent health. No recurrence of haemorrhage occurred during the follow-up period.
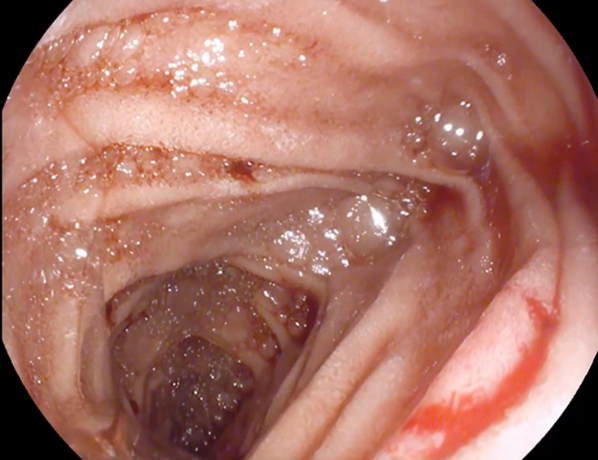
Figure 1: Fresh blood observed at the duodenal segment 1.
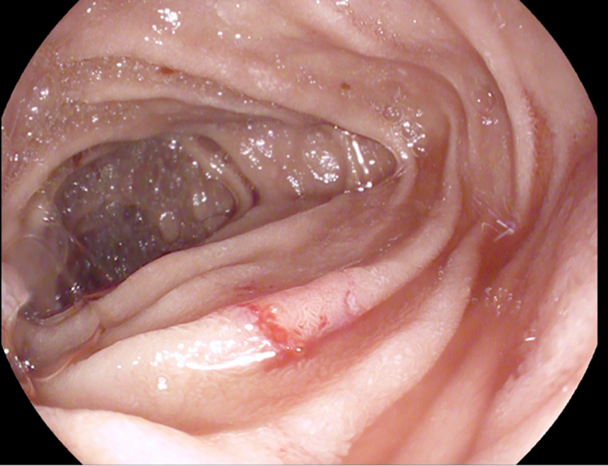
Figure 2: Appearance of the lesion in a D-shaped lesion with normal surrounding mucosa.
Discussion
A Dieulafoy lesion of the gastrointestinal tract was first described by the French surgeon Dieulafoy as an exulceration simplex in 1898; it is a rare but serious cause of gastrointestinal haemorrhage [1]. It is defined as a vascular anomaly consisting of a persistent and tortuous submucosal artery of large-calibre. The artery does not narrow when it reaches the mucosa and is therefore 1 to 5 mm in diameter, i.e., 10 times thicker than the normal size of an artery at this level [3]. On microscopic examination, the artery protrudes through a small mucosal defect which is usually 2 to 5 mm long and shows no other abnormalities of the arterial wall. The ulceration is limited to the overlying mucosa, while the surrounding mucosa appears histologically normal. Up to 6% of non-variceal bleeds in the upper gastrointestinal tract are caused by DL. Dieulafoy's lesion is a rare entity in the paediatric population [4]. Although it can occur in any part of the digestive tract, its most common location is the proximal third of the stomach and the lesser curvatures; although lesions in the duodenum, small intestine and colon have been reported. The cause of these lesions is unknown; however, congenital and acquired causes may contribute to their development [5]. Dieulafoy lesions can often go unnoticed during endoscopic assessment due to their small size, intermittent nature of bleeding and absence of surrounding stigmata such as ulceration [6]. When encountered, Dieulafoy lesions may be spurting or accompanied by active oozing blood. Dieulafoy lesions may be asymptomatic, unless the mucosa covering the vessel erodes, leading to bleeding [5]. Signs and symptoms are associated with blood loss, either due to intermittent or massive gastrointestinal haemorrhage. Melena is the most common presentation, followed by hematemesis, haematochezia, iron deficiency anaemia, haemoptysis and haemodynamic instability [8].In our case, the abundance of bleeding, the severity of the digestive haemorrhage and the endoscopic appearance of the lesion led us to think of a Dieulafoy lesion.The absence of arteriography in our institution limited further exploration of the lesion. The improvement of the digestive haemorrhage under PPI and the non-recurrence of bleeding were more in favour of a duodenal ulcer than a Dieulafoy lesion over the follow up period.
References
- Michael A Chang, et al. Endoscopic Management of Nonvariceal, Nonulcer Upper Gastrointestinal Bleeding. Gastrointestinal Endoscopy Clin N Am, 2018.
- Gabriele Marangoni, Adrian B Cresswell, Walid Faraj, Hizbullah Shaikh, Matthew J Bowles. An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. Journal of Pediatric Surgery, 2009; 44: 441–443.
- Christian Lilje, Greiner P, Riede UN, Sontheimer J, Brandis M. Dieulafoy Lesion in a One-Year-Old Child. Journal of Pediatric Surgery, 2004; 39(1): pp 133-134.
- Takaki Emura, Kenji Hosoda, Shota Harai, Noboru Oyachi, Takeyuki Suzuki, Ken Takada, et al. Dieulafoy lesion in a two-year-old boy: a case report. Journal of Medical Case Reports, 2016; 10: 293 DOI: 10.1186/s13256-016-1083-4.
- Joa ̃o Moreira-Pinto, Æ Carlos Raposo, et al. Jejunal Dieulafoy’s lesion: case report and literature review. Pediatr Surg Int, 2009; 25: 641–642. DOI: 10.1007/s00383-009-2383-1.
- Malika Kaci, Malika Baghdadi, Azzedine Selmani, et al. Dieulafoy gastric ulcer: A rare cause of massive upper gastrointestinal bleeding: about a histologically confirmed observation. JFMO: N°6, 2019.
- Mohammed Ibrarullah, Gajanan D Wagholikar. Dieulafoy's lesion of duodenum: a case report. BMC Gastroenterology, 2003.
- Giulia Maria Tronconi, Lucia Cococcioni, Maria Chiara Petrone, et al. Dieulafoy Gastric Lesion: An Unusual Cause of Pediatric Hematemesis. Open Journal of Pediatrics, 2016; 6: 120-123.

