Severe Cervical Spine Injury with Concurrent Cardiac Complications
El Mawla Zeinab1,*, Sarkis Jeannette2, Jabbour Ingrid2, Khalil Majd3, Olaywan Layal4, Bleibel Jerar4 and El Khalil Joseph5
1Department of Pulmonary & Critical Care, Faculty of Medical Sciences, Lebanese University, Hadat, Lebanon
2Department of Internal Medicine, Faculty of Medical Sciences, Lebanese University, Hadat, Lebanon
3Cardiology Division, Lebanese Hospital Geitaoui - University Medical Center (HLG-UMC), Beirut, Lebanon
4Pulmonary and Critical Care Division, Lebanese Hospital Geitaoui - University Medical Center (HLG-UMC), Beirut, Lebanon
5Orthopedic Department, Chief Medical office, Lebanese Hospital Geitaoui - University Medical Center (HLG-UMC), Beirut, Lebanon
Received Date: 28/08/2024; Published Date: 28/10/2024
*Corresponding author: El Mawla Zeinab, Department of Pulmonary & Critical Care, Faculty of Medical Sciences, Lebanese University, Hadat, Lebanon
Abstract
Introduction: Cervical spinal cord injury (SCI) causes severe motor and sensory impairments, including tetraplegia, and significantly impacts quality of life. Due to factors like immobility and autonomic dysregulation, SCI patients are at higher risk for ST-elevation myocardial infarction (STEMI). Managing both conditions simultaneously is complex and requires a coordinated, multidisciplinary approach to ensure optimal recovery and outcomes.
Case Presentation: A 65-year-old male with a heavy smoking history presented with tetraplegia and respiratory distress after a fall and was transferred to our facility 4 days later. He required intensive care for severe bradycardia and hypotension. Imaging revealed significant cervical spine injuries, leading to an anterior cervical discectomy and fusion (ACDF) at C3-C4-C5. Postoperatively, he experienced persistent bradycardia and developed an ST-elevation myocardial infarction (STEMI), necessitating cardiac catheterization and stenting. Further interventions included a permanent pacemaker, tracheostomy, and PEG tube. The patient was discharged home in stable condition with ongoing physiotherapy and follow-up.
Discussion: Spinal cord injury (SCI) and ST-elevation myocardial infarction (STEMI) are severe conditions that complicate patient health. SCI leads to paralysis and sensory loss, increasing the risk of STEMI due to factors like autonomic dysregulation and physical inactivity. Diagnosis of STEMI in SCI patients involves ECG, biomarkers, and imaging. Management includes acute reperfusion therapy, medication, and a multidisciplinary approach. Prognosis varies based on injury severity and treatment, requiring ongoing care for both cardiovascular and neurological health.
Conclusion: The case of a 65-year-old male with both severe cervical spinal cord injury and ST-elevation myocardial infarction highlights the rarity and complexity of managing these concurrent conditions. This unusual combination underscores the need for a comprehensive, multidisciplinary approach to optimize diagnosis, treatment, and patient outcomes.
Keywords: Spinal cord injury; STEMI; Respiratory distress; Bradycardia; Case report
Introduction
Cervical Spinal Cord Injury (SCI) is a severe medical condition resulting from trauma to the cervical spine, often leading to significant motor and sensory impairments below the level of injury. This type of injury can cause tetraplegia, affecting both upper and lower limbs, and severely impairing the patient’s quality of life and functional abilities [1]. The cervical spine, comprising the first seven vertebrae, is particularly susceptible to injury due to its mobility and the critical neural structures it protects. The impact of cervical SCI can be profound, necessitating comprehensive medical and rehabilitative interventions [2].
Patients with cervical SCI are at heightened risk for various complications, including cardiovascular events such as ST-elevation myocardial infarction (STEMI). STEMI is a serious type of myocardial infarction characterized by significant and prolonged ischemia of the heart muscle due to the complete blockage of a coronary artery [3]. The physiological stress associated with SCI, alongside factors such as immobility, autonomic dysregulation, and potentially pre-existing cardiovascular conditions, can increase the likelihood of STEMI [4].
The concurrent management of cervical SCI and STEMI presents a complex challenge, necessitating an integrated, multidisciplinary approach to optimize patient outcomes. Effective treatment strategies must address both the spinal injury and the cardiac event to mitigate long-term complications and improve overall recovery [5,6].
Case Presentation
A 65-year-old male with a heavy smoking history (80 pack-years) and no significant past medical history presented with tetraplegia and respiratory distress following a fall. He was transferred to our facility from a peripheral hospital 4 days after the accident. On admission to the ICU, the patient required sedation, intubation, and mechanical ventilation. He exhibited severe bradycardia with a heart rate of 30 bpm and hypotension, with a blood pressure below 70 mmHg. Initial management involved the administration of adrenaline to stabilize his hemodynamics.
Diagnostic imaging on April 15, 2024, provided critical insights into the patient's condition. An MRI of the brain revealed no acute infarcts, hemorrhages, contusions, or axonal injuries. However, MRI of the cervical spine identified significant findings, including thickening of the anterior longitudinal ligament, intense edema of the prevertebral soft tissues, and a Grade 1 retrolisthesis at C3. Additionally, there was a posterior disco-osteophytic complex at C3-C4 with central protrusion, posterior subluxation of the facet joints, and significant spinal cord compression with an anterior-posterior (AP) diameter of 4.2 mm. The imaging also showed focal myelopathy extending 2 cm craniocaudally and moderate neural foraminal narrowing, though no hemorrhage was noted. (Figure 1)
Due to the ineffectiveness of steroid therapy, it was discontinued, and surgery was postponed by 2 days because of the patient's instability.
On April 18, 2024, the patient underwent an anterior cervical discectomy and fusion (ACDF) at C3-C4-C5. The surgical procedure included the placement of an anterior plate and screws, intervertebral body cages, and posterior pedicular screws and rods. Postoperative radiographs confirmed minimal retrolisthesis at C3 and revealed multilevel degenerative disc disease with osteophyte formation.
Following surgery, the patient's hemodynamic status improved, and he became responsive to verbal stimuli with partial sensory recovery. Despite these gains, bradycardia persisted, especially during minimal positional changes and spontaneous breathing trials. On April 25, 2024, a temporary pacemaker was implanted due to ongoing bradycardia. The following day, the patient developed chest discomfort, ST elevation on ECG, (Figure 2) and elevated cardiac troponin levels, indicating an ST-elevation myocardial infarction (STEMI) with a troponin level of 75.5 ng/L (reference range: 0-14 ng/L). Cardiac catheterization revealed a 70% stenosis in the mid-right coronary artery (RCA), necessitating percutaneous transluminal coronary angioplasty (PTCA) and stenting of the mid-RCA. An echocardiogram performed on April 27, 2024, showed hypokinesia of the myocardial wall and minimal pericardial effusion.
Further management included the implantation of a permanent dual-chamber pacemaker on May 9, 2024, to address the persistent bradycardia. A tracheostomy was performed on May 10, 2024, to facilitate long-term ventilation, and a percutaneous endoscopic gastrostomy (PEG) tube was inserted on May 30, 2024, to provide nutritional support.
The patient was discharged home on June 5, 2024, in a conscious and cooperative state. He continued to engage in physiotherapy and was scheduled for outpatient follow-up. This case highlights the intricate management required for severe cervical spine injuries complicated by significant cardiac events and underscores the importance of a multidisciplinary approach in addressing both spinal and cardiac conditions effectively.

Figure 1: MRI of the cervical spine identified a posterior disco-osteophytic complex at C3-C4 with central protrusion, posterior subluxation of the facet joints, and significant spinal cord compression.
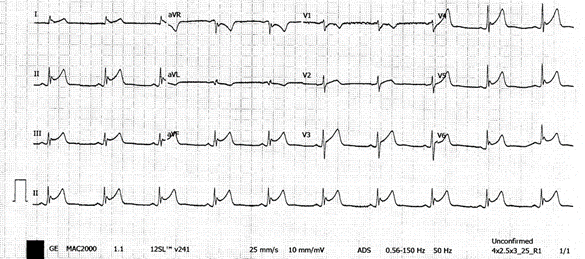
Figure 2: Electrocardiogram showing ST elevation on leads II, III, AVF.
Discussion
Spinal Cord Injury (SCI) and ST-elevation myocardial infarction (STEMI) are both serious medical conditions that can profoundly affect patient outcomes. SCI, resulting from trauma to the spinal cord, can lead to significant neurological deficits, including paralysis and loss of sensory functions below the level of injury. STEMI, characterized by prolonged and complete occlusion of a coronary artery, leads to substantial myocardial damage and requires urgent medical intervention. The intersection of SCI and STEMI presents a complex clinical scenario, as patients with SCI are at increased risk for cardiovascular events due to various physiological and clinical factors [3,4].
The prevalence of SCI in the general population is approximately 54 cases per million annually in the United States, with traumatic causes being the leading contributors [7]. Cardiovascular complications, including STEMI, are increasingly recognized as significant concerns in the SCI population. Studies indicate that individuals with SCI have a higher incidence of cardiovascular disease compared to the general population, partly due to the associated autonomic dysfunction, physical inactivity, and metabolic changes [8]. The incidence of STEMI in individuals with SCI is not well-documented but is believed to be higher due to these underlying risk factors.
The pathophysiology linking SCI and STEMI involves several interconnected mechanisms. SCI can lead to autonomic dysregulation, which affects cardiovascular control. This dysregulation can result in abnormal heart rate variability and increased susceptibility to arrhythmias [8]. Additionally, the immobility associated with SCI contributes to a sedentary lifestyle, which is a known risk factor for coronary artery disease [4]. Reduced physical activity and subsequent metabolic syndrome, including obesity, hypertension, and dyslipidemia, further exacerbate cardiovascular risk [4].
Several risk factors contribute to the increased incidence of ST-Elevation Myocardial Infarction (STEMI) in individuals with Spinal Cord Injury (SCI). Autonomic dysregulation is a significant factor, as SCI often impairs the balance between sympathetic and parasympathetic nervous systems, leading to abnormal cardiovascular responses [8]. Physical inactivity also plays a crucial role; reduced mobility in SCI patients results in lower levels of physical fitness, which can contribute to the development of metabolic syndrome, a condition characterized by obesity, hypertension, and dyslipidemia [4]. These metabolic abnormalities further elevate the risk of cardiovascular events. Additionally, SCI can cause immune dysfunction, potentially increasing susceptibility to atherosclerosis, which exacerbates the risk of STEMI [9].
Diagnosis of STEMI in the SCI population typically follows established clinical protocols. Electrocardiogram (ECG) is utilized to identify ST-segment elevation, a hallmark of STEMI [3]. Cardiac biomarkers, particularly elevated troponin levels, are critical for confirming myocardial injury [10]. Imaging techniques, including echocardiography and coronary angiography, are employed to evaluate the extent of myocardial damage and to detect any coronary artery lesions [10].
Management of STEMI in patients with SCI involves several key components. Acute reperfusion therapy is essential and may include thrombolysis or Percutaneous Coronary Intervention (PCI) to restore coronary blood flow [5]. Pharmacological management includes the use of antiplatelet agents and anticoagulants to address myocardial ischemia and prevent further clot formation [3]. A multidisciplinary approach is critical in managing these complex cases, requiring close coordination among cardiologists, neurologists, and rehabilitation specialists to address both cardiac and spinal injuries effectively [6].
The prognosis for SCI patients with STEMI depends on several factors, including the severity of the spinal injury, the extent of myocardial damage, and the effectiveness of the treatment regimen. Early intervention and comprehensive management can improve outcomes, but the presence of SCI can complicate recovery and rehabilitation. Long-term prognosis may involve ongoing cardiovascular monitoring and rehabilitation to address both neurological and cardiovascular health [4,7].
Conclusion
The case of the 65-year-old male with both severe cervical spinal cord injury (SCI) and ST-elevation myocardial infarction (STEMI) highlights the rarity and complexity of managing concurrent spinal and cardiac conditions. While each condition independently presents significant challenges, the intersection of SCI and STEMI is particularly uncommon, making this case especially noteworthy. The unusual combination of these conditions underscores the need for heightened clinical awareness and a tailored, multidisciplinary approach to diagnosis and treatment. This rare occurrence emphasizes the importance of addressing both spinal and cardiovascular health in a comprehensive manner to optimize patient outcomes and guide future research and clinical practices.
Consent for publication: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review upon request by the Editor-in-Chief of this journal.
Ethics Approval and Consent to Participate: Ethical approval was not applicable.
Conflict of interest: The authors declare that they have no conflict of interest.
Financial Disclosure: The authors declared that this study has received no financial support.
Acknowledgments: Not applicable.
Provenance and Peer Review: Not commissioned, externally peer reviewed.
References
- Fehlings MG, Tetreault LA, Wilson JR, Kwon BK, Burns AS, Martin AR, et al. A Clinical Practice Guideline for the Management of Acute Spinal Cord Injury : Introduction , Rationale , and Scope, 2017; 7: 84–94.
- Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D, et al. Review Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel : spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials, 2007; (December 2006): 190–205.
- Thygesen K, Jaffe AS, Chaitman BR, White HD, Zealand N, Canada PJD. Fourth Universal De fi nition of Myocardial Infarction ( 2018 ). J Am Coll Cardiol [Internet], 2018; 72(18): 2231–2264. https://doi.org/10.1016/j.jacc.2018.08.1038
- Furlan JC, Sakakibara BM, Miller WC, Krassioukov AV. Global Incidence and Prevalence of Traumatic Spinal Cord Injury, 2012.
- Support L, Support L, Life N, Magid DJ, Aziz K, Berg KM, et al. Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction.
- Kirshblum SC, Burns SP, Biering-sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury ( Revised 2011 ), 2011; 34(6): 535–546.
- Devivo MJ. Epidemiology of traumatic spinal cord injury : trends and future implications. Spinal Cord, 2012; (December 2011): 365–372.
- Krassioukov AV, Furlan JC, Fehlings MG. Autonomic Dysreflexia in Acute Spinal Cord Injury : An Under-Recognized Clinical Entity, 2003; 20(8): 707–716.
- Cragg JJ, Noonan VK, Krassioukov A. Cardiovascular disease and spinal cord injury Results from a national population health survey, 2013.
- Allan S Jaffe, Luciano Babuin, Fred S Apple P. Biomarkers in Acute Cardiac Disease The Present and the Future, 2006; 48(1): 1–11.

