Frontal Fibrosing Alopecia and Comorbidities in a Moroccan Population
Fajri Zineb*, Hanane Baybay, Meryem Soughi, Zakia Douhi, Sara Elloudi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II of Fez, Morocco
Received Date: 04/09/2024; Published Date: 25/10/2024
*Corresponding author: Fajri Zineb, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Keywords: Comorbidities; Frontal fibrosing alopecia; Moroccan
To the Editor: Frontal Fibrosing Alopecia (FFA) is a lymphocytic scarring alopecia that most commonly affects the fronto-temporal line and eyebrows. It is increasingly common and may be associated with multiple comorbidities and other inflammatory and autoimmune diseases.
The objectives of our study were to analyze the frequency of comorbidities associated with FFA in a Moroccan population.
We performed a descriptive retro-prospective observational study that included all patients diagnosed with FFA, at our dermatology department at University Hospital Center HASSAN II Fez in Morocco over three years from 2020 to 2023.
A total of 96 female patients with a confirmed diagnosis of FFA were included. The median age was 47. 61% were premenopausal. 42% were of phototype IV, 35 % of phototype III, and 15 % of phototype V. 49 % had a linear FFA type, 37,5 % had a diffuse type, and 9.3% had a pseudo-fringe sign type. 65.7% had an eyebrow alopecia.
In the population studied, 79 patients (82% of cases) had a comorbidity. 48% had the Cutaneous co-morbidities:
Lichen planus pigmentosus (26 %) and rosacea (16 %) were the most frequently reported comorbidities, followed by lichen pilaris (10,4%) and lichen planus (6,25 %) (Figure A).
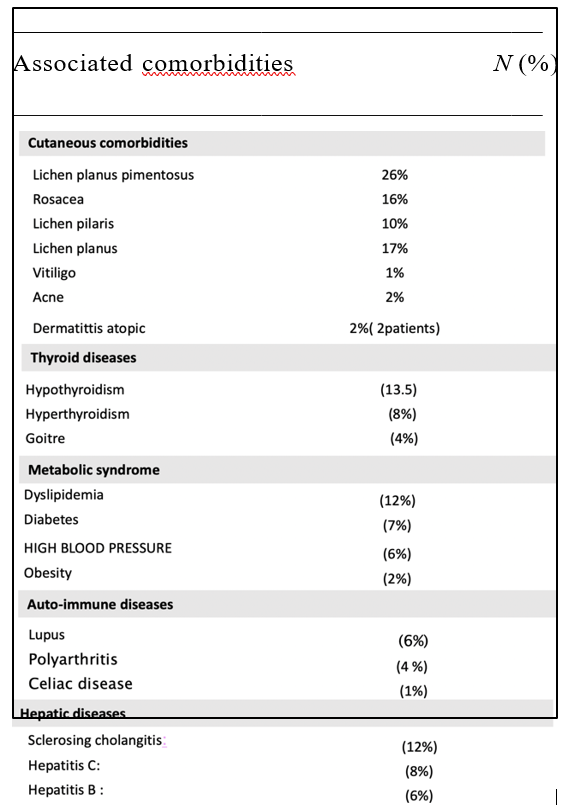
Other co-morbidities were found in particular: Thyroid disease (n=25 patients) => 26%, Metabolic syndrome (n=23 patients) => 24%, Autoimmune disease (n=11 patients) => 12%, Other (n=4 patients) => 4%. Table 1 summarizes all the associated comorbidities.
Lichen planus pigmentosus and FFA are variants of lichen and have been frequently associated especially in dark phototypes.
Rosacea was diagnosed in 28.9% of our patients, which supports findings by Pindado-Ortega et al1 that patients with FFA have a higher risk of rosacea. It seems that the immune system plays an important role by the involvement of common inflammatory pathways to these 2 pathologies of the pilosebaceous follicle [1]. Also, the prevalence of rosacea increases with age and some risk factors could help the development of rosacea during FFA-like peri- follicular erythema, a high body mass index and a low progesterone level [2].
The association of thyroid disorders and FFA might be related to thyroid hormones. In short term they have a stimulating effect on the cytokeratin 15, a marker of stem cells found in the hair follicle bulge, but after a long stimulation, thyroid hormones will have a role in the apoptosis of stem cells [3].
Dyslipidemia is also a frequently reported associated comorbidity with FFA. The peroxisome proliferator-activated receptor has been incriminated. This nuclear receptor plays the role of a transcription factor helping in the regulation of expression of genes involved in lipid homeostasis, hence it has a role in the maintenance of the pilosebaceous follicule. Studies have suggested that the initial triggering of inflammation in lichen planus is due to a dysfunction of this receptor, leading to a disruption of lipid metabolism in the sebaceous gland and a subsequent inflammatory response [4].
As for diabetes, a lower risk of diabetes in FFA patients [5] has been reported which is consistent with our results, given the low percentage of diabetes; 7% in our patients, compared to 12.4%; prevalence of diabetes in the adult population in Morocco.
Given that the prevalence of arterial hypertension in Morocco is 33.6% in the adult population, it also seems that the FFA is associated with a lower risk of arterial hypertension.
Previous observational studies have reported́ a significant elevated prevalence of autoimmune diseases in patients with FFA.
The greatest tendance autoimmune disease in women has been related to hormones.
In situations where there is an oestrogenic predominance, there is an immune shift towards the helper 2 T-cell response, increasing the autoimmune risk.
In fact, certain autoimmune diseases such as lupus and primary gallstone cirrhosis, coexisting with FFA, can present a clinical worsening with oestrogens. In our study, around 12% of patients, mainly women, had an associated immune disorder, notably lupus in 6 patients, followed by rheumatoid arthritis.
In conclusion: we observed multiple comorbidities in our population of FFA patients seen in a university hospital in Morocco, as autoimmune pathologies and inflammatory diseases, the mechanisms of which may be common, as well as their management. Knowledge of these pathologies, which may be associated with AFF, has a major impact on treatment and prognosis, which justifies the search for these comorbidities to ensure comprehensive management.
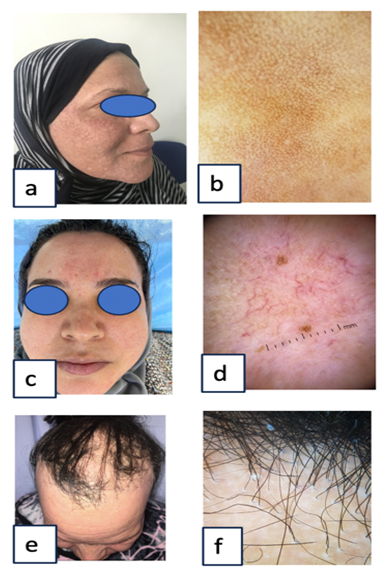
Figure A: lichen pigmentosus: (a) Clinique, (b) Dermoscopy: blue-grey dots rosacea (c) Clinique, (d) Dermoscopy: polygonal vessels Figure c : lichen pilaris (e) Clinique, (f) Dermoscopy peri-pilary scales.

Figure B: A patient with AFF and hyperthyroidism.
Table 1: Associated comorbidities.
References
- Pindado-Ortega C, Saceda-Corralo D, Buend´ıa-Castan~o D, et Frontal fibrosing alopecia and cutaneous comorbidities: a potential relationship with rosacea. J Am Acad Dermatol, 2018; 78(3): 596-597.e1.
- Porrin~o-Bustamante ML, Fern´andez-Pugnaire MA, Arias-Santiago S. Frontal fibrosing alopecia: a review. J Clin Med, 2021; 10(9): 1805.
- Tiede S, Bohm K, Meier N, et Endocrine controls of primary adult human stem cell biology: thyroid hormones stimulate keratin 15 expression, apoptosis, and differentiation in human hair follicle epithelial stem cells in situ and in vitro. Eur J Cell Biol, 2010; 89(10): 769-777.
- Karnik P, Tekeste Z, McCormick TS, et al. Hair follicle stem cell-specific. PPARgamma deletion causes scarring alopecia. J Investig Dermatol, 2009; 129: 1243-1257.
- Fertig RM, Hu S, Maddy A, et al. Medical comorbidities in patients with lichen planopilaris, a retrospective caseecontrol study. Int J Dermatol, 2018; 57(7): 804-809.

