Efficacy of Cervical Epidural Versus Thoracic Epidural Anesthesia for Breast Surgery: A Prospective Randomized Double-Blinded Study
Pratibha Jain Shah1, Ummu Habeeba2 and Falgudhara Panda3,*
1Professor and HOD, Department of Anesthesiology and Pain Medicine, Pt. J.N.M. Medical College and Dr. B.R.A.M. Hospital, India
2Registrar, Department of Anesthesiology and Critical Care, Aster Hospital, UAE
3Postgraduate Medical Officer, Department of Anesthesiology, District Hospital, India
Received Date: 29/07/2024; Published Date: 24/10/2024
*Corresponding author: Falgudhara Panda, MD, Postgraduate Medical Officer, Department Of Anesthesiology, District Hospital, Janjgir, Chhattisgarh, India
Orcid ID: 0009-0005-7169-4278
Abstract
Background & Aim: Both cervical and thoracic epidural anesthesia techniques are being used for breast surgeries across the globe but in lesser frequency. This prospective randomized double-blinded study compares the effectiveness of both regional techniques in terms of changes in hemodynamic parameters as primary objective and blockade characteristics (onset and duration of sensory and motor blockade, mean block level, quality of surgical anesthesia) and side effects/ complications as secondary objectives.
Methods: After approval from the Institute Ethics committee and written informed consent from patients, 80 female patients undergoing elective breast procedures were randomly allocated into two groups: Group CE (cervical epidural anesthesia receiving group) and group TE (thoracic epidural anesthesia receiving group).
Results: Group CE had a significant decrease in SBP and DBP at 15 minutes and thereafter till the offset of blockade; whereas group TE had significant fall in DBP at 10, 15, and 30 minutes without any significant fall in SBP. Heart rate (HR) decreased after 20 minutes of drug instillation in group CE which returned to baseline at 45 minutes; while HR fell after 10 minutes in group TE which returned to normal after 90 minutes. The onset of sensory and motor blockade, and mean blockade level were comparable among both groups. Duration of sensory and motor blockade was higher in group CE. The incidence of side effects and complications was also higher in group CE.
Conclusion: Though both thoracic epidural and cervical epidural are effective in providing anesthesia & analgesia for breast surgery, the thoracic epidural approach serves safer anesthesia in terms of its lesser hemodynamic variations, lower side effects, and complications, however, cervical epidural provides superior blockade characteristics.
Keywords: Breast surgery; Thoracic epidural anesthesia; Cervical epidural anesthesia
Introduction
Breast surgeries including lumpectomy, modified radical mastectomy, cosmetic reconstruction surgery, and breast augmentation are on the rise because of increased incidence of breast cancer. These surgeries were traditionally being conducted under general anaesthesia. [1,2] The advancements in imaging, opportunities for training, and back up with various studies offer a more audacious regional anesthesia like epidural anesthesia, thoracic spinal, paravertebral block, and interfascial plane block. Apart from avoidance of attempts in the difficult airway and reduction in intraoperative blood loss; existing literature reported various advantages of Thoracic Epidural Anaesthesia (TEA) and Cervical Epidural Anaesthesia (CEA) like superior-extended analgesia, hemodynamic stability, reduced postoperative nausea and vomiting (PONV), lower analgesic consumption, earlier resumption of feeding and mobilization, shorter duration of hospitalisation and rapid patient turnover [3-5].
CEA and TEA are used as the sole anaesthetic for various surgeries including breast surgeries to provide selective blockade of cardiac sympathetic fibres, which helps in decreasing the surgical stress, improves the myocardial oxygen balance, and stabilizes the hemodynamic parameters [4-6]. Attenuation of perioperative stress response improves immune function thereby inhibiting development of postoperative cancer recurrence and metastases [7]. But, thorough knowledge of anatomy, skills, and expertise are of utmost importance in conducting cervical and thoracic epidural since the adverse effects and complications attract legal and emotional consequences.
As per the available literature, there are hardly any study comparing CEA and TEA for breast surgeries. Therefore, the present study was aimed to compare effectiveness of cervical and thoracic epidural anesthesia for breast surgeries in regards to hemodynamic changes (changes in blood pressure, heart rate, respiratory rate and oxygen saturation) as primary outcome; block characteristics (onset, duration and quality of sensory and motor blockade, and extent of blockade) and adverse effects / complications as secondary outcomes.
Material and Methods
The present prospective double-blind randomized study was conducted in a tertiary care teaching hospital after getting approval from Institutional Ethics Committee and written informed consent from patients. Total 80 female patients between 18-60yrs of age, 40-75kg weight, 140-180cm height with American Society of Anaesthesiologists (ASA) physical status І - IIІ scheduled for elective breast surgeries were enrolled for study from March 2019 to August 2020. Patients who refused to participate, had systemic or local back infections, bradyarrhythmias, thoracic or cervical arthritis with neurological deficit, thoracic/cervical spine deformity, allergy to local anesthetic drugs, on blocker and bleeding disorders were excluded from the study.
For sample size calculation, a pilot study was conducted on 20 patients (n=10) who were equally distributed among CE group and TE group due to paucity of previous studies comparing these approaches for breast surgery. We observed that 60% of the CE group and 20% of the TE group had a ³ 20% drop in MAP from baseline. Taking this into consideration, with a confidence level of 99% and 80% of power, a minimum sample size of 39 per group was required to compare the effectiveness of these two anaesthetic approaches for breast surgeries as calculated by Epitool in stat software.
Randomisation was done by sealed envelope technique with an allocation ratio of 1:1 into 2 groups by a resident anaesthesiologist. For that, 80 slips labelled with either CE or TE were sealed with an adhesive and placed in a container. If participant was excluded after randomisation because of any reason mentioned above, then that slip was again dropped into the container. A total of 98 patients were screened and 12 patients were excluded based on exclusion criteria (Figure 1). Group CE received cervical epidural anaesthesia and Group TE received thoracic epidural anaesthesia for the breast surgeries.
All patients were nil per oral for six hours prior to operation. On arrival to operation theatre, multi-para monitors were attached & baseline heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), peripheral oxygen saturation (SpO2) & electrocardiogram (ECG) were recorded. A large wide-bore intravenous (iv) cannula was inserted into forearm opposite to the side of breast surgery and started with 10-15ml/kg/hr Ringer Lactate (RL). The patients were explained about Visual Analogue Scale (VAS 0-10) for measuring pain in the perioperative period in advance. All patients were premedicated with iv midazolam 1mg and iv metoclopramide 10mg.
For cervical epidural, patient was placed in sitting position with neck flexed and skin and underlying tissues at C6 – C7/ C7-T1 interspace were infiltrated with 2% lignocaine 1-2ml under all strict aseptic precautions. After 2-3minutes, 18-gauge Tuohy needle was advanced perpendicular to the skin through either the midline approach. Epidural space was identified by loss of resistance technique using hanging drop method. Epidural catheter was threaded through the needle and advanced for 3 to 5 cm caudad into epidural space then needle was withdrawn over the firmly gripped catheter that was then secured to the back and opposite shoulder with adhesive dressing.
For thoracic epidural, patient was placed in sitting position and T9-T10/ T8-T9 interspace was infiltrated with 1-2ml of 2% lignocaine under all aseptic precautions. After 2-3minutes, 18-gauge Tuohy needle was advanced at 30-450 cephalad either through midline or paramedian approach. Epidural space was identified by the loss of resistance technique using Luer lock syringe containing air. Epidural catheter was threaded through the needle and advanced for 4 to 5 cm cephalad into epidural space then needle was withdrawn over the firmly gripped catheter that was then secured to the back and opposite shoulder with adhesive dressing.
After epidural catheter insertion, patients were placed supine and test dose containing 3 ml of 2% lignocaine with adrenaline (1:200,000) was injected through the catheter to confirm catheter position. After 5-10 minutes of test dose confirmation, 10 ml of 0.5% bupivacaine was injected through the epidural catheter in both the groups. 100% oxygen was given by nasal cannula at a rate of 2-4 l/ minute to all the patients throughout the procedure. Surgeons were allowed to perform surgery after achieving adequate blockade of required dermatomes (T1-T6).
The sensory block was assessed every 2 minutes by pin prick bilaterally until complete blockade was obtained. The onset (i.e., the time from instillation of drug to complete loss of sensation of desired dermatomes), extent (i.e., number of dermatomes between highest and lowest level of skin analgesia) and duration of sensory blockade (i.e., onset of sensory blockade to first occurrence of pain during/after surgery) were noted. The motor block was assessed by checking the hand grip strength. The onset (i.e., the time from instillation of drug to onset of weakness of upper limb and hand grip strength) and duration of motor blockade (i.e., the onset of motor blockade to complete recovery of weakness of upper limb and hand grip strength) were noted. The quality of sensory blockade was assessed by visual analogue scale (Range 0-10, where 0 indicates no pain and 10 indicates maximum pain), while the quality of motor blockade was assessed using the following scale described by Michalek Pavel et al [8]: 1- absence of motor blockade, 2 - partial motor blockade, and 3- complete motor blockade. The block was considered as failed if the patient perceived pain after 30 minutes of procedure, and were converted to GA.
Continuous ECG and HR, SBP, DBP, MAP, RR and SpO2 were recorded at every 5 minutes interval for initial 20 minutes and there after every 10 minutes till the end of surgery. HR below 50/min was considered as bradycardia and treated with iv atropine. Significant hypotension was defined when there is a fall in the systolic BP more than 20% from the pre-operative value and was treated with iv fluids and iv mephenteramine. Fall in SpO2 below 90% and any respiratory distress was considered significant and treated accordingly.
Propofol infusion was started @ 25-75 mcg/kg/min for conscious sedation of grade II whenever required with constant monitoring of cardiopulmonary function. Level of sedation was assessed according to the modified Wilson sedation scale [9] (Grade I-awake, II-sleeping, easily arousable, III-deep sleep but arousable, IV-deep sedation but not arousable) hourly for four hours, then at six and 12 hours. Epidural top-up was given with 50% of the bolus dose (5 ml) if patient complained of pain or discomfort.
Postoperative analgesia was provided with 5ml of 0.125% bupivacaine on patient’s demand or when VAS >3. Epidural catheter was removed after 48 hours.
Any side effects or complications related to the techniques such as nausea, hypotension, bradycardia, shivering, respiratory compromise and Horner’s syndrome were managed and recorded throughout the study period.
Statistical analysis was performed using Microsoft Excel version 22. Results were expressed as mean± SD, number, and percentage. All tests were two tailed and performed at a significance level of 0.05.
Result
Demographic variables of patients and duration of surgery were comparable between the groups (Table 1).
Baseline SBP, DBP and HR was comparable in both the groups. SBP and DBP were significantly low at 15 min and thereafter till the offset of the blockade in group CE; whereas only DBP fall significantly at 10,15, 30 min in group TE (Figure 2). In group CE, a significant fall in HR was observed at 20 min after drug instillation, which returned to baseline at 45 min. Whereas, in group TE significant fall in HR was noted after 10 min that returned to normal after 90 min (Figure 3). The respiratory rate was increased at 10 min and thereafter remained same till offset of blockade in group CE which turned out to be statistically insignificant whereas, in group TE no such change was noticed. Mean RR was 15±1.1/min in group CE and 15 ± 1.3/min in group TE (p=0.36). None of the participants had episodes of desaturation throughout the study period. Mean SpO2 was 98±1% and 98 ± 1.5% in group CE and TE, respectively. (p= 0.35)
The mean onset of sensory & motor blockade was shorter in group CE compared to group TE; although it was statistically insignificant. However, the duration of both sensory & motor blockade was significantly prolonged in Group CE. The mean blockade level achieved was comparable with maximum of 11 segments and minimum of 8 segments in both groups. (Table 2). Mean VAS score for assessment of quality of analgesia was similar in both groups (Figure 4). There was higher failure rate in group CE (n= 4) compared to group TE (n=2) as depicted in Consort diagram.
Propofol supplementation for sedation was needed in 4 patients (10 %) in group CE and 6 patients (15 %) in group TE (p=0.25).
On assessing the side effects 10%, 42.5 %, 57.5%, 32.5%, and 6.6% of cases reported nausea, hypotension, bradycardia, shivering and Horner’s syndrome in group CE, whereas, 7.5%, 17.5%, 17.5 %, 22.5% and 0%, respectively in group TE. None of the patients had accidental intravascular injection, dural puncture and respiratory distress (Figure 5).
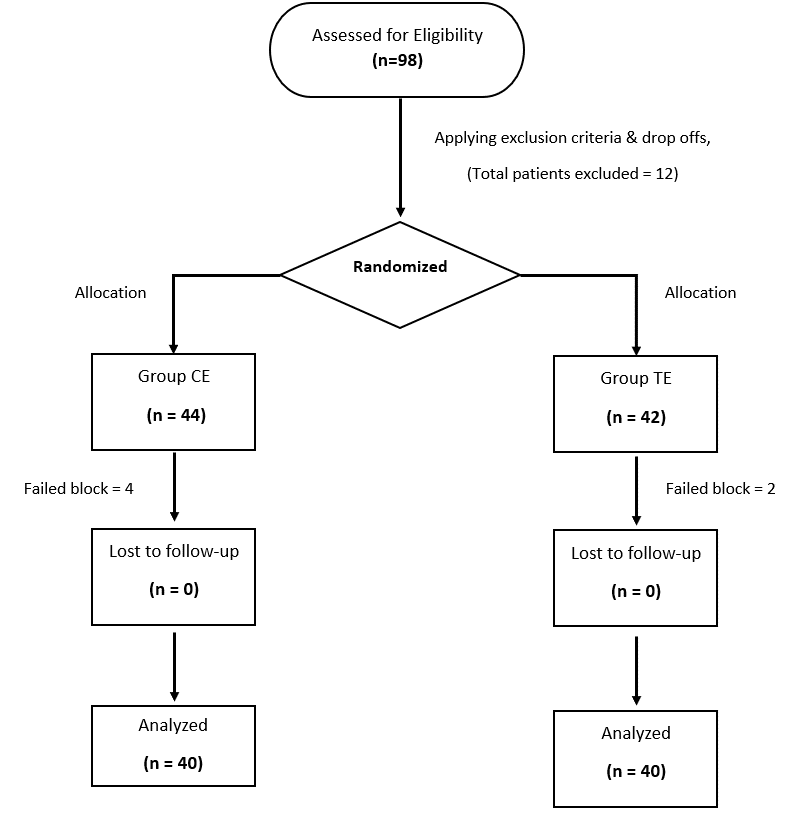
Figure 1: Consort Diagram
Table 1: Demographic profile and duration of surgery.

Table 2: Block Characteristics.

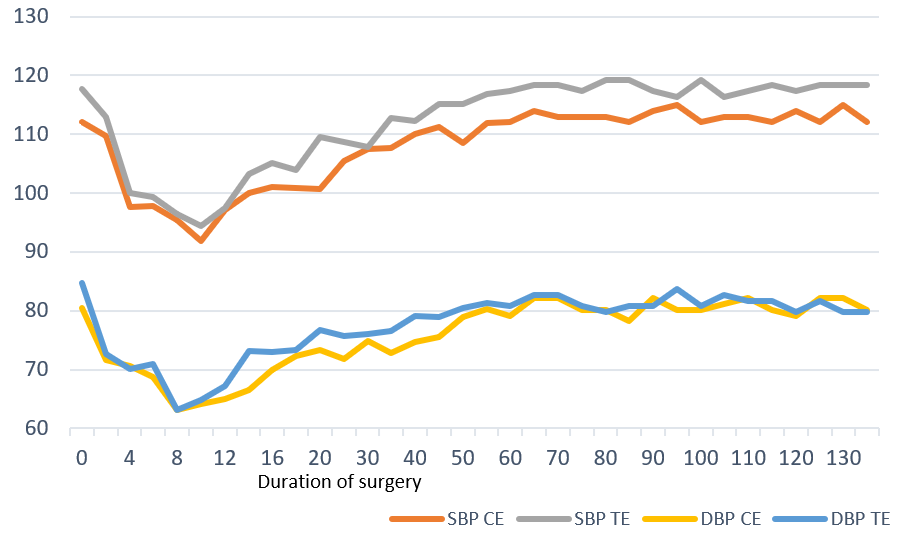
Figure 2: SBP & DBP at various time interval.
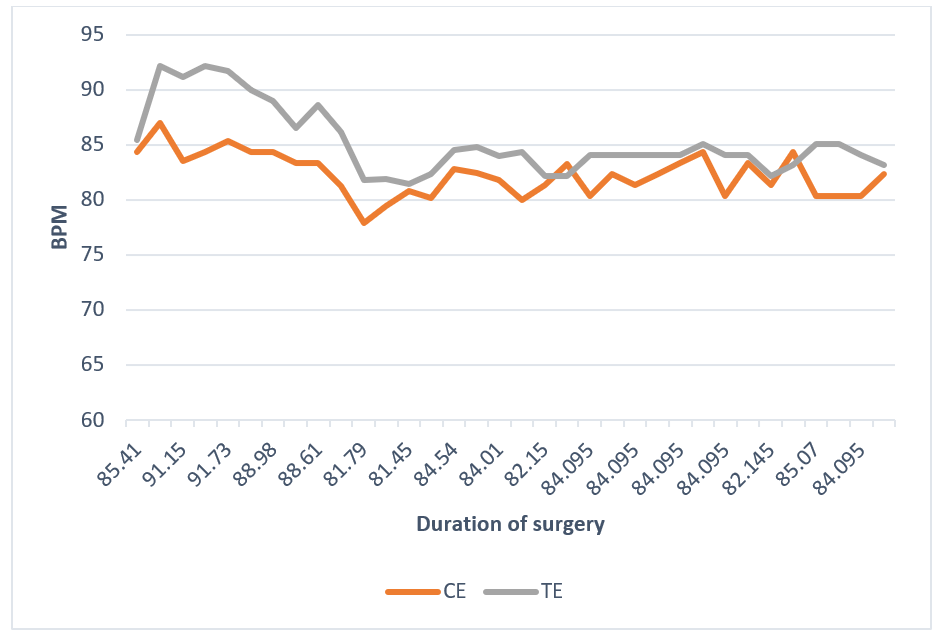
Figure 3: Heart Rate at various time intervals.
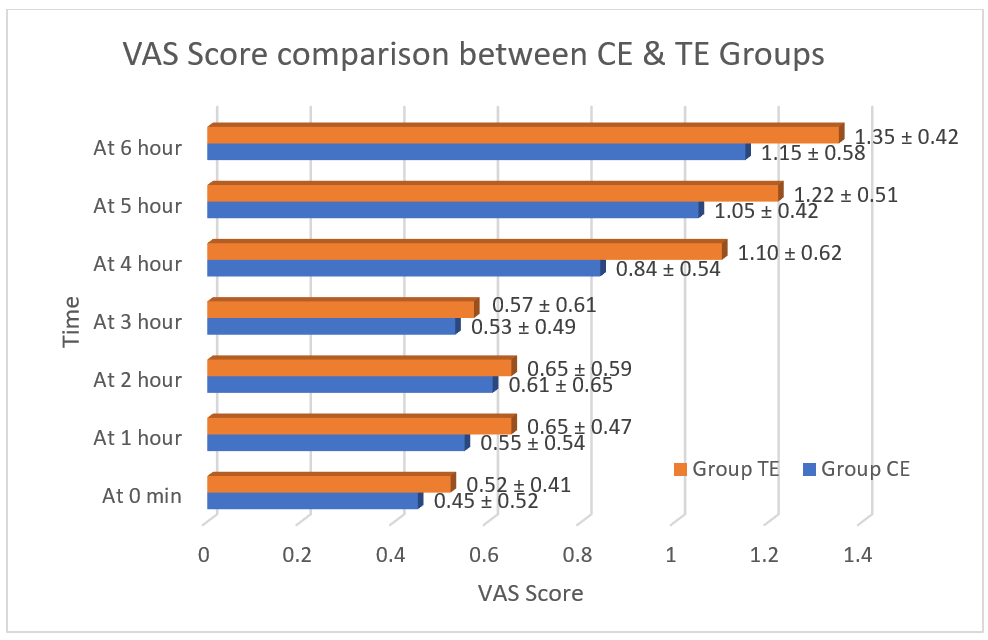
Figure 4: Quality of sensory block in respect to Visual analogue scale.
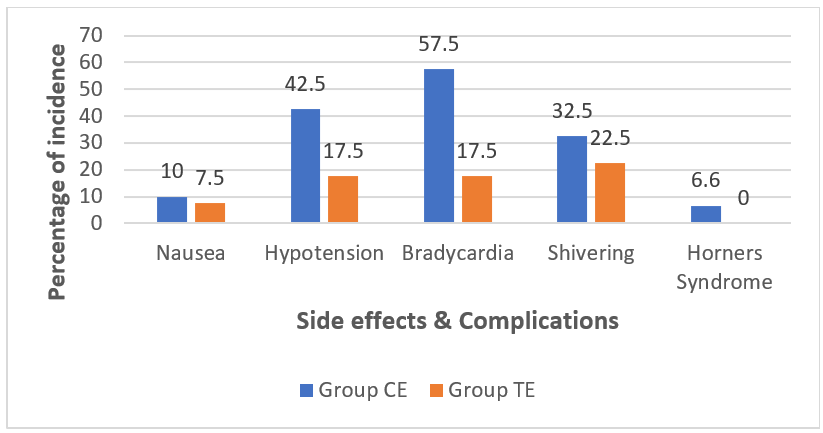
Figure 5: Side effects & Complications.
Discussion
Breast surgeries are on its rise and was traditionally being conducted under GA. Acute postoperative pain occurs in 40% women often necessitating the use of opioids. This aggravates the incidence of nausea and vomiting, impaired ventilation, resulting in prolonged hospital stay [10]. As concerns to the current study, both cervical epidural and thoracic epidural was found to be effective sole anaesthetic technique for conducting breast surgeries. It provides many advantages compared to GA which incorporates decreased incidence of nausea and vomiting, earlier hospital discharge and avoiding hemodynamic changes with tracheal intubation, can be used in patients with poor respiratory reserve, very low ejection fraction, CKD, and ASA 3 or 4 patients [10,11].
In general, the infrequent use of TEA for oncologic breast surgeries may be attributed to fear of potential complications like spinal cord injury, respiratory complications, spinal/epidural hematoma, and post-dural puncture headache. However, with experience and due precautions, these complications are extremely rare and the incidence of neurological injury is 0.01-0.001%. [12] The breast, axillary nodes, and pectoral muscles derive their innervation from multiple sources, including branches from the first to the sixth intercostal nerves, brachial plexus, intercostal brachial nerve (T2-T3), supraclavicular nerve, and lateral and medial pectoral nerves from the cervical plexus. As per existing literature, both the regional techniques are widely used for postoperative analgesia, but there are very few studies and case reports suggested their use as sole anaesthetic technique.
In the current study, significant fall in both SBP and DBP was noted from 15 min to the offset of blockade in group CE; whereas significant fall only in DBP at 10,15, 30 min in group TE. Kulkarni K et al [13] noted a significant fall in MAP at 30 min after CE for MRM patients. This late fall in BP could be due to deployment of lower concentration (0.25%, 10 ml) of bupivacaine in their study compared to (0.5%, 10 ml) drug in current study. An early and prolonged fall in SBP and DBP from 5 min to 50 min from baseline in thoracic epidural breast surgery in the study done by Ahmed AM et al [14] could be due to the usage of large volume of bupivacaine, i.e., 15 ml along with 0.5 mcg/kg fentanyl.
A significant fall in mean HR was observed in both cervical and thoracic epidural group but it was prolonged in case of thoracic epidural. Kulkarni K et al [13] who studied in cervical epidural and Helal SM et al [15] who did study in thoracic epidural noted a significant drop in the mean HR just like the current study. But there was a late (at 30 min) and prolonged fall in HR (up to 120 min) in the study of Kulkarni K et al which might be due to use of 10 ml of 0.25% of bupivacaine in conjunction with 25μg of fentanyl while Helal SM et al monitored haemodynamic only up to 60 min [13,15].
The change in respiratory rate observed in cervical epidural group in current study was same as observed by Kulkarni K et al in their study in cervical epidural [13]. No change in respiratory rate was found in TE group, just like finding of Ahmed AM et al who did their study in thoracic epidural anaesthesia [14].
The mean onset of sensory and motor blockade was shorter in group CE compared to group TE; although it was statistically insignificant. However, the duration of both sensory & motor blockade was significantly prolonged in Group CE. So, in our study, we found an exceptional block trait with group CE compared to group TE. Also, Georgiou L et al observed a superior blockade characteristic in Cervical Epidural group as compared to Thoracic Epidural group in the treatment for head and neck cancer pain [16]. This difference can be attributed to the more time required for the drug to penetrate the CSF when it is administered in the thoracic region. This is in agreement to the findings of the other studies that support the rostral spread of analgesic in to the CSF after epidural administration [17-20].
Apart from these patient-patient variations, drug dosage, quality difference also adds upon to these differences. Duggan J et al inferred that the larger dose of bupivacaine produced the fastest onset and longest duration of blockade [21].
Mean blockade level achieved were similar in both groups (9.2±0.52 segments in group CE vs 9.5± 0.65 segments in group TE) with maximum of 11 segments and minimum of 8 segments in both groups. Kulkarni K et al observed blockade of maximum 12 segments in their study on cervical epidural [13]. Whereas Vineetha P et al noted blockade of maximum 12 segments and minimum 6 segments in their study on thoracic epidural [6]. These observations were reminiscent of the current study.
Mean VAS score for quality of sensory blockade was similar in both groups. Kulkarni K et al noted that 24 hr VAS score in CE bupivacaine group was 2.9, which was lower like in the current study even though comparison could be difficult due to two observation time frames used [13]. Helal SM et al noted mean VAS score of 1.20±0.76 at 6 hr in the TE group for mastectomy like our study (1.26±0.33 in group CE vs 1.54±0.3 in group TE, p=0.1835) [15]. Jalakandan B et al observed mean VAS score of 1.56±0.65 at 6 hr in the TE group for modified radical mastectomy which was similar to our study [12].
Sedation supplementation of analgesic was needed in 10% of patients in group CE and 15% patients in group TE even though it was statistically insignificant. There were no studies to evaluate this parameter too to compare and comment. Kulkarni K et al in their study of comparison between the efficacy of 0.25 % bupivacaine with 0.375% ropivacaine in cervical epidural for radical mastectomies also observed sedation requirement in 20% and 30% patients in both the groups with similar sedation score, respectively [13]. In the study conducted by Helal SM et al who compared thoracic epidural and ultrasound‑guided thoracic paravertebral block in perioperative pain management for mastectomy, there was statistically no significant difference among the studied groups in terms of the total fentanyl required during surgery [15].
Overall nausea, hypotension, bradycardia, shivering and Horner’s syndrome was observed in 10%, 42.5 %, 57.5%, 32.5%, and 6.6% patients, respectively in group CE, whereas, 7.5%, 17.5%, 17.5 %, 22.5% and 0% patients, respectively in group TE. Kulkarni K et al noted hypotension and bradycardia in 25% patients while none had nausea/vomiting following cervical epidural [13]. Ravi PR et al also observed nausea/vomiting in 5.5% patients and bradycardia in 2.5% patients following thoracic epidural [22]. Vineetha P et al noted hypotension, bradycardia and discomfort in 31%, 8.8% and 4.4% patients, respectively following thoracic epidural [6].
Small sample size, limited study duration, lack of a baseline pulmonary function tests and blind technique were few of the limitations of our study.
In future the same study can be protracted with utilisation of USG for epidural space identification and catheter insertion instead of blind technique, stretching the study into extended postoperative period for better post-operative analgesia. Usage of other drugs like ropivacaine or different concentrations or volumes of drugs with adjunct can also be tried.
Conclusion
Though both thoracic epidural and cervical epidural are effective in providing anaesthesia and analgesia for breast surgery; thoracic epidural approach serves more safer anaesthesia in terms of lesser haemodynamic variations, lower side-effects and complications, however cervical epidural provides superior blockade characteristics compared to thoracic epidural blockade.
References
- Arora G. Cervical epidural anaesthesia for carcinoma breast surgery as the sole anaesthesia modality. Journal of Anaesthesia and Critical Care Case Reports, 2019; 5(2): 6-9.
- Stevens RA, Stevens MM. Cervical and high thoracic epidural anesthesia as the sole anesthetic for breast surgery. Techniques in Regional Anaesthesia & Pain Management, 1998; 2: 13–18.
- Nesmith RL, Herring SH, Marks MW, Speight KL, Efird RC, et al. Early experience with high thoracic epidural anesthesia in outpatient submuscular breast augmentation. Ann Plast Surg, 1990; 24: 299-303.
- Srivastava A, Jamil S, Khandelwal A, Raj M, Singh S. Thoracic Epidural Anesthesia for Modified Radical Mastectomy in a High-Risk Patient: A Case Report with Literature Review. Cureus, 2021; 13(6): e15822. doi: 10.7759/cureus.15822.
- Thoracic epidural anesthesia for modified radical mastectomy in a patient with cryptogenic fibrosing alveolitis: a case report. Trikha A, Sadhasivam S, Saxena A, Arora MK, Deo SV.J Clin Anesth, 2000; 12: 75–79.
- Vineetha P, Ramadass KT, Sajid B, Biji KP. A prospective observational study to assess the efficacy of thoracic epidural anaesthesia for mastectomy. Ann Int Med Dent Res, 2017; 3: 9-13.
- Wenk M, Massoth C, Pöpping DM, Möllmann M. Feasibility of cervical epidural anesthesia for breast cancer surgery.Anesthesiol Res Pract, 2017; 2017: 7024924.
- Michalek P, David I, Adamec M, Janousek L. Cervical epidural anaesthesia for combined neck and upper limb procedures. Anesth Analg, 2004; 99: v1833-1836.
- Höhener D, Blumenthal S, Borgeat A. Sedation and regional anaesthesia in the adult patient, BJA: British Journal of Anaesthesia January, 2008; 100 (1): 8-16.
- Patel A. Cervical Epidural Anesthesia as a Sole Technique in Breast Cancer with Multiple Comorbidities. J Anesth Clin Res, 2021; 12: 889.
- Hiremath VR. Thoracic epidural anesthesia for modified radical mastectomy-in type2 diabetes mellitus patient. J of Evolution of Med and Dent Sci, 2014; 3: 15002-15006.
- B J, S G. Is Thoracic Epidural Anesthesia a Better Alternative to General Anesthesia in Modified Radical Mastectomy Surgeries? IJAA, 2018; 5(10): 1757-1764.
- Kulkarni K, Namazi IJ, Deshpande S, Goel R. Cervical Epidural Anaesthesia with Ropivacaine for Modified Radical Mastectomy. Kathmandu Univ Med J, 2013; 42(2): 126-131.
- Ahmed AM, Ali H, Helal O, Sobhi T (2017) Comparative Study between Continuous Thoracic Epidural vs. Thoracic Spinal Anaesthesia in Breast Surgery. J Pain Relief, 2017; 6: 292. doi:10.4172/2167-0846.1000292.
- Helal SM, Abdel Aziz AA, Gab-Allah KA, Ramadan EG. Comparative study between thoracic epidural and ultrasound-guided thoracic paravertebral block in perioperative pain management for mastectomy. Menoufia Med J, 2019; 32: 1191-1196
- Georgiou L, Louizos A, Sklavou C, Manolopoulos L, Yiotakis I, Adamopoulos G. Cervical versus thoracic epidural morphine for the treatment of head and neck cancer pain. Ann Otol Rhinol Laryngol, 2000; 109(7): 676-678. doi: 10.1177/000348940010900711.
- Bromage PR, Camporesi EM, Durant PAC, Nielsen CH. Rostral spread of epidural morphine. Anesthesiology, 1982; 56: 431-436.
- Gourlay GK, Cherry DA, Cousins MJ. Cephalad migra-tion of morphine in CSF following lumbar epidural administra-tion in patients with cancer pain. Pain, 1985; 23: 317-326.
- Larsen VH, Iversen AP, Christiensen P, Andersen PK. Postoperative pain treatment after upper abdominal surgery with epidural morphine at thoracic or lumbar level. Acta Anaesthesiol Scand, 1985; 29: 566-571.
- Sullivan SR, Cherry DA. Pain from an invasive facial tumor relieved by lumbar epidural morphine. Anesth Analg, 1987; 66: 777-779.
- Duggan J, Bowler GM, McClure JH, Wildsmith JA. Extradural block with bupivacaine: influence of dose, volume, concentration and patient characteristics. Br J Anaesth, 1988; 61(3): 324-331. doi: 10.1093/bja/61.3.324.
- Ravi PR, Jaiswal P. Thoracic epidural analgesia for breast oncological procedures: A better alternative to general anesthesia. J Mar Med Soc, 2017; 19: 91-95.
- Doss NW, Ipe J, Crimi T, et al. Continuous thoracic epidural anesthesia with 0.2% ropivacaine versus general anesthesia for perioperative management of modified radical mastectomy. Anesth Analg, 2001; 92: 1552–1557.

