Comparison of Acute Physiological and Chronic Health Evaluation (APACHE-II), Sequential Organ Failure Assessment Score (SOFA) and CURB -65 Scores in Delta Variant of SARS-CoV-2 Patients Admitted in a Tertiary Care Hospital
Gajender Singh Ranga1,*, Sonu Singh1, Anupama Tandon2 and Ashish Goel1
1Department of Medicine, College of Medical Sciences and Guru Teg Bahadur, India
2Department of Radiology, Department of Anaesthesia University College of Medical Sciences and Guru Teg Bahadur, India
Received Date: 12/08/2024; Published Date: 22/10/2024
*Corresponding author: Gajender Singh Ranga, Department of Medicine, Department of Anaesthesia University College of Medical Sciences and Guru Teg Bahadur, India
Abstract
Background: SARS-CoV-2 infection is associated with considerable morbidity & mortality through direct invasion, immunological response and multisystem involvement. APACHE-II, SOFA AND CURB-65 scores are routinely used to predict outcome in various clinical conditions However, there is no consensus on best possible scoring system for SARS-CoV-2 infection. If in this group of patients, if appropriate scoring system is known then it can be used to predict outcome in these patients.
Aim: To study of APACHE-II, SOFA AND CURB-65 score in patients with SARS-CoV-2 infection.
Methods: This study of diagnostic accuracy included 30 patients >12 years old of either sex admitted in ICU tertiary care centre and tested positive for SARS-CoV-2 infection by RT-PCR and /or rapid antigen test and belonging to moderate and severe category as per guidelines of Government of India, Ministry of Health and Family Welfare. The sensitivity, sensitivity and cut-off score of APACHE-II, SOFA AND CURB-65 was estimated.
Result: The mean age of patients who were discharged or died was 60.33 ± 16.62 & 63.6 ± 15.66 years, oxygen saturation 80.20 ±8.53 and 95.87 ±2.20 percent at room air and on oxygen therapy respectively. The oxygen saturation of patients who died was 64.00 ± 9.86 and 92.53 ±2.56 percent at room air and oxygen therapy respectively. The area under curve for APACHE-II, SOFA andCURB-65 score was 100,100 and 83.3% and cut-off values 12.50, 5.50 & 1.50 respectively.
Conclusion: APACHE-II and SOFA are very sensitive and robust scores for predicting mortality in patients with SARS-CoV-2 infection while CURB-65 scoring system is also good but predictive value is not as good as APACHE-II or SOFA scores.
Keywords: Predictive value; SARS-CoV-2; APACHE-II; SOFA; CURB-65 score
Introduction
SARS-CoV-2 was first identified in Wuhan, Hubei Province, China in the month of December, 2019 and after that spread rapidly. WHO declared it pandemic on March 11 [1].
The virus affects all the systems of the body but respiratory system being the main one. It uses the catalytic domain of ACE2 receptor on the pneumocytes for binding with its S (spike) high affinity protein. Though it affects both types of pneumocytes, type 2 cells are comparatively more vulnerable [2]. It is observed that some patients deteriorate rapidly as it involves multiple systems of body, leading to considerable morbidity and mortality.
Apart from typical sign and symptoms of fever, cough, fatigue, diarrhoea, dyspnoea, shortness of breath, loss of taste and smell, etc. It is observed that some patients rapidly deteriorated developing respiratory failure, acute respiratory distress syndrome (SARS) and even multiple organ failure, leading to death.
In context of SARS Cov-2, there is ongoing interest in identification of reliable prognostic markers. Acute Physiological and Chronic Health evaluation (APACHE-II) [3], and Sequential Organ Failure assessment (SOFA) [4] already established prognostic markers in critically ill patients including those with SARS-CoV-2 but the best score is still not known. Confusion, Urea, Respiratory Rate, Blood Pressure, Age 65. CURB-65 [5] is a scoring system for pneumonias but not well studied in patients with SARS-CoV-2 infection. Thus, a need was felt to establish a robust scoring system with high sensitivity, specificity and predictive.
Material and Method
The study was conducted at wards and ICU of a tertiary care centre.
Total of 30 subjects classified as belonging to moderate and severe category were include in the study. The subjects were categories into 2 groups and as per Guidelines of Ministry of Health and Family welfare of Govt. Of India [6], patients of mild category were not admitted
- Group A = 15 Patients discharged from GTB hospital successfully after SARS-CoV-2 infection.
- Group B = 15 Patients who succumbed to SARS-CoV-2 infection.
Prior to enrolment in study, Hospital Ethical Committee clearance was taken. Consent was taken from the nearest kin on phone since most patients to be very sick and attendants were not allowed to enter ICU. Patients more than 12 years of age who tested positive for SARS-CoV-2 infection on rapid antigen detection test using commercially available kit/and or Elisa for RT-PCR were include in the study. After admission each subject was subjected to detail clinical evaluation
After clinical evaluation within 24 hours-48 hours of admission APACHE-II, SOFA & CURB-65 questionnaire was administered and score of each scoring system was calculated after results of following investigations;
All patients were subjected to following investigations:
- Hemogram- Hb, TLC, DLC, platelets
- Kidney function test- blood urea, serum creatinine, serum sodium, serum potassium
- Liver function test-serum albumin/globulin, serum bilirubin direct/indirect
- serum alkaline phosphatase
- SGOT & SGPT (serum amylase/lipase)
- ECG
- chest x-ray
- Arterial blood gas evaluation
All three scores were calculated & correlated with outcome data.
The data was further subjected to following statistical analysis to find the specificity, sensitivity, cut-off values of each scoring system.
Statistical Analysis
SPSS 20 was used to analyse the data
Based on clinical evaluation and laboratory reports we identified the cut off value of these indicators to be the upper or lower limits of within normal range, values were presented as mean ± SD or as number and percentage. The difference of categorical values of between the survivors and death was compared by chi-square test or Fisher exact test. Continuous variables were compared, using Student`s t test. Spearman correlation and analysis was performed among significant variables and univariate analysis. Receiver operating characteristics (ROC) was analysed to evaluate and compare the predictive value of theses 3 scoring system. The p values of less than 0.005 was considered significant.
Results
After analysis of data obtained from observations, following are the results after statistical analysis.
The age and sex distribution of patients in the study group has been described in Tables 1 and 2.
Table1: Distribution of cases according to age of the patient.
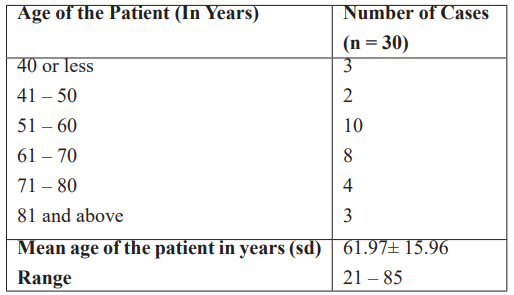
Table 2: Age and sex wise distribution of patients.
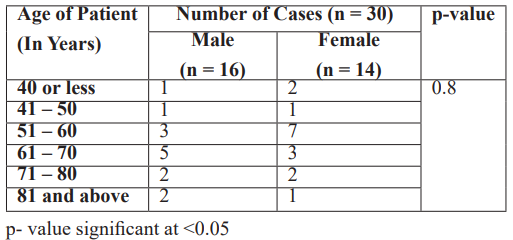
Table 3: Comparison of haematological and biochemical parameters between the two groups. (n = 30).
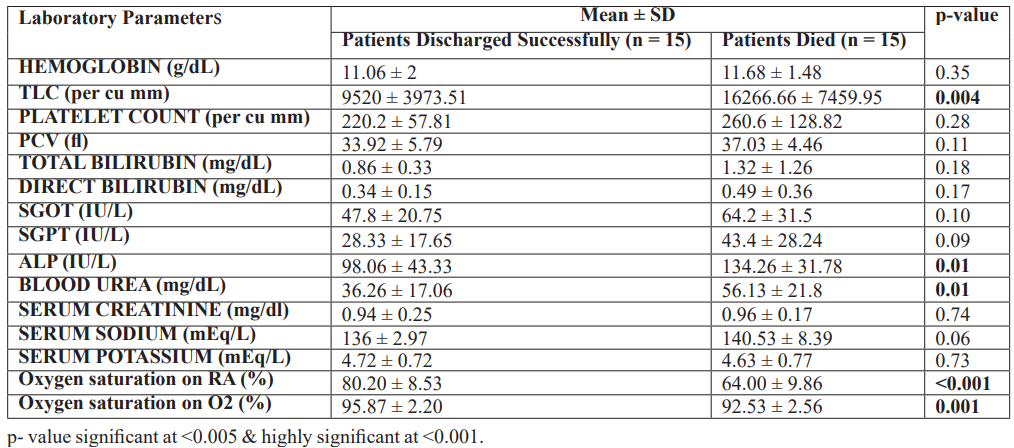
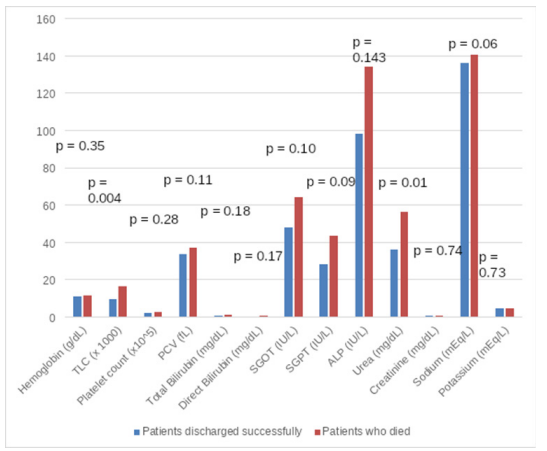
Figure 1: Comparison of hematological and biochemical parameters between the two groups.
Table 4: Results of APACHE-II, SOFA & CURB-65score between the two groups (n = 30).
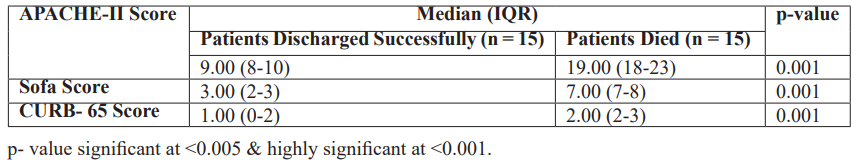
The above table shows the results of APACHE-II, SOFA and CURB-65 scores. As can be seen that patients who died had significantly higher values of each score (p =0.001)
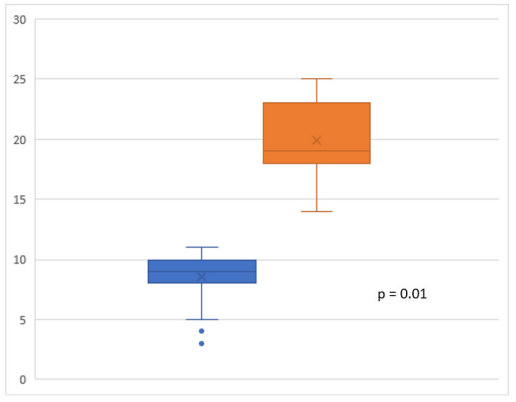
Figure 2: Comparison of APACHE-II score between the two groups.

Figure 3: Comparison of SOFA score between the two groups.
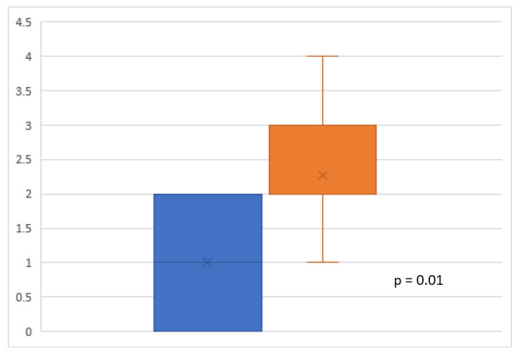
Figure 4: Comparison of CURB-65 score between the two groups.
ROC Curve regarding APACHE-II, SOFA & CURB-65 score has been depicted in figure no 7.
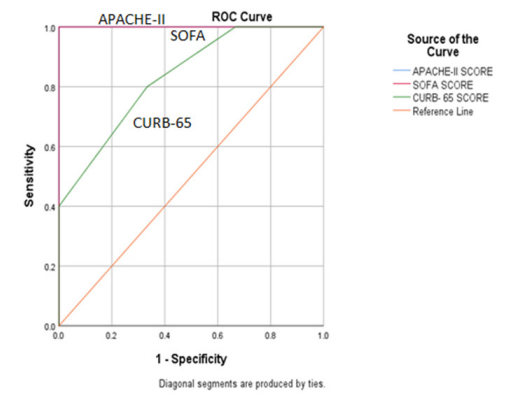
Figure 5: ROC curve to assess diagnostic validity of various scores to predict clinical outcome. (n=30).
Diagnostic validity of APACHE-II, SOFA & CURB-65 has been described in table 6
Table 5: Show diagnostic validity of various scores to predict clinical outcome. (n = 30).
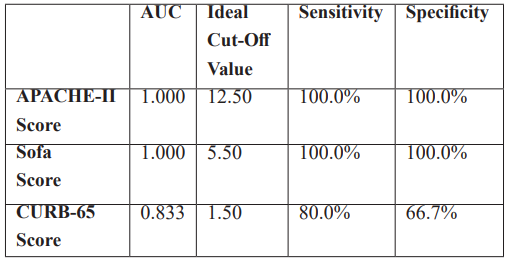
The above figure and table show the ROC curve constructed to identify ideal cut-off values for APACHE-II, SOA and CURB-65 scores. As can be observed, the area under the curve for APACHE-II and SOFA score was 100%, while for CURB-65 was 83.3%. At the ideal cut-off value of 12.50 for APACHE-II score, the sensitivity and specificity of APACHE-II score in classifying the study group according to the patient outcome was 100%. Similarly, at SOFA score of 5.50, the sensitivity and specificity of SOFA in classifying the study group according to the patient outcome was 100%. At a cut-off value of 1.50, CURB-65 score had a sensitivity of 80% and specificity of 67% in identifying patients according to outcome.
Discussion
The analysis of data in our study revealed that 18 (60%) of our patients were between 50-70 years of age (Table 1, 2). It highlights the fact that majority patients affected were in relatively elderly age group. These possibly could also be due to the fact that younger patients (<12 years) were excluded from the study & those (>70 years) are more likely to remains at home due to various other disabilities and lack of family support and hence are less likely to get exposed to SARS-CoV-2 infection. In Gao et al.’s study [7], which included older (≥65 years) COVID-19 patients, the deceased group had more morbidities including cardiovascular diseases (49% vs. 20%, P<0.001), respiratory diseases (51% vs. 11%, P<0.001), chronic kidney disease (29% vs. 5%, P<0.001) and cerebrovascular disease (20% vs. 3%) than the discharged group. In a study by Vrillon et al [8] included the very elderly (≥85years) COVID-19 patients, the non-survivor group had more cardio-neurovascular diseases (68.2% vs. 37.0%, P=0.013), more complications like acute respiratory disease syndrome (95.5% vs. 1.9%, P<0.001), and needed more frequent treatment with oxygen (95.5% vs. 46.3%, P<0.001) compared with the survivor group. Yong Sub Na et al [9] also reported in-hospital mortality rate of elderly patients with severe SARS-CoV-2 was 25.5%. Non-survivor group were older, had more underlying comorbidities, frailer, and more severe by severity scores than the survivor group.
Infection rates among males & females were almost equals (Table 2). Chen J et al. [10] also in their study did not find any significant differences w.r.t age ((>65 all patients 106(63.5), survival 101(62.7), and dead 5(83.3), age <65 all patients 61(36.5), survival 60(37.3), and dead 1(16.7) and sex, (male all patients 84(50.3), survival 78(48.4), and dead 6(100.0), female all patient 83(49.7), survival 83(51.6) and dead 0(0.0).
We did not includes patients with mild infection (spo2 >94%)(6) as per guidelines of govt. as these patients were categorised as having mild illness and so were not candidate for hospital admission. O2 saturation difference was highly significant between those who died and survived respectively (p<0.001) (Table 3) & these patients were so severely ill that even on O2 therapy the difference of oxygenation was highly significant (p<0.001) (Table 3). Hypoxia is extremely detrimental to all body organs and is main factor in pathogenesis of multi organ failure. CURB-65 score in our study was significantly different between survivors & those who did not survive (Median [IQR] 1.00(0-2) & 2.00(2-3)) respectively (Table 4) highlighting presence of severe infection in our patients who died (p=0.001) (Table 4, Figure 2). Further large no of our patients required mechanical ventilators due to inclusion criteria. Invasive ventilators has been reported to be having highly significant correlation with mortality(p<0.001)(11) due to ventilators associated pneumonia, barotrauma and lower cardiac output and various other factors.
Investigation done on our patients who died revealed significantly higher total leucocyte count (p=0.004) (Table 3, Figure 1). Atieh et al [12] in a meta-analysis of 19 articles reported leucocytosis (the lymphocyte counts lower than 0.8 × 109 /L is associated with COVID-19 severity, number of neutrophil higher than 3.5 × 109 /L is associated with a poor clinical outcome). Further Haung G et al [13]. Have reported that leucocytosis at time of admission was associated with worse prognosis in this study patients categorized as having severe illness tended to have lower lymphocyte count ( pooled MD -0.36, 95% CI -0.50 to 0.27; p<0.00001) and higher leukocyte count ( pooled MD 1.32, 95% CI 0.62 to 2.02; p,0.00001). SARS Cov-2 induces severe inflammation resulting even cytokine storm which is directly associated with high mortality by causing severe lung injury. Chen J et al [14] reported severe positive correlation with mortality (p<0.001). Further neutrophil release reactive oxygen molecules & metalloproteinase which is also injurious to various tissues.
Results of our study show that APACHE-II score ranged from [8-10 (Median IQR) 9.00] and [18-23 (Median IQR) 19.00] respectively among those who survived & those who expired the difference was statistically highly significant (p=0.001) (Table 4, Figure 3). The ROC curve showed Area undercover 1.0 with Ideal cut-off value 12.50 with 100% specificity & sensitivity signifies that this score is a robust score for predicting adverse outcome. Our results are similar to that of Beigmohammadi M Taghi et.al [11] who reported mortality rate for ICU based on APACHE-II score value mean APACHE-II and mean SOFA scores were significantly higher in the non-survivor than in the survivor group (14.4 ±5.7 vs. 9.5 ± 5.1, p≤0.001, 7.3 ± 3.1 vs.3.1 ± 1.1, p≤0.001, respectively). Their study showed an increase in mortality rate at higher score (p≤0.001) at cut off score of 13. Zou et.al.(15)reported APACHE-II score(23.23 ± 6.05 vs. 10.87 ± 4.40; p<0.001) and SOFA score at (4.56 ± 2.81 vs. 1.63 ± 1.25; p<0.001) were higher in those who died . They further reported that APACHE-II was a better predictor of hospital mortality than SOFA score.
In our study, ROC curve regarding SOFA score indicates that AUC was 1.00, at ideal cut-off value 5.50 had sensitivity & specificity 100% (Table 5, Figure 5). Indicating that it is good score to predict adverse outcome at time of admission of patients. Nays(9)reported that SOFA score showed the best performance in predicting the prognosis of elderly patients as compared to APACHE-II & CURB-65 score (AOC =0.766 & p<0.001). They concluded that SOFA score is an efficient tool for assessing in hospital mortality in elderly patients with severe SARS-CoV-2 in their study APACHE-II score was (11.0 (8.0-14.0) & 14.0 (11.0-19.0) in survivor and non-survivor respectively (p<0.001). Similarly, SOFA score was1.0 (0.0-3.0) & 4.0(2.0-8.5) respectively in survivors than on survivor with p-value<0.001) and CURB-65 score was (1.0 (1.0-2.0) & 2.0(1.5-3.0) in survivor and non-survivor respectively (<0.001.) Beigmohammadi M Tyagi [11] also reported that mean SOFA score was significantly higher in non survivors than in survivors group (7.3 ± 3.1 vs 3.1 ± 1.1, p≤0.001). AUC was 89.5% for SOFA and 73% for APACHE-II score & both scores showed increase in mortality at higher score value (p≤0.001) with cut off value of 13 for APACHE-II & 5 for SOFA score mean daily SOFA score had a predictive performance (p≤0.001).
Analysis of data in our study revealed that CURB-65 score in non survivors and survivors was 2.0 and 1.0 respectively & this difference was highly significant (p≤0.001) (Table 4, Figure 4). ROC curve to assess diagnostic validities of scale to predict clinical outcome showed that AUC was 83 within ideal cut off value 1.50 has sensitivity of 80% & specificity 66.7% (Table 5, Figure 5). It indicates that CURB-65 scoring system is also good scoring system to predict mortality at time of admission of SARS-CoV-2 infection. However, score does not seembetter than APACHE-II & SOFA score as sensitivity & specificity are less than both these scores (100% vs 80%).
So, the early identification of these parameters and judicious use of APACHE-II, SOFA & CURB-65 score can identify and risk stratify patients at risk of death & so to mitigate the adverse outcome appropriated therapeutic strategies should be instituted. APACHE-11 and SOFA scores are equally good, CURB-65 is not as good as these two scores but still a valuable predicative tool to categorize the patients with SARS-CoV-2 infection. So, we recommend further larger prospective studies to arrive at definitive conclusion.
Conclusion
APACHE-II at cut off value of 12.50 score is highly sensitive & specific for predicting mortalities in patients with SARS-CoV-2 infection. SOFA score at cut-off value of 5.50 score is highly sensitive & specific for predictive mortalities in patients with SARS-CoV-2 infection. CURB-65 at cut-off value of 1.50 score is also sensitive & specific for predicting mortalities in patients with SARS-CoV-2 infection. CURB-65 scoring system is also good scoring system but predictive values to risk stratify is less than APACHE-II & SOFA scores.
Limitations of Study: We could not include larger number of patients due to various constrains like strict isolation of patients. These results pertain to delta variant so this data may /may not be extrapolated to other variants of SARS-CoV-2.
Disclosures
Human subjects: Consent was obtained after Hospital Ethics Committee approval (number IECHR/2020/PG/46/38).
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: None.
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements: Dr.Sonu Singh, Dr.Gajender Singh Ranga & Anupama Tandon are joint first authors.
References
- Ramanathan K, Antognini D, Combes A, Paden M, Zakhary B, Ogino M, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID- research that is available on the COVID-19 resource centre - including this for unrestricted research re-use. 2020; January: 19–21.
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet, 2020; 395(10224): 565–574.
- Akavipat P, Thinkhamrop J, Thinkhamrop B, Sriraj W. Acute physiology and chronic health evaluation (Apache) II score – the clinical predictor in neurosurgical intensive care unit. Acta Clin Croat, 2019; 58(1): 50–56.
- Jain A, Palta S, Saroa R, Palta A, Sama S, Gombar S. Sequential organ failure assessment scoring and prediction of patient’s outcome in Intensive Care Unit of a tertiary care hospital. J Anaesthesiol Clin Pharmacol, 2016; 32(3): 364–368.
- Jones BE, Jones J, Bewick T, Lim WS, Aronsky D, Brown SM, et al. CURB-65 pneumonia severity assessment adapted for electronic decision support. Chest, 2011; 140(1): 156–163.
- Ministry of Health and Family Welfare. Goverment of India. ClinicalManagementProtocolforCOVID19, 2020; 1–22.
- Gao S, Jiang F, Jin W, Shi Y, Yang L, Xia Y, et al. Gao et al - Risk factors influencing the prognosis of elderly patients infected with COVID-19, 2020; 12(13): 12504–12516.
- Vrillon A, Hourregue C, Azuar J, Grosset L, Boutelier A, Tan S, et al. COVID-19 in Older Adults : A Series of 76 Patients Aged 85 Years and Older with COVID-19, 2020; 2735–2743.
- Na YS, Kim JH, Baek MS, Kim W, Baek A, Lee B, et al. In-hospital mortality prediction using frailty scale and severity score in elderly patients with severe COVID-19, 2022; 37(3): 303–311.
- Chen J, Liu B, Du H, Lin H, Chen C, Rao S, et al. Performance of CURB-65, PSI, and APACHE-II for predicting COVID-19 pneumonia severity and mortality. Eur J Inflamm, 2021; 19.
- Beigmohammadi MT, Amoozadeh L, Rezaei Motlagh F, Rahimi M, Maghsoudloo M, Jafarnejad B, et al. Mortality Predictive Value of APACHE II and SOFA Scores in COVID-19 Patients in the Intensive Care Unit. Can Respir J, 2022; 2022.
- Pourbagheri-sigaroodi A, Bashash D, Fateh F, Abolghasemi H. Clinica Chimica Acta Laboratory fi ndings in COVID-19 diagnosis and prognosis, 2020; 510(June): 475–482.
- Huang G, Kovalic AJ, Graber CJ. Prognostic Value of Leukocytosis and Lymphopenia for Coronavirus Disease Severity, 2020; 26(8): 1839–1841.
- Cheng PF, Wu H, Yang JZ, Song XY, Xu M Da, Li BX, et al. Pneumonia scoring systems for severe COVID-19: which one is better. Virol J, 2021; 18(1): 1–10. https://doi.org/10.1186/s12985-021-01502-6
- Zou X, Li S, Fang M, Hu M, Bian Y, Ling J, et al. Acute Physiology and Chronic Health Ev6aluation II Score as a Predictor of Hospital Mortality in Patients of Coronavirus Disease 2019. Crit Care Med, 2020; 48(8): E657–65.

