CT Features of Fibrous Dysplasia
Kaouthar Sfar*, Imane Mohammadine, Rachida Chehrastane, Kaoutar Maslouhi, Omar El Aoufir and Laila Jroundi
Emergency Radiology Department of the University Hospital Ibn Sina, Rabat, Morocco
Received Date: 04/08/2024; Published Date: 21/10/2024
*Corresponding author: Kaouthar Sfar, Emergency Radiology Department of the University Hospital Ibn Sina, Rabat, Morocco
Fibrous dysplasia, a genetic developmental disorder of skeletal system, originates from sporadic mutations in the GNAS gene, which encodes the α-subunit of the Gs stimulatory protein [1-3].
Bone alterations involve the replacement of the normal marrow space within the affected bone with fibro-osseous tissue, resulting in the deformation of the bone due to poorly organized and structurally unstable fibrous tissue [2,3].
Fibrous dysplasia can involve one single bone (monostotic) or many bones (polyostotic)with skin pigmented lesions (Jaffe's type) and endocrine disorder (McCune-Albright syndrome) [4].
Patients with polyostotic forms are typically diagnosed during childhood or adolescence, often presenting with symptoms such as pain, pathologic fractures, swelling, or vaginal bleeding. In contrast, those with monostotic forms are usually asymptomatic, leading to the diagnosis being made incidentally [2].
Computed Tomography (CT) is the examination of choice for diagnosis and follow-up, due to its superior ability to provide detailed images of the bone and accurately assess the extent of the lesion especially for craniofacial lesions [5]. CT imaging features include [3] (Figure 1):
- Smooth and homogeneous ground glass.
- Dense and sclerotic lesion.
- Cystic lesion.
- Well circumscribed borders.
- Expansion of the affected bone and endosteal scalloping with persistence of smooth cortical thinning.
- The lesion may be surrounded by a layer of thick sclerotic reactive bone: rind sign.
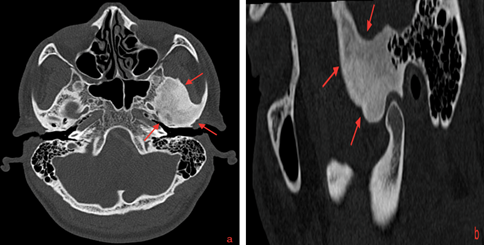
Figure 1: Axial(a) and sagittal (b) computed tomographic images of craniofacial fibrous dysplasia (red arrow) showing expansive mixed lesion with ground glass opacity involving temporal and sphenoid bones.
References
- Delavaud C, Lincot J, Debray M, Schouman-Claeys E, Dallaudiere B. An incidental posterior mediastinal mass. Diagn Interv Imaging, 2014; 95: 121-122.
- BerKmen YR, Zalta BA. Extramedullary Hematopoiesis. Radiology, 2007; 245: 905-908.
- Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK. Typical and atypical presentations of extramedullary hemopoiesis. AJR, 2002; 179: 1239–1243.
- Laamrani F, Dafiri R. [Large hilum in a child with sickle cell anemia. Extramedullary hematopoiesis]. Arch Pediatr, 2015; 22: 88-89, 104-105.
- Psichoglou H, Malagarl K, Spanomichos G. Mediastinal extramedullary hematopoiesis in hemolytic anemia. JBR-BTR, 2004; 87: 150-151.
- Maazoun F, Gellen Dautremer J, Boutekadjirt A, Pissard S, Habibi A, Bachir D, et al. [Symptomatic extramedullary haematopoiesis in β-thalassemia: A retrospective single centre study]. Rev Med Interne, 2016; 37: 5-12.
- Ogier M, Kerjouan M, Libessart T, Merzoug A, Leroyer C, Desrues B, et al. [Posterior mediastinal mass]. Rev Mal Respir, 2015; 32: 959-962.
- Chourmouzi D, Pistevou-Gompaki K, Plataniotis G, Skaragas G, Papadopoulos L, Drevelegas A. MRI findings of extramedullary haemopoiesis. Eur Radiol, 2001; 11: 1803–1806.

