Could the Greater Consumption of Chicken be Fueling the Global Ischemic Heart Disease and Stroke Pandemic? A Chicken-Cholesterol versus Corned Beef-Cholesterol Absorption Kinetics Case Study
Cocores JA1,2*
1Founding Director, Culinary Medicine, Psychephysics Mediated Research Laboratories (PMR Labs), 5219 D Wallis Road, West Palm Beach, FL 33415
2Research Associate, CarpeVITA Genomics, Newport, DE 19804
Received Date: 23/06/2020; Published Date: 21/07/2020
*Corresponding author: Department of Psychiatry, University of Florida College of Medicine & McKnight Brain Institute, Gainesville, FL, USA. E-mail: drjac11@bellsouth.net
Case Study
As of 08/12/2018, health organizations [1-3] and clinical entities [4-5] have recommended eating more chicken to reduce risk prevalence and either postpone or prevent the genesis of ischemic heart disease (IHD) and stroke, reasoning that chicken contains lower amounts of cholesterol than corned beef.
A review of the literature revealed no scientific based absorption, kinetics or bioavailability study that supported the notion that chicken-cholesterol translates into low-density lipoprotein (LDL) plasma levels at a lower rate than corned beef-cholesterol.
The following case study was designed to prompt more extensive investigations regarding the absorption and elimination dynamics of chicken-cholesterol versus corned beef-cholesterol
Method
Mr. M. signed a consent form to participate in this study after he had carefully read the protocol for the total cholesterol, triglycerides, very low-density lipoprotein and LDL detoxification, chicken-cholesterol challenge, and corned beef-cholesterol challenge [6]. In addition, he understood that once his LDL plasma level was reduced to approximately normal, he would begin the corned beef-cholesterol challenge by first having a fasting lipid panel drawn. Then, Mr. M. would consume 165 mg of Amadori product [7] containing or boiled, corned beef-cholesterol within an alkaline green fiber diet consisting of green shakes made of blended gandules, lima beans, kale and first-pressed olive oil, and cucumber, zucchini, celery and avocado salads. He then would return to the lab the following morning in order to have a lipid panel drawn. Also, the aforementioned procedure would be repeated consuming 210 mg of slightly melanoidin coated [7] or broiled, skinless boneless chicken pectoral muscle-cholesterol. Moreover, the corresponding exogenous cholesterol value would be divided by the corresponding delta LDL, which would yield a lipoprotein index (LI) for corned beef and chicken. The lower the LI, the higher the translation rate from corporally exogenous cholesterol to the subject’s plasma LDL levels.
Results
Mr. M. was a 64-year-old with a history of atrial fibrillation, IHD and episodes of disorientation and motor collapse. His LDL levels ranged from 149 to 193 mg/dL (Normal Range = 0-99 mg/dL) from 08/29/2016 through 03/24/2017. Mr. M. stopped taking his statin, antihypertensive, and antithrombotic medication in the fall of 2017 because he deemed them ineffective and costly and that they were associated with neurological, cardiac, and gastrointestinal side effects.
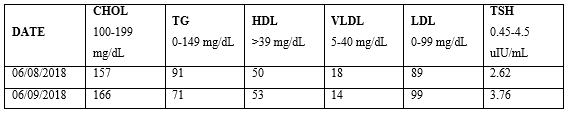
Implementing the procedure set out above, Mr. M’s LDL increased by 10 mg/dL/day after consuming 165 mg of corned beef-cholesterol on 06/08/2018 (Table 1). Hence, his LI for corned beef was 16.5 (165 mg corned beef-cholesterol/10 mg/dL = delta LDL).
Table 1: Corned Beef-Cholesterol Challenge.
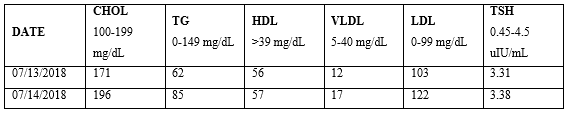
The subject’s LDL increased by 19 mg/dL/day after consuming 210 mg of chicken-cholesterol on 07/13/2018 (Table 2). Therefore, the subject’s LI for chicken was 11.1 (210 mg chicken-cholesterol/19 mg/dL = delta LDL).
Table 2: Chicken-Cholesterol Challenge.
Mr. M. assimilated, absorbed and/or translated exogenous cholesterol into corporal LDL more readily from chicken than from corned beef.
Conclusion
Chicken-cholesterol was 49% more bioavailable than corned beef-cholesterol in the subject studied. Is Mr. M. a genetic outlier or do these results translate to a larger subgroup or to the populace? These somewhat counterintuitive and paradoxical results warrant further investigation.
Disclosure
Dr. JA Cocores has nothing to disclose.
References
- DASH Eating Plan. National Heart, Lung, and Blood Institute.
- Nutrition Tips for Stroke Survivors. The American Heart Association/American Stroke Association.
- The American Heart Association’s Diet and Lifestyle Recommendations. American Heart Association.
- Gidding SS, Dennison BA, Birch LL, et al. Dietary Recommendations for Children and Adolescents: A Guide for Practitioners. Pediatrics. 2006;117(2):544-59.
- Lifestyle Changes to Help You Manage HeFH. WebMD.
- Cocores JA. Could the greater consumption of fish and chicken be contributing to the global ischemic heart disease and stroke pandemic? psychepubs.com.
- Zhang Q, Ames JM, Smith RD, Baynes JW, Metz TO. A Perspective on the Maillard Reaction and the Analysis of Protein Glycation by Mass Spectrometry: Probing the Pathogenesis of Chronic Disease. J Proteome Res. 2009;8(2): 754-69.

