Prenatal Diagnosis, Neonatal Gastric Outlet Obstruction and Minimal Invasive Surgical Excision of Pyloric Gastric Duplication Cyst
Indre Zaparackaite1, Shailinder Jit Singh2, Debashish Bhattacharya3, Swamy KB4, Rafael Cavalcante Correia5, Partap Kumar Midha6 and Ramnik V Patel7,*
1Department of Pediatric Surgery, Emergency’s Children’s Surgical Hospital, Entebbe, Uganda
2Department of Pediatric Surgery, Nottingham University Hospitals, Nottingham, UK
3Department of Pediatric Surgery, Sultan Qaboos Hospital, Salalah, Sultanate of Oman
4Lincoln University College, Lincoln University, Kuala Lumpur, Malaysia
5Santa Casa de Tatui Gen Hospital, 330 Maneco Pereira Road, Tatui 18273000, Sao Paulo, Brazil
6J. Watumull Global Hospital & Research Centre, Delwara Road, Mount Abu, Rajasthan, India affiliated to Medical Faculty of God Fatherly World Spiritual University, Mount Abu, Rajasthan
7Departments of Pediatrics and Ped Surgery, Postgraduate Institute of Child Health & Research and KT Children Govt University Teaching Hospital, Rajkot 360001, Gujarat, India
Received Date: 02/08/2024; Published Date: 21/10/2024
*Corresponding author: Mr. Ramnik V Patel MD, MS, MCh, LL M, DCH, DNBPS, FRCSEd, FRCS Ped, FEBPS, FACS, FAAP, Director-Professor, Department of Pediatric Surgery, Postgraduate Institute of Child Health and Research and K T Children Government University Teaching Hospital Rajkot 360005, Gujarat, India
Abstract
Gastric pyloric duplication cyst is rarely diagnosed on prenatal diagnosis by ultrasound although it leads to a polyhydramnios which should alert for search of a possible upper gastrointestinal obstruction and the duplication cyst has its own signature on the cyst wall. The neonatal presentation with complete gastric outlet obstruction is uncommon. Minimal invasive approach is preferable to traditional standard exploratory laparotomy. We wish to report an extremely rare and interesting case of an infant with gastric pyloric duplication cyst diagnosed prenatally and who had presented as neonatal complete gastric outlet obstruction diagnosed postnatally. The patient underwent minimal invasive periumbilical exploration and complete excision of the duplication cyst uneventfully.
Keywords: Alimentary tract; Antenatal diagnosis; Cyst, duplication; Fetal; Gastric outlet obstruction; Minimal invasive; Neonate; Periumbilical; Pyloric
Abbreviations: GPAL-Gravida, Parity, Abortion, Living child; APGAR-Appearance, Pulse, Grimace, Activity and Respiration; PDC-Pyloric Duplication Cyst; SMA-Superior Mesenteric Artery; SMV-Superior Mesenteric Vein; CT-Computed Tomography; MRCP-Magnetic Resonance Cholangiopancreatography
Introduction
Our team has an extensive experience of prenatal diagnosis [1], fetal surgery and minimal invasive neonatal interventions [2,3,4] and various alimentary tract duplications but have never come across such an exciting case with several issues and implications with regards to the diagnosis and subsequent therapeutic interventions [5-12]. While anecdotal case reports describe an isolated prenatal diagnosis [13], a very rare neonatal presentation with complete gastric outlet obstruction [14] or a minimal invasive treatment of pyloric gastric duplication [15]; we wish to share our exciting experience in the management of such an interesting case combining all three of these features in one case.
Case Report
A 22-year-old G1P1A0L0 pregnant woman presented for prenatal ultrasound scan at which she was diagnosed with polyhydramnios and baby boy had been noted to have pyloric duplication cyst in the gastric outlet area of the stomach in the abdomen. The mother was monitored during pregnancy which was uneventful and underwent an uncomplicated delivery at 38 weeks of gestation of apparently normal-appearing boy.
At birth, the patient had an apparently healthy appearance with normal APGAR scores, was doing well with no respiratory difficulties and normal physical examination findings but started non bilious vomiting with upper abdominal distention, was unable to tolerate breast feeds and had not passed meconium on day one. Nasogastric tube was passed easily without any hold up in the esophagus, had large nonbilious aspirates and vital signs were within normal limits. Abdominal examination revealed fullness and palpable ill defined mobile soft mass in the junction of right hypochondrium and epigastrium.
The laboratory values at birth were normal. Abdominal radiograph showed distended gastric bubble and paucity of gas in the distal alimentary tract (Figure 1A and B). Abdominal ultrasonography scans showed a unilocular cyst at the antropyloric region measuring 2.5cm x 3cm x 2.3cm to the right, anteriorly and superiorly with a characteristic gut wall signature i.e., hyperechoic inner and hypoechoic outer wall (Figure 2A). Postero-inferiorly it tapered and has debris. The antral lumen appeared to be displaced inferiorly, to the left and posteriorly by the lesion and there were no signs of infantile pyloric stenosis. Ten ml water injected through nasogastric tube which showed no distal passage and confirmed pyloric duplication with complete gastric outlet obstruction. There was no biliary dilatation and rest of the abdomen was normal. Color Doppler studies revealed normal Superior Mesenteric Artery (SMA)/Superior Mesenteric Vein (SMV) orientation, no signs of midgut volvulus and the portal vein was patent and in normal position posterior to the duodenum (Figure 2B). Limited controlled water soluble upper gastrointestinal study with 30 ml contrast (Figure 3A and B) and after withdrawal of 40 ml of fluid double contrast film showed complete gastric outlet obstruction (Figure 4A and B).
We have given detailed information to parents about the final diagnosis of confirmation of prenatally diagnosed pyloric gastric duplication with complete neonatal gastric outlet obstruction allowing them to ask questions and concerns. The parents were given an overview of all available options of laparoscopic, minimal invasive periumbilical and traditional open exploratory laparotomy in the treatment for an informed decision. The parents decided to go for the minimal invasive periumbilical approach for possible excision of the pyloric duplication cyst.
The patient underwent examination under anesthesia and periumbilical exploration. At exploration, a large pyloric gastric duplication causing complete gastric outlet obstruction was noted. A total excision of the pyloric duplication was carried out uneventfully. The post operative period was smooth, tolerated oral breast feeding very well and discharge home in 48 hours. At 12 month follow up, the patient is asymptomatic and thriving well.
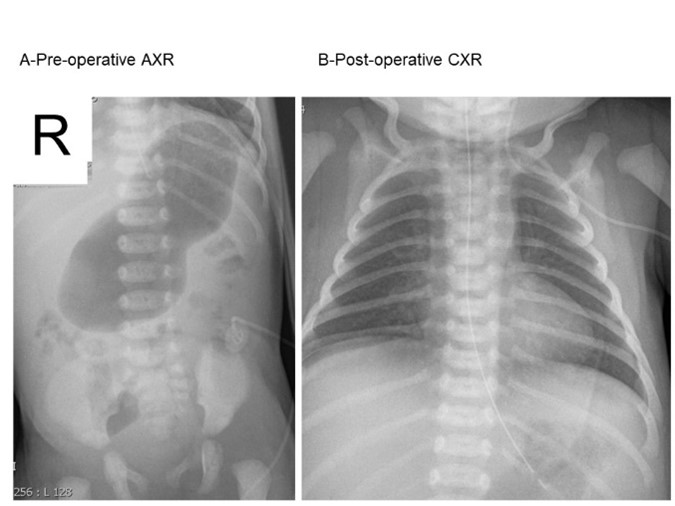
Figure 1: A Plain abdominal film at presentation B. Post-operative chest and upper abdominal film.

Figure 2A: Upper abdominal ultrasound-note classic double walls of the cyst wall B. Color doppler showing blood supply to the cyst wall and normal vessels.
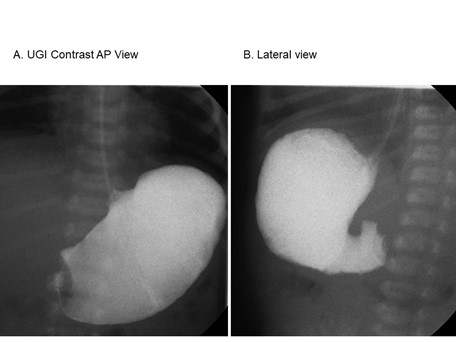
Figure 3: Upper gastrointestinal water-soluble contrast A. Anteroposterior view B. Lateral view-note no gastroesophageal reflux and complete gastric outlet obstruction.

Figure 4: Double contrast radiographs A. Anteroposterior view and B. Lateral view Note dilated gastric bubble with active peristalsis and even no air is passing down the pylorus.
Discussion
Pyloric Duplication Cyst (PDC) is an extremely rare congenital anomaly of the alimentary tract, whose clinical presentation often mimics those of hypertrophic pyloric stenosis in infancy rather than in the immediate neonatal period. Gastrointestinal duplications, mainly intestinal ones, are observed in 1 of every 4500 autopsies, predominantly in white males. Congenital pyloric duplication is extremely rare, few cases being described in the literature.and only six cases with prenatal diagnosis have been reported [13]. However, coexistent infantile pyloric stenosis and pyloric duplication has been reported once [16].
Prenatal diagnosis in our case was done easily with ultrasound scans as the typical alimentary tract duplication with hyperechoic inner and hypoechoic outer wall and associated hydramnios prompted us to look at the gastric outlook obstruction at the same time. Delivery at term at the tertiary centre with neonatal surgical services was helpful. Postnatal diagnosis with plain radiograph, ultrasound-doppler scans and limited water-soluble with or without double contrast study will suffice in most cases of isolated simple pyloric duplication. However, in combined gastric and pancreatic duplication cyst, axial imaging in the form of computed tomography (CT and magnetic resonance pancreatography (MRCP) may be helpful [17]. Endoscopic ultrasonography has been reported for gastric duplication but it involved general anesthesia in the neonate and best avoided [18]. Laparoscopy lends itself to better visualization of the duplication with relation to surrounding structures, especially if pre-operative imaging has not definitively identified the anomaly and can proceed to surgical excision [15].
The alimentary tract duplications diagnosed antenatally can be observed initially and excised later on at an optimum time electively but those who present with symptoms needs urgent intervention. The duplication cyst is better treated as theta are prone to complications such as obstruction, infection, rupture, pressure symptoms and pain, development of cancer at later date, etc.
The literature describes multiple approaches to these benign lesions including: endoscopic mucosal resection, laparoscopic excision, minimal invasive periumbilical approach, partial excision and mucosal stripping, internal drainage, enucleation, resection with Heineke-Mikulicz type pyloroplasty, or even complete pyloroantrectomy with Billroth I reconstruction [19,20]. The majority of these cysts do not communicate with the lumen permitting partial excision of the cyst wall and decompression of the pylorus lumen. This allows the mucosal stripping or cauterisation at the same time leaving the common wall intact, antropyloric function is minimally affected as compared to pyloromyotomy or gastric resection and reconstruction allowing speedy and complete recovery [15].
Although our team has experience and expertise of performing laparoscopic neonatal gastric surgery [4], we prefer to give full account of the current evidence-based options with pros and cons of each of these options and allow the parents to take a final informed decision. We use balanced anesthesia in the form of rectal paracetamol, local anesthesia at the periumbilical incision and laryngeal mask anesthesia which is similar to single port laparoscopic approach but is quick, safe and accurate and does not need endotracheal intubation and prolonged anesthesia.
Conclusion
We presented the unusual case of a congenital pyloric gastric duplication diagnosed prenatally with polyhydramnios and confirmed postnatally presenting as complete neonatal gastric outlet obstruction who subsequently had undergone minimal invasive total excision uneventfully. This case shows the importance of looking actively for any upper gastrointestinal obstruction in cases of polyhydramnios and tell-tale signs and signature of a duplication cyst of alimentary tract. Recent advances in prenatal diagnosis, perinatal care, high index of suspicion and quick work up of the case in the postnatal period with minimal invasive surgical approach is safe and effective which helped achieve successful outcome with quick and complete recovery.
Compliance with ethical standards:
Acknowledgments: We are grateful to Dr Jitendra G Govani, Primary Care Physician for referring the patient to us and Dr. Anil Kumar Trambadia MD, DCH and Dr Kavita Trambadia MD, DCH consultant pediatricians and monitoring the growth, development and follow up care.
Conflict of interest: The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval: All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from the parents and all the relatives involved prior to all the procedures. Parents and all involved parties were informed about the procedure.
References
- Patel RV, Sharma RK. Ultrasonic Prenatal Diagnosis. Gynecology & Obstetrics Update, 2000; 2(3): 37-43.
- Yadav K, Patel RV, Singh JM. Fetal Surgery - An experimental gastroschisis model in fetal rabbits. Ind Jr Surgery, 1987; 49(3,4): 118-125.
- Patel RV, Anthony FM, Govani ND, Govani DR, Panchasara N, Patel RR, et al. Abdominal Wall Defects and Hernias-lessons learnt from observations from the experimental fetal surgery gastroschisis model in rabbits and their clinical extrapolation. Medp Pediatr Child Health Care, 2022; 1(1): 8-15.
- Singal AK, Patel R, Jain S, Gavhane J, Kadam NN. Laparoscopic management of neonatal gastric volvulus: a case report and review of the literature. Eur J Pediatr Surg, 2009; 19(3): 191-193.
- Govani DR, Patel RR, Patel RV, Doshi S. Ileo-cecal Sphincteric Duplication-Total Cyst Excision with Ileo-cecal Valve Preservation. Austin J Clin Case Rep, 2014; 1(8): 2.
- Patel RV, Milliken I, Dick A, Marshall D. Infected transverse colonic cystic duplication simulating pelvic appendicular abscess. BMJ Case Reports, 2013. doi:10.1136/bcr-2013-201459.
- Patel RV, Brown LM, More B, Stewart R. Neonatal-perforated appendix forming antibioma masquerading as duodenal duplication. BMJ Case Rep, 2013. pii: bcr2013200067. doi: 10.1136/bcr-2013-200067.
- Lawther S, Patel RV, de la Hunt MN. Ileal duplication cyst associated with segmental ileal stenosis and neonatal perforation. J Ped Surg Case Reports, 2013; 1: 8e10.
- Vietan D, Patel R, Huddart S. Duplicated Proctodeum. Pediatr Surg Int, 2009; 25(6): 535-536.
- Mehta MH, Mehta SG, Trivedi PS, Patel RV. Pararectal duplication. Ind J Med Sc, 1992; 46: 83-85.
- Narasimharao KL, Patel RV, Malik AK, Mitra SK. Chronic perianal fistula: beware of rectal duplication. Postgrad Med J, 1987; 63: 213-214.
- Yadav K, Nayar PM, Patel RV, Das GC. Caecal duplication cyst presenting as an intussusception in an infant. J Ind M A, 1987; 85(2): 57-58.
- Mărginean CO, Mărginean C, Horváth E, Gozar L, Gozar HG. Antenatally diagnosed congenital pyloric duplication associated with intraluminal pyloric cyst – Rare entity case report and review of the literature. Romanian Journal of Morphology and Embryology, 2014; 55(3): 983-988.
- Grosfeld JL, Boles Jr ET, Reiner C. Duplication of pylorus in the newborn: a rare cause of gastric outlet obstruction. J Pediatr Surg, 1970; 5(3): 365-369.
- Delaplain PT, Gholizadeh M, Reyna T. Minimally invasive approach to non-communicating pyloric duplication. Journal of Pediatric Surgery Case Reports, 2018; 37(10): 19-23. https://doi.org/10.1016/j.epsc.2018.07.003
- Lammers D, Marenco C, Do W, Barlow M. Pyloric duplication cyst with associated hypertrophic stenosis: A potential causal relationship. Journal of Pediatric Surgery Case Reports, 2020; 57(6): 101467. https://doi.org/10.1016/j.epsc.2020.101467
- Hérin E, Sauvanet A, Cros J, Koulakian H, Levy P, Vullierme M. Recurrent acute pancreatitis caused by combined gastric and pancreatic duplications: value of preoperative CT and MRCP and conservative surgery. J Surg Case Rep, 2020; 8: 1–5. doi: 10.1093/jscr/rjaa175.
- Lyu X, Pang X, Wu L, Wang L. Diagnosis of gastric duplication cysts in a child by endoscopic ultrasonography. Chin Med J, 2019; 132: 488–490. doi: 10.1097/CM9.0000000000000077.
- Liu F, Xu X, Lan M, Tao B, Liang Z, Zeng J. Clinical Characteristics of Gastric Duplication in Children. Front. Pediatr, 2022; 10: 857056. doi: 10.3389/fped.2022.857056.
- Kim GH, Lee MW, Lee BE, Park DY. Endoscopic submucosal dissection for gastric duplication cyst with heterotopic pancreas. Endoscopy, 2021; 53: E19. doi: 10.1055/a-1173-7326.

