Primitive Neuroectodermal Tumor of Axilla
Rabileh Madina*, Sidki Kenza, Lanjerie Safae, Insumbo Paulino, Saleheddine Tariq and El Fenni Jamal
Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Received Date: 31/07/2024; Published Date: 18/10/2024
*Corresponding author: Rabileh Madina, Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Abstract
Primitive neuroectodermal tumors (PNETs) are poorly differentiated small round cell neoplasms. They are commonly observed in children and are rare in adults, and are often aggressive. PNETs are quite rare, with the incidence of PNET in the axilla being extremely rare, and very few cases have been reported due to their rarity in the literature.
We report the case of a 68-year-old male patient who presented with a right axillary mass. A cervical and thoracic scanner was performed revealing a lesional process centered on the right axillary hollow and the pectoralis minor muscle, following a wide local excision of this axillary mass, an attack of axillary primitive neuroectodermal tumor was diagnosed after the histopathological examination.
Keywords: Axilla Neuroectodermal Tumors; Differential diagnosis
Introduction
Peripheral primitive neuroectodermal tumors (PNETs) represent rare malignant neoplasms, primarily seen in extraskeletal and soft tissues, and most commonly manifest during childhood or adolescence. Pathologically, PNETs belong to the category of small round cell sarcomas, characterized by neuroectodermal differentiation [1]. The incidence of PNETs is 1% of all sarcomas, and they exhibit very aggressive biological behavior as well as an unfavorable prognosis [2]. ESFT encompasses Ewing's Sarcoma of bone, Extraosseous Ewing's Sarcoma (ESS), Askin tumor, and PNET. Ewing's Sarcoma (ES) and PNET exhibit similar chromosomal translocation characteristics involving chromosomes 11 and 22 (11;22), along with comparable clinical features, cellular molecular traits, prognoses, and a strong expression of Cluster of Differentiation 99 (CD99), differing mainly in the degree of neural differentiation [3]. The most frequently observed location for extra-skeletal ES/PNET is within the deep soft tissues, with only a few documented cases of primary cutaneous ES /PNETs [4]. Differential diagnosis includes other types of ESFT and other small round blue cell tumors. The treatment strategy involves multiple modalities including surgery, chemotherapy, and radiation therapy. For localized disease, the standard care is surgical intervention, which may be followed by additional chemotherapy and radiation therapy. We report a case of 68-year-old male patient diagnosed with a Primitive Neuroendocrine Tumor (PNET) in the right axilla, who was treated using a multimodal approach.
Case Report
A 68-year-old patient with no personal or family medical history presented with a progressively increasing, painful right axillary swelling accompanied by local inflammatory signs, along with tingling and numbness in the fingers of the hand. This condition has been evolving in the context of a general decline in health over the past eight months.
A Thoraco-Abdominopelvic (TAP) scan was performed, revealing a lesion process centered on the right axillary area and the pectoralis minor muscle, characterized by heterogeneous tissue density enhancement following contrast agent injection, measuring 109 x 103 x 125 mm. This process extends into the intercostoclavicular space and reaches the cervical base, respecting the thoracic cage without any underlying bone lysis Figure 1. Additionally, multiple bilateral micronodular and parenchymal pulmonary lesions of random distribution, suggestive of secondary origins, were also noted (Figure 2).
18FDG PET CT Scan showed a hypermetabolic multiple discrete right axilla level I nodes with increased vascularity in the right anterior chest wall and axilla, mildly hypermetabolic right axillary level III and right internal mammary lymph nodes, with bilateral hypermetabolic pulmonary nodules. The patient underwent wide local excision, Immunohistochemistry (IHC) was positive for CD99, Chromogranin, and Synaptophysin and negative for Thyroid transcription factor 1 (TTF1) and Leucocyte common antigen (LCA). All these features were consistent with diagnosing a Primitive neuroendocrine tumor of the axillary lymph node. Given the contexts of pulmonary and lymph nod metastases, The patient was planned for salvage chemotherapy followed by radiotherapy sessions. Following the completion of radiation treatment,there was a lesional stability response with more than a 18% reduction in the tumor size,as evaluated by Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1].
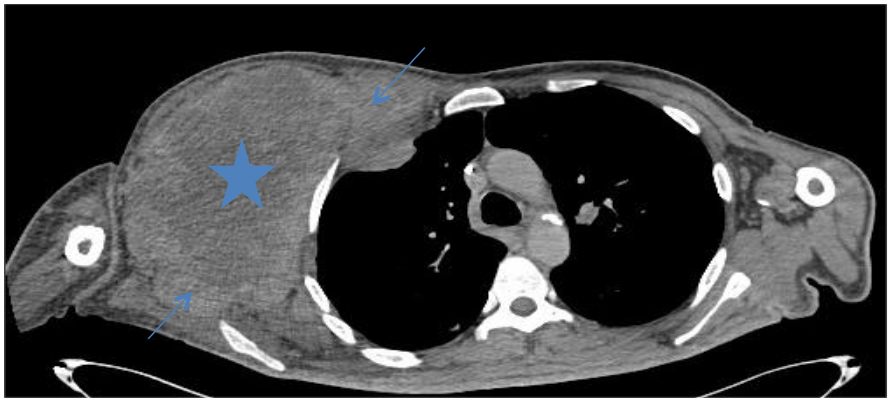
Figure 1: CT neck and thorax (axial ) shows a voluminous double-component lesion process solid (blue arrow) and cyst portion ((five-pointed star ),centered on the right axillary area and the pectoralis minor muscle, with an indistinct margin in the axillary region,characterized by heterogeneous tissue density enhancement following contrast agent injection.

Figure 2: CT thorax axial parenchymal window,we note a dense nodule with irregular contours located at the level of the apico-dorsal segment of the left upper lobe ( arrow), suspicious in appearance.
Discussion
PNET is a highly aggressive soft tissue sarcoma. The tumor is part of the Ewing sarcoma family and occurs most commonly in children, adolescents, and young adults (< 35 years old).4 PNET is widely diagnosed through clinically and histologically identical tumors comprised of small round blue cells; these cells are uncommon entities, accounting for 5% of all small round cell tumor cases [5]. PNET affecting bones and soft tissues of the limbs,They arise from the neuroectodermal elements, which probably develop from migrating embryonic cells of the neural crest [6]. These tumors have similar characteristic translocation [11,22] and express CD99 cell surface adhesive glycoprotein plays an essential role in diagnosing ES/PNET.But other tumors also express CD99. Thus, the differential diagnosis includes other members of ESFTs along with neuroendocrinecarcinoma, lymphoma, metaplastic carcinoma of the breast, and rhabdomyosarcoma [10]. PNETs arise outside the central and sympathetic nervous system, and their overall incidence accounts for 1% of all sarcomas. PNETs are commonly located in the soft tissues of the thoracopulmonary region (Askin tumor), paraspinal region, and limbs. Tumors originating in the intra-abdominal and retroperitoneal regions, head and neck regions and bone are relatively rare [7].
In imaging, PNET mostly shows mixed isointense to hypointense signals on T1-weighted imaging, and isointense to hyperintense signals on T2-weighted imaging. PNET may have heterogeneous enhancement on CT scan and significant enhancement on the MRI). It can be seen from our cases that the tumor density may appear uniform when it is small and the tumor may appear heterogeneous when it is large in size. PNETs generally do not have clear boundary with its adjacent organs or tissues suggesting their invasive nature. It may be a diagnostic valuable sign when maximum intensity projection reconstruction image demonstrates tortuous blood vessels within the tumor on enhanced CT images.On ultrasound, these tumors present a heterogeneous hypoechoic appearance with cystic areas [9]. Imaging also makes it possible to assess the measurements of the tumor, the locoregional extension, the presence of metastases and the evaluation of the tumor response. Metastases are frequently found during the initial diagnosis as in the case of our patient and are located in descending order at the lung (50%), bone (25%), marrow (20%), liver and brain.
According to the National comprehensive Cancer Network (NCCN) guideline, the treatment plan for all members of ESFT is the same. It includes a multimodality approach consisting of local treatment (surgery and radiation therapy) and chemotherapy [8]. As these tumors have a high tendency for distant metastasis, they should be treated with multiagent systemic chemotherapy to control the micrometastases and improve overall survival. The good prognosis of ES/PNETs depends on their early diagnosis, with the prognosis of metastatic disease being dismal.
Conclusion
Primitive neuroectodermal tumors (PNETs) are rare tumors constituting only 1% of all sarcomas, with PNETs of the axilla in an adult being extremely rare. Generally, the imaging appearances of PNET lack characteristics. When the tumor is small its density may appear uniform and it tends to become heterogeneous when the tumor is large. PNETs generally do not have clear boundary, or partially so, with its adjacent organs or tissues suggesting their invasive nature. Upon further validation, maximum intensity projection image reconstruction demonstrates tortuous blood vessels within the tumor on enhanced CT images may be valuable information for diagnosis of PNET. The confirmation is essentially anatomo-pathological.
References
- Friedrichs N, Vorreuther R, Poremba C, Schafer KL, Böcking A, Buettner R, et al. Primitive Neuroectodermal Tumor (PNET) in the differential diagnosis of malignant kidney tumors. Pathology-Research and Practice, 2002; 198(8): 563-569. https://doi.org/10.1078/0344-0338-00303.
- Tsokos M, Alaggio RD, Dehner LP, Dickman PS. Ewing sarcoma/peripheral primitive neuroectodermal tumor and related tumors. Pediatric and developmental pathology, 2012; 15(1_suppl): 108-126. https://doi.org/10.2350/11-08-1078-PB.1.
- Carvajal R, Meyers P. Ewing's sarcoma and primitive neuroectodermal family of tumors. Hematology/Oncology Clinics, 2005; 19(3): 501-525. https://doi.org/10.1016/j.hoc.2005.03.004.
- Delaplace M, Lhommet C, De Pinieux G, Vergier B, De Muret A, Machet L. Primary cutaneous Ewing sarcoma: a systematic review focused on treatment and outcome. British Journal of Dermatology, 2012; 166(4): 721-726. https://doi.org/10.1111/j.1365-2133.2011.10743.x.
- Hameed M. Small round cell tumors of bone. Arch Pathol Lab Med, 2007; 131(2): 192–204. doi:10.1043/1543-2165.
- Dehner LP. Primitive neuroectodermal tumor and Ewing's sarcoma. TheAmerican journal of surgical pathology, 1993; 17(1): 1-13.
- Carvajal R, Meyers P. Ewing's sarcoma and primitive neuroectodermal family of tumors. Hematol Oncol Clin North Am, 2005; 19: 501–525, vi. 10.1016/j.hoc.2005.03.004
- Shravan S. Primitive Neuroectodermal Tumor of Axilla in an Adult: A Rare Entity. Journal of Clinical Case Studies Reviews & Reports, 2021; 3(2): 1-2.
- O Keeffe F, Lorigan JG, Wallace S. Radiological features of extraskeletal Ewing sarcoma. Br J Radiol, 1990; 63(750): 456–460.
- Milanezi F, Pereira EM, Ferreira FV, Leitao D, Schmitt FC. CD99/MIC‐2 surface protein expression in breast carcinomas. Histopathology, 2001; 39(6): 578-583. https://doi.org/10.1046/j.1365-2559.2001.01309.x.
- Gachechiladze M, Skarda J, Ibrahim M, et al. Primitive neuroectodermal tumor (PNET) of the lung in an adult woman. World J Surg Oncol, 2014; 12: 374. doi:10.1186/1477-7819-12-374.

