A Rare Case of Basal Cell Carcinoma in a Non-Sun-Exposed Area
Hafsa El Boukili*, Sara Elloudi, Zakia Douhi, Meriem Soughi, Hanane Baybay and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Morocco
Received Date: 16/07/2024; Published Date: 16/10/2024
*Corresponding author: Hafsa EL BOUKILI, Department of Dermatology, University Hospital Hassan II , Faculty of Medicine and Pharmacy, Sidi Mohamed Ben Abdellah University, Fez, Morocco
Abstract
Basal Cell Carcinoma (BCC) is the most common cutaneous malignancy, accounting for approximately 80% of all non-melanoma skin cancers. BCCs typically develop on sun-exposed areas, with around 85% of reported cases occurring on the head or neck. However, BCC can also arise in non-sun-exposed areas such as the axilla, nipple, genital and perianal regions. This report describes a rare case of BCC originating from an unusual site, emphasizing the importance of biopsying all suspicious lesions.
Keywords: Basal Cell Carcinoma; Unsual sites; Non sun-exposed
Introduction
Basal Cell Carcinoma (BCC) is the most common cutaneous malignancy and accounts for approximately 80% of all nonmelanoma [1].
BCC is caused by various factors including exposure to excessive actinic, ionizing and, ultraviolet (UV) radiation and these are accepted as most important causal factors. BCC affects more often areas exposed to sunlight, but it may occur in covered areas and rare sites, hindering early diagnosis and treatment.
Hence, we report a case of BCC in a female patient, arising in a non-sun-exposed area such that BCC is kept as a differential in a chronic nonhealing lesion even if it arises in atypical sites in atypical populations.
Observation
A 52-year-old patient, 38 years old woman presented with a lesion in the back of left thigh for the last 3 years. No history of past trauma, radiation exposure or damage, at the site of lesion. She first noticed a small raised lesion in the right flank, 3 years ago which was not symptomatic and did not trouble her and hence she did not consult a physician for the same. She has noted that the lesion has grown larger over the previous one to two years, and that dressing or rubbing against the lesion causes a minor amount of pain and discomfort. Cutaneous examination revealed a well demarcated exophytic pearl-shaped tumor with telangiectasie on the surface and periphery, with a subcutaneous component, measuring about 5cm (Figure 1). On palpation it was not tender and moved freely from underlying structures.

Figure 1: A pearl-shaped tumor with a subcutaneous component, and telangiectasie on the surface measuring about 4cm in the right flank.
On dermoscopy: Blue gray Ovoid nests, and arborizing vessels were seen (Figure 2).
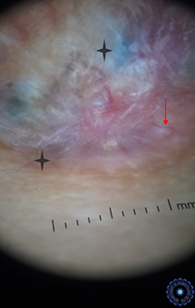
Figure 2: Blue gray Ovoid nests (black star) , and arborizing vessels (Red arrow).
Excision with 1cm free margins was indicated and the specimen was sent for histopathological examination. The biopsy result showed a Basal cell carcinoma, nodular variant with all peripheral margins (Superior, Lateral, Inferior, Medial, and Basal) being microscopically free from tumor. Tumor was 5mm away from the nearest superior margin.
Discussion
Nodular basal cell carcinoma comprises about 60-80% of the cases and occurs most often on the skin of the head. Clinically it is presented by elevated, exophytic pearl-shaped nodules with telangiectasia on the surface and periphery [2]; Besides ultraviolet radiation there are other exogenous carcinogens such as exposure to chemical carcinogens, and possibly infection with human papilloma viruses, ethnical differences, type of skin, chronic irritation, chronic inflammation, burns, skin lesions, immunologic, and genetic factors [3,4]. Although these cancers rarely metastasize, basal cell carcinomas can invade nearby structures. Therefore, early recognition is critical to optimize outcomes [5]. These tumors typically arise in sun-exposed areas, in about 80% of patients it appears in the head, and in half of them affects the skin of cheeks and the nose [2]; rarely, they occur in nonexposed areas and have been found on the trunk, genitals, nails, axilla, nipple, or sole of the foot [6,7].
Defining unusual locations for BCC remains a subject of controversy in the literature. Arbitrary criteria have been established, considering factors such as percentage incidence, previously identified unusual locations [8].
However, these criteria are imprecise, relying on subjective, there is generally consensus on certain locations being considered unusual for BCC, including the breasts, periungual region, palms, soles, glutei, and intertriginous areas like the axilla, groin, and genitals [9].
The factors determining the anatomical distribution pattern of BCC remain unclear. Despite the common association of BCC with sun-exposed sites, up to one-third of cases occur in unexposed areas. Additionally, BCC is rare on the forearms, hands, and lower limbs, despite significant sun exposure. The occurrence of BCC on the lower limbs is three times higher in women than in men, possibly due to increased sun exposure.
Concerning the association of tumor location with histological subtypes, studies indicate that unexposed areas like the trunk and limbs predominantly exhibit a superficial pattern. In contrast, sun-exposed areas like the nose, neck, and head mainly display a nodular pattern. The sclerodermiform pattern is not significantly associated with any specific body site, suggesting its appearance may be unrelated to external factors, despite the predominance of some subtypes in specific areas potentially being explained by local predisposing conditions, such as sun exposure [10,11].
In our knowledge, the case of our patient is the first described instance of having a nodular histological type in a non-photoexposed site, which is the back.
Conclusion
The case report of this instance of BCC, nodular type, that showed up in an unusual location (the right flank) emphasizes the need for dermatologists to remember that basal cell carcinoma can be diagnosed in such lesions that appear in atypical areas and in non-sun-exposed areas of skin.
Regardless of the method employed to categorize locations as unusual for BCC, it is crucial to acknowledge and report instances in uncommon sites. This approach is essential for advancing our understanding of the pathogenesis, diagnostic criteria, therapeutic approaches, and prognosis of BCC occurring in atypical locations.
References
- Sheikh Manzoor, Seerat Fatima, Rinchan Angmo Ayushi. A Rare Case of Basal Cell Carcinoma in a Non-Sun-Exposed Area: Case Report, 2023.
- Dourmishev A, Popova L, Dourmishev L. Basal‑cell carcinoma and squamous‑cell carcinomas: Epidemiology, location and radiotherapy.
- Pfister H, Ter Schegget J. Role of HPV in cutaneous premalignant and malignant tumors Clin Dermatol, 1997; 15: 335-47.
- Crowson AN. Basal cell carcinoma: Biology, morphology and clinical implications. Modern Pathology, 2006; 19: 127-147.
- Audrey V Carr, Edward Feller, Fouad R Zakka, et al. A Case Report of Basal Cell Carcinoma in a NonSun-Exposed Area: A Rare Presentation Mimicking Recurrent Perianal Abscess: Hindawi Case Reports in Surgery, 2018; 9021289: 5.
- Betti R, Bruscagin C, Inselvini E, Crosti C. Basal cell carcinomas of covered and unusual sites of the body. 4 Case Reports in Surgery International Journal of Dermatology, 1997; 36: 503–505.
- Roth MJ, Stern JB, Haupt HM, Smith RRL, Berlin SJ. Basal cell carcinoma of the sole. Journal of Cutaneous Pathology, 1995; 22: 349–353.
- Betti R, Martino P, Moneghini L, Vergani R, Tolomio E, Crosti C. Basal cell carcinomas of the areola-nipple complex: case reports and review of the literature. J Dermatol, 2003; 30: 822-826.
- Betti R, Bruscagin C, Inselvini E, Crosti C. Basal cell carcinomas of covered and unusual sites of the body. Int J Dermatol, 1997; 36: 503-505.
- Ane Beatriz, Mautari Niwa, Eugênio R. A. Pimentel. Basal cell carcinoma in unusual locations. An Bras Dermatol, 2006; 81(5 Supl 3): S281-284.

