Isolated Sacral Tuberculosis
Rabileh Madina*, Wen-yam Traoré, Sidki Kenza, Insumbo Paulino, Lanjerie Safae, Saleheddine Tariq, Edderai Meryem and El Fenni Jamal
Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Received Date: 24/07/2024; Published Date: 15/10/2024
*Corresponding author: Rabileh Madina, Department of Radiology, Mohammed V of the Military Hospital, Rabat, Morocco
Abstract
Tuberculosis remains one of the most common infectious diseases worldwide. Spinal tuberculosis is a fairly common form of osteoarticular tuberculosis. However, isolated sacral tuberculosis is rare. Rapid diagnosis and early treatment of the disease will reduce the risk of developing complications. We report a case of sacral tuberculosis diagnosed in a 62-year-old man who was hospitalized for progressive sciatica of the left leg for six months. The patient had no history of active tuberculosis, no fever and no weight loss without change in general condition. Physical examination reveals a painless mass, located in the lower lumbar region on the left side and neurological examination of which reveals no motor or sensory deficits. There is no intestinal or urinary incontinence. The study of Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) of the lumbosacral spine revealed a large osteolytic lesion centered on the sacrum and the left iliac wing with cortical rupture in places fusing towards the pre and soft tissues adjacent retrosacrals . The patient underwent a sacral biopsy under guided ultrasound and the diagnosis of tuberculosis was confirmed by histology. The evolution was satisfactory with the addition of anti-tuberculosis chemotherapy.
Introduction
Tuberculosis (TB) is an infectious disease caused by the transmission of the Mycobacterium tuberculosis bacillary complex, which usually affects multiple systems if not recognized and treated in time. Tuberculosis can affect all bone and joint structures in the body. Osteoarticular tuberculosis (OAT) accounts for 2–5% of all TB cases and 11–15% of extrapulmonary tuberculosis [1]. The principal location of the OAT is the spinal cord, which represents approximately 50% of cases affecting more often dorsolumbar vertebrae [2]. Isolated tuberculosis of the sacrum is rarely reported in the literature, which leads to a delay in diagnosis and subsequently persistence of a normally curable disease. The involvement of the spine in the case of TB generally occurs after the haematogenous spread of the bacteria from a primary region, usually the lungs. The spread occurs through the anterior part of the vertebral bodies, or may involve the central portion of the vertebrae by communicating through the valveless venous plexus or the Batson plexus [1] Patients usually present with fever, night sweats, pain in the lower region of the back radiating to the legs, and weight loss.1 X-ray is usually the primary imaging modality, while MRI of the spine is more specific. Biochemical and microbiological analysis of the biopsy or aspirate confirms the diagnosis [2]. It is pharmacologically treated by anti-tubercular therapy, supplemented by surgical management if the spread leads to physical deformities or complications [1,2]. In the wide spectrum of spinal TB, isolation to the sacrum is a rare presentation. Amongst various sacral pathologies diagnosed on imaging, TB of the sacrum is one of the rare conditions that need adequate clinical, biochemical, and microbiological analysis to be ruled as the disease, which is why the authors believe a thorough review of the same is necessary. It is pharmacologically treated by anti-tubercular therapy, supplemented by surgical management if the spread leads to physical deformities or complications [1,2].
Case Report
A 62-year-old man who was hospitalized for progressive sciatica of the left leg for six months. The patient had no history of active tuberculosis, no fever and no weight loss without change in general condition. Physical examination reveals a painless mass, located in the lower lumbar region on the left side and neurological examination of which reveals no motor or sensory deficits. There is no intestinal or urinary incontinence. Laboratory tests showed an ESR at 90 mm at the first hour and C-Reactive Protein (CRP) at 45 mg/L. Other biologic parameters were normal. The study of computed tomography (CT) of the lumbosacral spine revealed a large osteolytic lesion centered on the sacrum and the left iliac wing with significant bone destruction associated with several rounded hypodense masses with regular contours annular enhancement after injection of the PDC, filling the presacral space and infiltrating the mesorectum and the left piriformis muscle fusing towards the pre and soft tissues adjacent retrosacrals containing a few air bubbles (Figure 1). Magnetic resonance imaging (MRI) showed the presence osteolytic lesion process centered on the sacrum and left iliac wing , intervertebral disc of L5-S1 was intact with normal lumbar vertebrae. Lesion showed low intense signal on T1-weighted images and hyperintense signal on T2-weighted images (Figure 2), peripherally enhanced with gadolinium with T1 fat saturation ,this lesion extends posteriorly towards the left middle gluteal muscle and anteriorly towards the ileo-psoas muscle containing areas of to abscessed accumulations contiguous low intense signal on T1-weighted images and hyperintense signal on T2-weighted images with typical more intense thin rim of peripheral enhancement .Finding were suggestive of a mitotic bony lesion; chordoma; Ewing sarcoma; tuberculosis , evoking in the first place an infectious origin (sacral tuberculosis) . Serum laboratory testing showed a higher level of Erythrocyte Sedimentation Rate (ESR) ranged up to 35 mm/hr with C-Reactive Protein (CRP) level at 6.3 mg/l. The other hematological and biochemical parameters were normal. The patient had a needle aspiration of the mass performed through ultrasound-guided biopsy. The pathological examination of the specimen revealed the presence of an epithelioid granuloma accompanied by caseous necrosis, indicating a possible tuberculosis infection. The GeneXpert test returned positive results. Antibacillary chemotherapy, consisting of Isoniazid, Rifampicin, Ethambutol, and Pyrazinamide, was initiated for a duration of one year. The patient showed full recovery from signs and symptoms after three months. Follow-up outpatient visits occurred at the 9-month and 12-month marks, with no reported complaints.
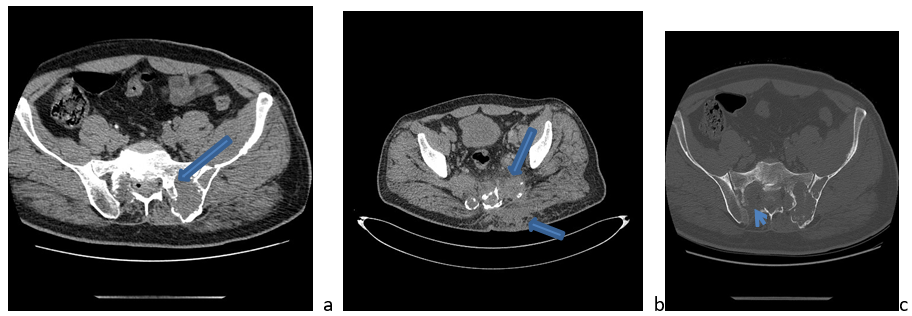
Figure 1: Axial CT scan of the pelvis in parenchymal window (a, b) objective a large osteolytic lesion centered on the sacrum and the left iliac wing associated with several rounded hypodense masses with regular contours fusing towards the adjacent pre and retrosacral soft tissues(blue arrow). (c) Axial CT scan of the pelvis in bone window setting shows osteolytic lesion with significant bone destruction with cortical rupture in places (arrow head).
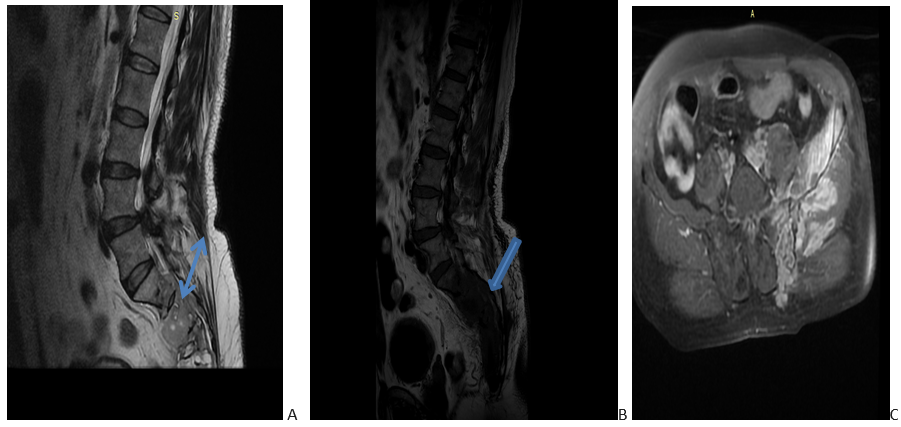
Figure 2: A) sagittal MRI lumbosacral showed the presence osteolytic lesion process centered on the sacrum and left iliac wing , inter vertebral disc of L5-S1 was intact with normal lumbar vertebrae , a high intense sacral mass lesion on T2-weighted imaging (double arrow). B) Sagittal MRI lumbosacral showed a lot intense sacral mass lesion on T1-weighted imaging (full arrow). C) Gadolinium enhanced MR imaging T1 fat saturation imaging showed a mixed-intense sacral and parasacral mass lesion, intraspongy formations of mixed intensity with peripheral enhancement, which correspond to abscesses.
Discussion
Tuberculosis continues to be a prevalent infectious disease in developing countries. This study indicated that isolated sacral tuberculosis predominantly affects young adults, with an average age of 37.6 years (ranging from 20 to 72). Notably, females are the most impacted group, accounting for 70% of the case [4].
Tuberculosis continues to cause significant morbidity and mortality, despite universal access to effective multidrug chemotherapy. The emergence of multidrug-resistant mycobacteria, coupled with a global rise in HIV infections, has led to a recent increase in the number of tuberculosis cases. This health issue remains one of the most urgent priorities in developing countries. Spinal tuberculosis presents several atypical characteristics, including isolated vertebral infection, skip lesions, involvement of neural arch, and unusual sacral lesions [4,8].
The sacrum and cervical spine are uncommon locations for spinal tuberculosis. This condition is almost always the result of hematogenous dissemination of mycobacteria from primary sites in the lungs and/or urogenital tract. The paravertebral venous plexus of Batson is typically regarded as the primary pathway for the spread of tuberculosis bacilli into the spine. Additionally, it is possible that lymphatic drainage from the pleura or kidneys influences the para-aortic lymph nodes, which may subsequently impact the vertebrae [4-7].
Clinical manifestations of sacral tuberculosis depend partly on the age of the patient. As noted by Pun et al and evident in our series, young individuals tend topresent with discharging sinuses and abscesses while backache and sciatic pain are a dominant clinical feature in adults [4,9]. Neurological symptoms occur infrequently in sacral tuberculosis because the sacral nerve roots are shielded by bone.
During laboratory tests, patients typically exhibit an elevated erythrocyte sedimentation rate and high levels of C-reactive protein due to the underlying infectious pathology. Additionally, leukocytosis may or may not be present in the patient, as noted by the authors. For instance, Chang et al. reported a case of sacral tuberculosis mimicking a neoplasm, with elevated carbohydrate antigen 19-9 levels. A chest X-ray is mandatory in all cases of sacral tuberculosis to rule out pulmonary tuberculosis.
An initial diagnosis can be made using an X-ray of the spinal region, but the definitive diagnosis and the extent of the disease are better understood through an MRI of the spinal region, as MRI is more sensitive than an X-ray of the spine and more specific than a CT scan of the same area.
MRI is considered the most sensitive technique for the early detection and complete differentiation of the disease. In cases of sacral tuberculosis, the radiological features of the mass lesion typically show low intensity on T1-weighted images and high intensity on T2-weighted images. Additionally, there is often an associated parasacral abscess. These findings align with the results reported by Patankar et al. [4]. Sacral tuberculosis is marked by the replacement of the normally bright sacral marrow, appearing hypointense on T1-weighted MRI images. The hyperintensity observed on T2-weighted images is likely due to marrow edema [4,5]. Using gadolinium-enhanced MRI with fat saturation is considered the most sensitive approach for diagnosing sacral tuberculosis. This technique strongly indicates isolated sacral tuberculosis when it reveals intraspongy formations of mixed intensity with peripheral enhancement in the vertebral bodies, which correspond to abscesses
MR imaging also provided us with an accurate depiction of the presacral abscess, its extension under the anterior longitudinal ligament and differentiation from a pyo-genic abscess due to its circumscribed nature [11]. Incontradistinction to pyogenic abscesses, which frequently transgress the ligaments to enter the retroperitoneum [10].
This examination is very useful in planning the diagnostic and therapeutic procedure in this type of pathology. As radiological characteristics of sacral tuberculosis may be confused with neoplasms diseases, fresh tissue should be collected for culture and biopsy.
The diagnosis of tuberculosis is confirmed by tissue aspiration and histopathological analysis of the tissue, showing the presence of a tuberculous granuloma, central caseous necrosis surrounded by epithelioid cells and giant cells of the Langhans type also by the culture of Lowenstein Jensen and PCR, revealing acid-fast bacilli and Mycobacterium TB in the lesion [10,11].
Adequate treatment for sacral TB includes primary therapy ATT, consisting of isoniazid, rifampin, pyrazinamide, and ethambutol. The World Health Organization (WHO) recommends ATT for a period of 9 months for patients who have TB in bones and joints, [13] while the American Thoracic Society (ATS) recommends ATT for 12 months for children and 6 months for adults [14]. The duration of ATT can vary depending on the local guidelines, as well as the severity of the disease.
Without early diagnosis and appropriate treatment, complications can occur, including structural and postural deformities, permanent neurological damage, and spread of the disease to adjacent structures, which can lead to the formation of cold abscesses in the gluteal and piriformis muscles. Surgical intervention may be necessary in patients with structural complications, such as bone failure, abscesses, and spinal deformities.
Conclusion
Sacrum in isolation is a rare location for spinal TB, often overlooked by primary physicians, athough it is uncommon, it is important to suspect this condition in patients with chronic lower back pain or in children who present with sinus discharge and abscesses. The use of magnetic resonance imaging aids in recognizing this pathology and allows for the rapid initiation of antituberculous chemotherapy treatment. A prompt diagnosis and early treatment of the disease will mitigate the risk of developing complications.
References
- Pertuiset E. Tuberculose osseuse et articulaire périphérique. EMC-Rhumatologie Orthopédie, 2004; 1: 463–486. http://dx.doi.org/10.1016/j.emcrho.2004.08.00.
- Shantanu K, Sharma V, Kumar S, Jain S. Tuberculose du sacrum imitant une tumeur maligne. BMJ Case Rep, 2012; 2012: bcr0720114505.
- Patankar T, Krishnan A, Patkar D, Kale H, Prasad S, Shah J, et al. Imaging in isolated sacral tuberculosis: a review of 15 casesSkeletal, 2000; 29(7): pp. 392-396.
- Osman W, Braiki M, Alaya Z, Mouelhi T, Nawar N, Ben Ayeche M. A Rare Case of Tuberculosis with Sacrococcygeal Involvement Miming a Neoplasm Case Rep. Orthop, 2016; 2016: pp. 1-5.
- Pertuiset E, Beaudreuil J, Lioté F, Horusitzky A, Kemiche F, Richette P, et al. Kuntz Spinal tuberculosis in adults: a study of 103 cases in a developed country, 1980–1994.
- Sament R, Bachhal V, Gopinathan NR. Sen Isolated tuberculosis of sacrum with monoparesis: an atypical presentation Asian Spine Journal, 2013; 7(4): p. 351.
- Naim-Ur-Rahman, El-Bakry A, Jamjoom A, Jamjoom ZA, Kolawole TM. Atypical forms of spinal tuberculosis: case report and review of the literature. Surg Neurol, 1999; 51: 602–607.
- Pun WK, Chow SP, Luk KDK, Cheng CL, Hsu LCS, Leong JCY. Tuberculosis s of the lumbosacral junction: long-term follow-up of 26 cases. J Bone Joint Surg Br, 1990; 72: 675–678.
- Desai SS. Early diagnosis of spinal tu-berculosis by MRI. J Bone Joint SurgBr, 1994; 76: 863–869.
- Huang YH, et al. Polymerase chain reaction as the sole diagnostic tool for sacral-spinal tuberculosis. Surg Infect (Larchmt), 2013; 14(2): 225-228.
- Khanna K, Sabharwal S. Spinal tuberculosis: a comprehensive review for the modern spine surgeon. Spine J, 2019; 19(11): 1858-1870.
- World Health Organization (WHO). Treatment of tuberculosis guidelines, fourth edition, 2010.
- Bass JB Jr, et al. Treatment of tuberculosis and tuberculosis infection in adults and children. American Thoracic Society and the Centers for Disease Control and Prevention. Am J Respir Crit Care Med, 1994; 149(5): 1359-1374.

